Presentation
A 77-year-old Asian female presented for evaluation of an empty left orbit after a motor vehicle accident. She was the restrained driver in a one-vehicle crash, traveling at 75 miles per hour, during which the airbag deployed. Immediately after the accident, she reported a loss of vision in the left eye. At an outside hospital, she was noted to have a left-sided inferior and medial wall orbital fracture with herniation of the globe into the maxillary sinus. She had no other systemic trauma and no intracranial trauma.
History
Past ocular history included cataract surgery with posterior chamber intraocular lens placement in both eyes. Past medical history disclosed osteoporosis, gastroesophageal reflux disease and leukocytoclastic vasculitis. Family history was unremarkable. In terms of social history, the patient lived alone and had never smoked. She didn’t have known drug allergies. Current medications included omeprazole and alendronate.
 |
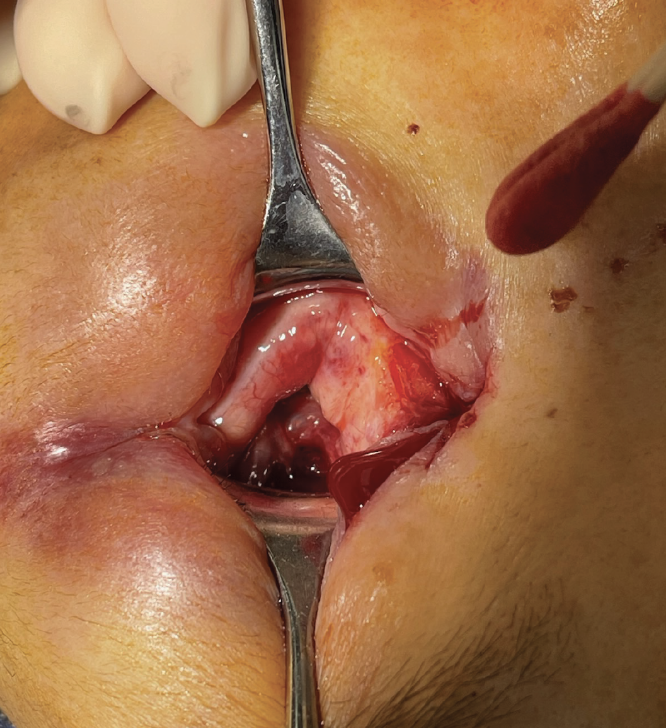
| Figure 1. CT scan of the orbits demonstrates herniation of the left globe into the left maxillary sinus with possible impingement of the lateral orbital floor on the globe. |
Examination
 |
| Figure 2. Preoperative photograph demonstrating herniation of the globe into the maxillary sinus. |
The patient’s vital signs were within normal limits. There was no evidence of acute or chronic injury to the chest, abdomen, pelvis, extremities or neck. Ocular examination demonstrated best-corrected visual acuity of 20/20 in the right eye and no light perception in the left eye, which was noted to be displaced inferiorly into the maxillary sinus. Multiple attempts were unsuccessfully made to establish potential light perception in the left eye, including transillumination into the region of the herniated globe. Ishihara color plates were 8/8 on the right eye. The pupil was round and reactive on the right. Intraocular pressure was 16 mmHg in the right eye. Confrontational visual field was full in the right eye. Extraocular motility was full for the right eye. The anterior segment examination was remarkable for a well-positioned PCIOL in the right eye. Dilated fundus examination was notable for a cup-to-disc ratio of 0.55 in the right eye. The left upper lid and left lower lid were notable for multiple lid lacerations. No globe was visible on careful examination of the left orbit with Desmarres retractors. No examination of the eye itself could be performed for the left eye.
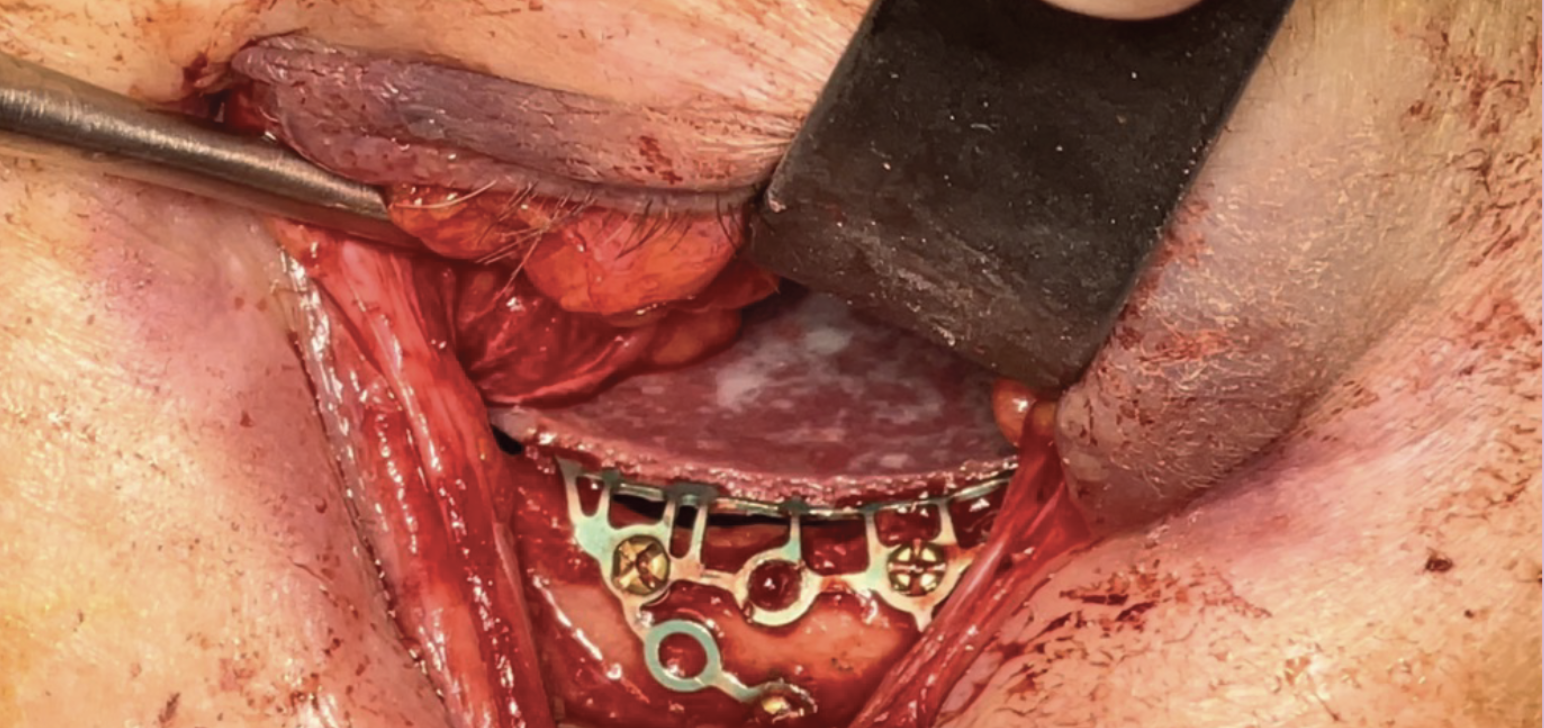 |
| Figure 3. Intraoperative photograph demonstrating placement of a porous, polyethylene-coated titanium implant for orbital floor repair. |
What’s your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
CT brain and orbits with and without contrast demonstrated a comminuted left-sided orbital floor fracture with herniation of the left globe into the left maxillary sinus (Figure 1). Although the left globe appeared symmetric in volume compared to the right globe, the lateral aspect of the orbital floor appeared to exert mass effect on the globe. Extensive orbital hematoma, as well as transection and retraction of all left-sided extraocular muscles were also noted. These findings confirmed that the patient had a traumatic globe dislocation into the maxillary sinus.
Subsequently, the patient was promptly taken to the operating room on the same day for surgical repair. Examination during the procedure confirmed that the globe and orbital contents had subluxed into the maxillary sinus, with nearly complete incarceration of the globe beneath the fractured left orbital floor (Figure 2). A transconjunctival approach was employed to access the orbital floor. Malleable retractors were used in a hand-over-hand fashion to carefully elevate the globe and orbital contents back into their proper position within the orbit. To repair the orbital fracture, a porous polyethylene-coated 3-D titan surgical implant was sized appropriately and securely attached to the inferior orbital rim with screws (Figure 3). Additional procedures included a left upper medial canthoplasty, repair of the left upper and lower eyelid lacerations, and a left lateral canthoplasty.
 |
|
Figure 4. Postoperative photograph demonstrating replacement of the globe into anatomical position. |
The initial examination of the left eye in the operating room revealed an IOP of 6 mmHg, a fixed and dilated pupil, a well-formed anterior chamber, a grossly normal optic nerve, and no apparent retinal lesions (Figure 4).
On the first postoperative day, the patient was noted to have hand motion vision on the left. By postoperative week three, the patient’s vision had improved to count fingers in the left eye. Examination in the clinic also disclosed a globe with minimal motility, a temporally subluxed posterior chamber intraocular lens capsular bag complex, and a fundus examination without signs of retinal detachment. At the two-month postoperative mark, the patient continued to have count fingers vision, as well as ptosis and motility deficits. This enophthalmos continued to progress during the three- and five-month postoperative visits, with 8 mm of enophthalmos observed at the final examination in our clinic (Figure 5). The patient was subsequently evaluated at an outside hospital and underwent a left orbital floor and medial wall fracture overlay using a custom implant. After this procedure, the patient was noted to have 20/40 vision, but still experienced complete left-sided movement deficits and no improvement in the residual enophthalmos.
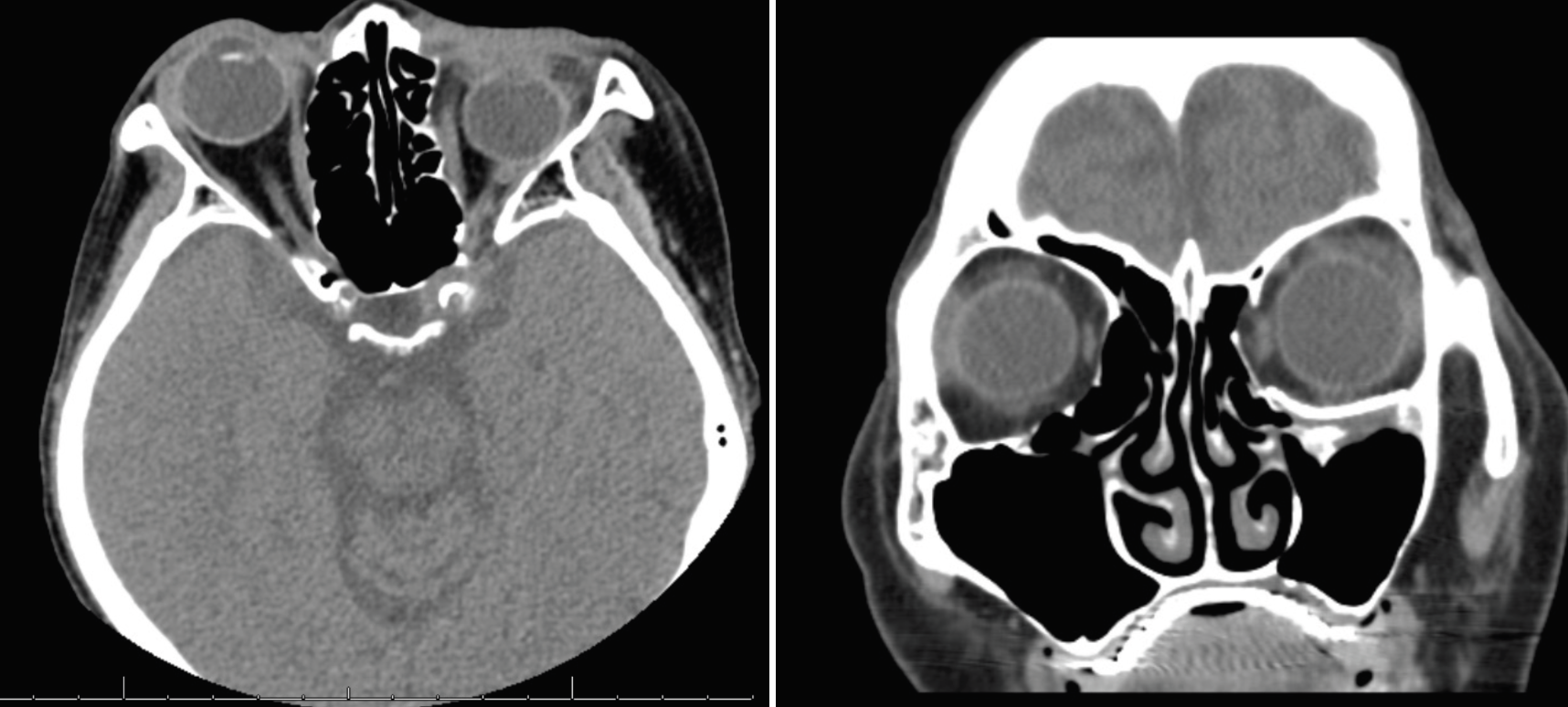 |
| Figure 5. CT scans of the orbit at postoperative month five demonstrate good position of the globe in the superior/inferior axis and marked enophthalmos of the left eye. |
Discussion
Traumatic globe dislocation into the paranasal sinuses is rare, with only 24 published cases in the English-language literature between 1971 and 2015.1 The primary causes of such dislocations are traffic accidents, accounting for 42 percent of cases, with other forms of blunt trauma being the second most common cause at 33 percent.1 Most of these dislocations occur into the maxillary sinus (87.5 percent), with a smaller proportion into the ethmoid sinus (12.5 percent).1
The mechanisms of such dislocations are thought to involve a combination of hydraulic and buckling mechanisms. The hydraulic mechanism theory states that blunt trauma initially occludes the orbital aperture, leading to an increase in intraorbital pressure. This, in turn, causes the orbital bones to fracture at their weakest point, typically along the posterior medial section of the orbital floor. Increased pressure can also lead to more extensive damage in other vulnerable areas of the orbit, such as the medial wall and the remaining inferior floor. On the other hand, the buckling mechanism theory proposes that direct pressure results in the deformation of the inferior orbital floor, ultimately leading to a blowout fracture of both the orbital floor and the medial wall.2,3 Of note, the globe is normally secured within the orbit by an intricate network of soft tissue support structures, including the Lockwood ligament, lateral and medial check ligaments, and orbital fat. Only in cases of severe trauma that disrupt both the soft tissue and bony anatomy can the globe experience herniation or
subluxation.4
A review of 31 cases in the literature found that 45 percent of them had vision at the level of counting fingers or better, while 39 percent had light perception or worse vision, and 16 percent didn’t report any visual outcomes.5 Additionally, this review showed that same-day repair was linked to better visual outcomes, with eight out of 14 patients who underwent same-day repair achieving a vision of 20/40 or better, whereas none of the seven patients who had delayed repair beyond the first day reached such visual acuity.5
Most authors agree that immediate globe repositioning is crucial. Delayed treatment can lead to increased edema and pressure on the optic nerve and central retinal artery, raising the risk of irreversible vision loss.2,6,7 Like our patient, other cases in the literature have demonstrated that individuals initially presenting as having no light perception ultimately achieved 20/40 vision or better. However, it should be noted that outcomes related to eye motility were generally unfavorable, with only three out of 31 cases reporting minimal impairment in extraocular movement. Late enophthalmos is another complication in these cases and is due to displacement of orbital soft tissue into the enlarged bony orbit, fat atrophy, scar contracture and fibrosis of extraocular muscles.8
In terms of surgical techniques, there are two primary approaches described for repositioning the dislocated globe: direct traction with the aid of an instrument3, 9, 10 and manual repositioning of the globe through a trans-maxillary approach.1,6 For this patient, direct traction of the globe was able to successfully reposition the globe. Various materials have been used in these procedures, including titanium mesh, silicon sheets, autogenous bone and porous polyethylene. Titanium mesh was chosen for this patient as it had several advantages including biocompatibility, cost-effectiveness and the ability to be appropriately contoured to fit a large wall deficit.1,6
In conclusion, traumatic globe subluxation is relatively uncommon. Same-day repair increases the probability of improved visual outcome. Surgical techniques include direct traction to reposition the globe to an anatomical location. Repair of the fracture is crucial to prevent re-subluxation of the globe. Persistent ocular motility restrictions and late enophthalmos are complications, even in the cases with good visual outcomes.
1. Amaral MB, Nery AC. Traumatic globe dislocation into the paranasal sinuses: Literature review and treatment guidelines. J Craniomaxillofac Surg 2016;44:5:642-647.
2. Noman SA, Shindy MI. Immediate surgical management of traumatic dislocation of the eye globe into the maxillary sinus: Report of a rare case and literature review. Craniomaxillofac Trauma Reconstr 2017;10:2:151-158.
3. Kreiner B, Amer R, Sharfi G, Solomon A, Ilsar M. Traumatic displacement of the globe into the paranasal sinuses: Case report and guidelines for treatment. J Oral Maxillofac Surg 2008;66:4:826-830.
4. Alam MS, Noronha OV, Mukherjee B. Timing of surgery in traumatic globe dislocation. Indian J Ophthalmol 2017;65:8:767-770.
5. Lajoie J, Marous C, Wladis E. A case of traumatic globe subluxation into the paranasal sinuses. Abstract presented at: American Society of Ophthalmic Trauma, Paper Session III. June 4, 2022.
6. Haggerty CJ, Roman P. Repositioning of a traumatically displaced globe with maxillary antrostomy: Review of the literature and treatment recommendations. J Oral Maxillofac Surg 2013;71:11:1915-1922.
7. Ramstead C, McCabe J, Alkahtani M, Leong-Sit J, Morhart M. Traumatic dislocation of the globe into the maxillary sinus. Can J Ophthalmol 2008;43:3:364-366.
8. Hazani R, Yaremchuk MJ. Correction of posttraumatic enophthalmos. Arch Plast Surg 2012;39:1:11-17.
9. Xu B, Xu XL, Yan J. Treatment of traumatic globe dislocated completely into the maxillary sinus. Int J Ophthalmol 2013;6:1:106-107.
10. Abrishami M, Aletaha M, Bagheri A, Salour SH, Yazdani S. Traumatic subluxation of the globe into the maxillary sinus. Ophthalmic Plast Reconstr Surg 2007;23:2:156-158.



