When Belgian refractive surgeon Erik Mertens began using Bausch & Lomb's Zyoptix system, his retreatment rate was 20 percent, mainly from overcorrections and not having a custom nomogram yet. Now, however, after incorporating what he's learned about the system's nuances, he's pleased to report a retreatment rate of only 2.3 percent. If you're thinking about using Zyoptix, here's advice from Dr. Mertens and other experts that will help you optimize your treatments, too.
Getting a Measurement
The Zyoptix system is composed of three main hardware components, the Zywave aberrometer, the Orbscan topographer and the Technolas 217z excimer laser. It's new software is called Zylink, which takes the wavefront data from the Zywave and translates it into an ablation pattern.
Surgeons say good measurements start with good techs. They train their techs to be proficient with the Zywave and in identifying good and bad wavefront images. This keeps things flowing in your clinic, since the preop workup can take as long as 40 minutes longer than a conventional one when done by unskilled hands.
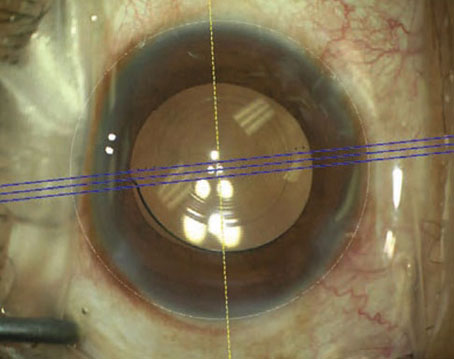
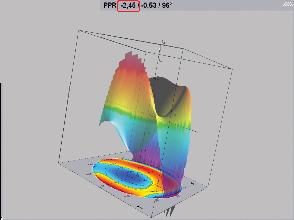 |
| Even low myopes such as this patient can have significant aberrations that can be addressed with a custom treatment. |
"You want one or two of your most competent tech(s) doing this," says Rochester, N.Y., surgeon and Zyoptix investigator Scott MacRae, "because that person will need to critically look at the scans and make sure they're of good quality, which is really important. If they're not, the tech has to know when to repeat them."
Next, surgeons say you have to take care when dilating the patient before taking the wavefront, which requires at least a 6.5-mm pupil. Louis Probst, MD, who practices both in the Chicago area and in Canada, says he uses a dilation technique recommended to him by Argentina's Roberto Zaldivar, MD.
"Applying numerous dilating drops induces a toxic keratopathy that almost destroys your wavefront map," Dr. Probst says. "So, the best way to dilate is to instill one drop of 2.5 % neosynephrine and 0.8 % Mydriacyl (tropicamide) and have the patient close the eye for five minutes. Then, use a pupillometer to see how large the pupil becomes in the dark." He says that, usually, by then the pupil is about 6.5 mm and he can do a Zywave measurement, leaving no time for toxic keratopathy to develop.
Third, the patient himself can help you get a good measurement.
"Make sure the patient sits at the device with a straight back without tilting his head," says Dr. Mertens. "Ensure he doesn't look directly at the fixation light. Instead, have him look a little bit above it. If he looks into the light, he'll automatically try to keep it in focus and will be accommodating. This will result in higher myopic values than the eye really has. Stress to him the importance of being relaxed, not focusing on anything, as if he's just staring into the distance."
If the pupil doesn't dilate as widely as you need, Dr. Mertens recommends adding one drop of unpreserved tropicamide, then measuring the pupil within two or three minutes.
After you complete the series of five wavefront scans, the Zywave will throw out two outliers and keep three. All the surgeons say that it's important to print out the three original scans for reference, because once you move past them in the system you can't retrieve them. This may change, at least overseas, in the next few months, says Dr. Mertens. He says the company plans to release new software that will allow the surgeon to save these screens in order to look at them later. He's not certain when this feature will be available to U.S. users, however.
"Have the tech print the Zywave screen demonstrating the three scans, the pupil dilation and the grid of lenslet light spots to confirm that the three scans are similar, the pupil hasn't dilated asymmetrically and the lenslet spots are clear and consistent," advises Dr. MacRae.
After you've acquired the wavefront data, surgeons advise you to make sure that the spherical error as measured by the Zywave's phoropter predicted refraction is within 0.75 D of the subjective refraction, that the cylinder is within 0.5 D and that the astigmatic axis is within 15 degrees.
"If this isn't the case, don't proceed," says Dr. Mertens. "You can try re-examining the patient, but don't treat him with those values."
Since, at first, it can take 10 minutes or more to prepare a floppy disk with all the necessary data to be fed into the laser and for the Zylink software to determine a laser shot pattern from that data, Dr. MacRae has his tech load the data beforehand and then reviews the Zylink with the tech either in the afternoon prior to the treatment day or the morning of the treatment.
Treating the Patient
• Alignment and centration. To make sure the operating microscope, laser and cornea are all aligned properly, Dr. Mertens first marks the horizontal axis of the cornea at the slit lamp. He puts the slit in the horizontal position and marks the cornea at the limbus on either side of the slit.
"That way, I know exactly where the horizontal axis of the cornea is when the patient lies down," he says. "Cyclotorsion of 10 degrees can negate the benefit of Zyoptix."
He also takes care to make sure the microscope is aligned with the laser.
"When you change the interpupillary distance of the microscope, you shift the horizontal line in the microscope," he says. "So, if you have different surgeons using the same laser, the horizontal line of the microscope may not be the same as the laser's."
To align the two devices, he activates the fixation light and the aiming beam of the laser, then presses the F5 key on the Zyoptix keyboard. The aiming beam, which doesn't blink, will jump aside and the line going between the blinking fixation light will be the horizontal line of the laser.
"Turn the horizontal line of the crosshairs in your microscope and put it in the same direction as the two dots, and it will then be the same as the zero axis of the laser," he explains. "When the patient is lying beneath the laser, you only have to look at your horizontal line in the microscope and align it with the two marks on the cornea. If the corneal marks aren't in line with the microscope cross, ask the patient to move his upper body to the left or right in respect to what you see in the microscope. Then, you can align the cornea and the microscope, the latter of which you've already aligned with the laser."
• Asymmetric dilation. When capturing the wavefront, Dr. MacRae advises to "check to make sure the pupillary center is close to where it is naturally; occasionally you'll see a 0.1-mm to 0.3-mm shift, In which case you may want to redilate and make sure it's centered."
"If a rare shift of 0.5-mm occurred, I'd bring the person back and try to get him to dilate symmetrically with 0.5% mydriacyl, or 1% if I had already used 0.5%," says Dr. MacRae. "You can see the eccentric dilation on the lenslet light spot printout. If the pupil centers are still shifting, I'd consider doing a conventional treatment."
Dr. Mertens performs his treatments on dilated eyes in an effort to avoid decentration problems.
"That's why the printed screens of the original three wavefront measurements are important," he says. "With them, you can verify how the dilation was during the measurements and make sure that it's the same way before the actual treatment."
• Overcorrections. The surgeons agree that the Zyoptix system tends to overcorrect patients until its user refines his nomogram. Because of this, they recommend backing off the target correction by around 6 to 12 percent. You can do this in the Zylink window, but only by a maximum amount of 0.75 D.
• Large zones. "In the clinical trial, we found our outcomes were better when we treated with a 6.5 mm-7 mm optical zone then with a 6-mm one," explains Dr. MacRae. "This held true for all outcomes: higher-order aberrations, contrast sensitivity, uncorrected acuity and patient satisfaction. The larger the zone, the more you can reduce higher-order aberrations."
Dr. MacRae notes, though, that anatomical considerations may outweigh the need for a larger zone. "If someone has a low mesopic pupil diameter of 5 mm, you don't need to treat her with a 7-mm zone. She'd probably be happy with a 6.5-mm one," he says. "There's no need to take that much tissue because her pupil doesn't dilate that widely."