Scientists compared the rate of intraoperative complications and visual outcomes in patients with neovascular age-related macular degeneration and control eyes without nAMD undergoing phacoemulsification.
As part of the multicenter retrospective, non-randomized comparative study, investigators classified eyes based on the presence or absence of a nAMD diagnosis. The main outcomes were: the rate of intraoperative complications; the logMAR visual acuity at four to 12 weeks postoperatively in both groups; and the reinjection rate of intravitreal anti-VEGF after phacoemulsification.
Here are some of the findings:
- Preoperative VA was worse in the nAMD group (0.9 +0.5) vs. the reference group (0.6 +0.5).
- No difference was reported in the rates of posterior capsule rupture (PCR) (2.90 vs. 2.77 percent; p=0.889), dropped lens fragments (0.46 vs. 0.29 percent; p=0.618) or zonular dialysis (0.46 vs. 0.58 percent; p=0.749) between the two groups.
- Receiving ≥10 intravitreal injections before cataract surgery predicted the likelihood of PCR with an odds ratio of 2.86 (p=0.027).
- The proportion of eyes achieving a visual gain of ≥0.3 logMAR (∼3 Snellen lines equivalent) was lower in nAMD eyes (39.2 vs. 63.7 percent; p<0.0001).
- A total of 203 eyes (73 percent) in the active treatment group and 139 eyes (36 percent) in the inactive treatment group received more than one intravitreal injection after phacoemulsification (p<0.0001).
- Scientists reported that the risk of posterior capsule rupture was higher for eyes receiving ≥10 intravitreal injections before phacoemulsification. Only 39 percent of eyes with neovascular age-related macular degeneration had visual improvement by ≥3 Snellen lines.
J Cataract Refract Surg 2023; Sep 26. [Epub ahead of print].
Siddiqui M, Elhusseiny A, Soliman M, et al.
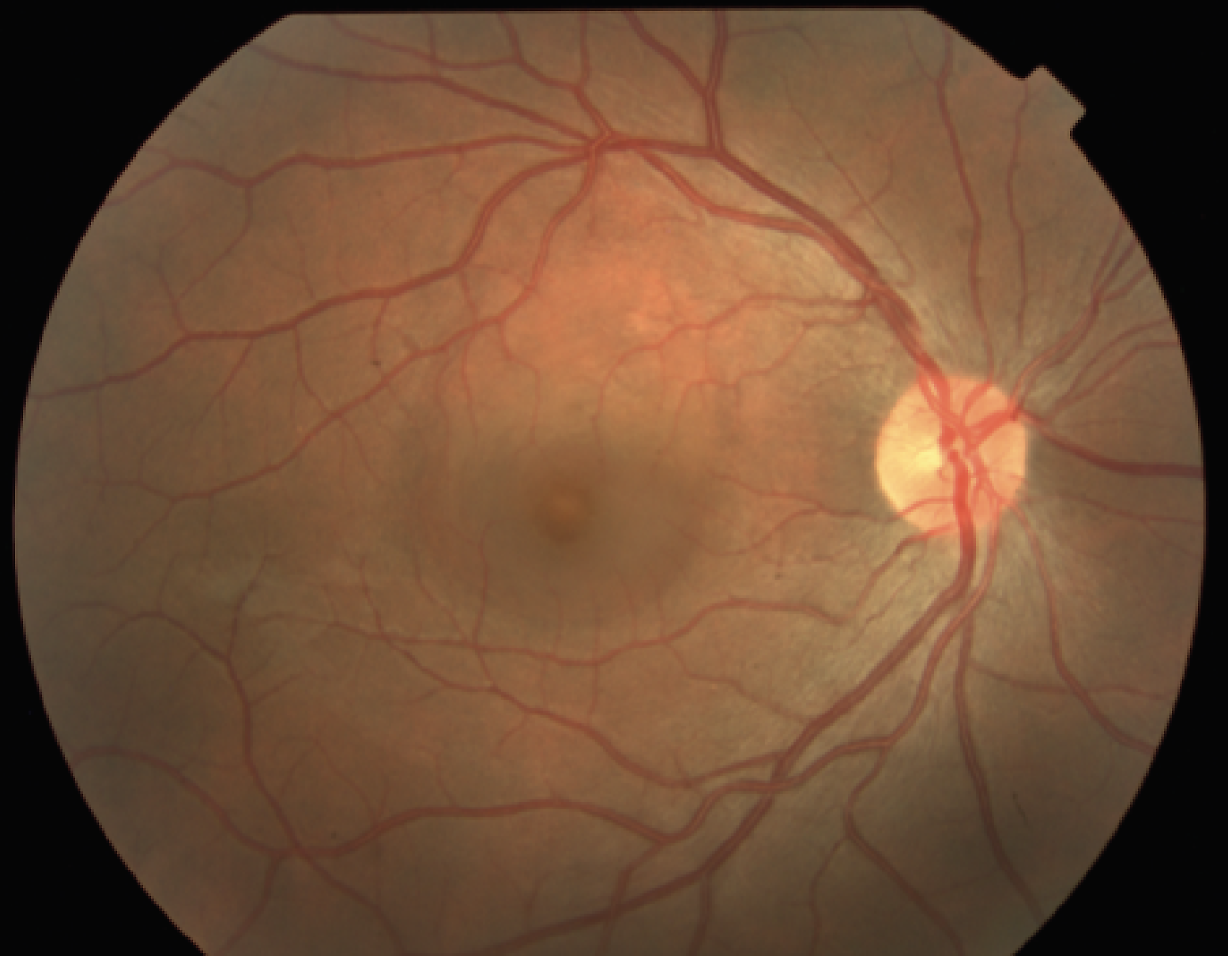
Conversion of Drusen to MNV
Investigators analyzed imaging features preceding the occurrence of type 3 (T3) macular neovascularization using tracked spectral-domain optical coherence tomography.
From a cohort of eyes with T3 MNV and ≥12 months of prior tracked SD-OCT, T3 lesions that developed above soft drusen were selected for OCT analysis. Retinal imaging findings at the location where type T3 MNV occurred were analyzed at each follow-up until the onset of T3 MNV. The following OCT parameters were assessed: drusen size (height and width); outer nuclear layer (ONL)/Henle fiber layer (HFL) thickness at the drusen apex; the presence of intraretinal hyperreflective foci (HRF), retinal pigment epithelium (RPE) disruption, incomplete RPE and outer retina atrophy (iRORA); and complete RORA (cRORA).
Here are some of the findings:
- From a cohort of 31 eyes with T3 MNV, T3 lesions developed above soft drusen in 20 eyes (64.5 percent).
- Drusen showed progressive growth (p<0.001) associated with ONL/HFL (p<0.001) thinning prior to T3 MNV.
- The following OCT features were identified preceding the occurrence of T3 MNV, typically at the apex of the drusenoid lesion: disruption of the external limiting membrane (ELM)/ellipsoid zone (EZ) and/or the RPE; HRF; and iRORA/cRORA.
Investigators found specific anatomic alterations preceding the occurrence of type 3 macular neovascularization that commonly originate above soft drusen, including drusen growth, reduced outer nuclear layer/Henle fiber layer thickness and RPE atrophy at the drusen apex. They suggested that identifying these features should warrant close monitoring for identification of type 3 macular neovascularization, which can benefit from prompt intravitreal anti-VEGF therapy.
Retina 2023; Sep 19. [Epub ahead of print].
Bousquet E, Santina A, Corradetti G, et al.
Corneal Ulcers in Ocular Graft vs. Host Disease
Scientists evaluated the incidence, clinical characteristics, microbiological profile and therapeutic outcomes of corneal ulcers in individuals with chronic ocular graft-vs-host disease.
The retrospective clinical cohort study involved a review of individuals diagnosed with graft-vs-host disease following hematopoietic stem cell transplantation (HSCT) seen at the Bascom Palmer Eye Institute between May 2010 and November 2021. Baseline demographics, clinical characteristics, microbiological profile, risk factors for corneal ulceration and treatment outcomes were studied. Etiology was deemed infectious in individuals with a positive culture or appropriate clinical scenario (presence of stromal infiltrate or hypopyon); otherwise, ulcers were presumed to be non-infectious. Treatment success was defined as re-epithelialization with infiltrate resolution, and treatment failure was defined as progression to corneal perforation or keratoplasty. Kaplan-Meier survival analysis was used to estimate the incidence of ulceration while Cox regression analyses helped evaluate demographic and risk factors. Infectious and non-infectious ulcer groups were compared using two-way independent T tests, one-way analysis of variances (ANOVAs) and chi-squared tests.
A total of 173 individuals were included (53.7 ±14.4 years old; 59 percent male).
Here are some of the findings:
- Thirty-three individuals developed an ulcer 74.5 ±54.3 months after HSCT, with estimated five- and 10-year incidences of 14 and 30 percent, respectively.
- Twenty-two ulcers (66.6 percent) were deemed infectious (15 confirmed microbiologically, seven clinically) and 11 (33.3 percent) were deemed non-infectious.
- Risk factors for corneal ulceration included: black race (HR: 2.89; CI, 1.30 to 6.42; p<0.01); previous ocular surgery (HR: 9.16; CI, 3.86 to 21.72; p<0.01); lid margin abnormalities (HR: 3.44; CI, 1.69 to 6.99; p<0.01); and topical steroid use (HR: 2.74; CI, 1.33 to 5.62; p<0.01).
- Contact lens use reduced the risk of corneal ulceration (HR: 0.29; CI, 0.13 to 0.66; p<0.01).
- Infectious ulcers had a significantly higher frequency of treatment failure than non-infectious ulcers (57.1 vs. 20.0 percent; p=0.04).
Scientists determined that corneal ulceration is a potential complication of graft-vs-host disease, with several clinical features identified as risk factors. They added that infectious ulcers had worse outcomes than non-infectious ulcers.
Am J Ophthalmol 2023; Sep 27. [Epub ahead of print].
Sepulveda-Beltran PA, Carletti P, Banda V, et al.
 |
Anti-VEGF Treatment Response in CSCR
Researchers identified baseline predictors of anti-VEGF treatment response at three years in patients affected by choroidal neovascularization secondary to central serous chorioretinopathy.
In the retrospective longitudinal study, medical records of patients diagnosed with choroidal neovascularization secondary to central serous chorioretinopathy and treated using anti-VEGF injections between April 2015 and May 2020, were reviewed. The study’s researchers identified or measured the potential qualitative and quantitative predictors of treatment response based on baseline multimodal imaging exams available, including structural optical coherence tomography, fluorescein angiography, indocyanine green angiography and OCT-angiography. Univariate and multivariate analyses were performed.
Twenty-nine eyes from 29 patients affected by CNV complicating CSCR were included. Here are some of the findings:
- At the end of the three-year follow-up, the mean BCVA was 20/50 Snellen equivalent (0.38 ±0.36 logMAR), and no significant difference was found from baseline BCVA (0.37 ±0.29 logMAR) (p=0.9).
- Twenty out of 29 eyes (69 percent) had active lesions at the end of the follow-up.
- At multivariate analysis, no included features were independently associated with three-year BCVA outcomes.
- Pigment epithelium detachment height (ß=0.017; p=0.028) and outer limiting membrane preservation at the fovea (ß=-5.637; p=0.026) were independently associated with choroidal neovascularization activity at three years.
Researchers found that pigment epithelium detachment height and outer limiting membrane obliteration at the fovea might be considered baseline predictors of lesion activity at three-year follow-up in patients with choroidal neovascularization secondary to central serous chorioretinopathy treated with anti-VEGF therapy.
Graefes Arch Clin Exp Ophthalmol 2023; Sep 29. [Epub ahead of print].
Cozzupoli GM, Sacconi R, Tombolini B, et al.



