Performing cataract surgery in a patient who has an overfiltering trabeculectomy is a scenario we all hope to avoid. Nevertheless, it’s good to be prepared, because sooner or later every glaucoma or cataract surgeon will be faced with such a patient.
A trabeculectomy can be very effective for lowering the intraocular pressure when the normal outflow channels aren’t functioning well. If a trabeculectomy works too well, however, the result can be hypotony and its attendant sequelae. The visual consequences of hypotony are problematic, and measures must be taken to increase the IOP. Unfortunately, fixing hypotony is challenging; it’s much easier to lower IOP in a glaucoma patient than it is to raise it. Furthermore, care must be taken to not elevate the IOP too much in patients with known glaucomatous damage.
Facing hypotony in a patient with a visually significant cataract introduces even more variables and challenges. Here, I’ll offer some suggestions for managing a patient in this situation, to increase the likelihood of achieving the best possible outcome when performing cataract surgery.
Asking Key Questions
When you’re planning to do cataract surgery on a patient with an overfiltering, hypotonous trabeculectomy, preoperative considerations are arguably the most important step. It’s important to ask four main questions before you operate on these patients:
• Is this really hypotony? First of all, you need to decide whether your patient is hypotonous—meaning that the patient is symptomatic from the low IOP. Symptomatic hypotony isn’t associated with a specific IOP; some people may be hypotonous at a pressure of 7 mmHg, while others may not have signs of hypotony despite an IOP of 2 mmHg.
Population-based normative values indicate that an IOP of 10 mmHg or less is below “normal.”
More patients may develop complications of low IOP at 5 mmHg or less, which is a threshold for hypotony often used in clinical trials. However, these numerical thresholds don’t reflect the reality that some patients may have lower measurements of IOP but not have any ocular complications due to the low IOP.
The presence of symptomatic hypotony is indicated by clinical signs such as decreased vision, hypotony maculopathy (which you can see on exam or OCT), and sometimes choroidal effusions or corneal folds. If your patient has an IOP of 2 or 3 mmHg, but their visual acuity is 20/20, they have no visual distortions and they’re happy as a clam, that’s not hypotony.
Whether or not the signs of hypotony appear seems to depend on how much a given eye can tolerate at a given pressure. That means that hypotony is very patient-dependent. That’s why your first step is deciding whether the low IOP you’re finding is associated with hypotony.
Once you’ve decided that the patient’s IOP really is lower than it should be, the next three questions become crucial:
• How long has the patient been hypotonous? If it’s been more than six months or a year, there may be some irreversible components to the hypotony—especially hypotony maculopathy, which can lead to blurred, distorted and decreased vision. If the hypotony maculopathy has been present for a long time, the odds of a perfect outcome are diminished, so you need to make sure you set the patient’s expectations appropriately.
• How much of an IOP increase are you looking for? If you’re starting from 6 mmHg and looking to nudge the IOP up a little bit, you’re going to use different techniques than if you’re starting at a pressure of 0 or 1 mmHg and trying to increase that pressure to 10 mmHg. (More about those techniques in a minute.)
 |
| Performing a surgical revision of the bleb is a good way to proceed if you need a significant increase in IOP to avoid the consequences of doing cataract surgery on a hypotonous eye. This should be done prior to the cataract surgery to ensure that optical measurements are made with the eye at a normal pressure. |
How much you need to raise the pressure will help you answer the next question:
• Should I address the hypotony before, during or after the cataract surgery? If you’re trying to increase the IOP a lot, I’d argue you’ll be better off trying to accomplish that beforehand, to ensure the accuracy of your IOL calculations. We know that the axial length of the eye can increase when IOP increases. That means that if you measure the axial length before addressing the hypotony and the pressure is normalized later, your cataract surgery will lead to a myopic surprise.
Studies have shown that in the presence of a normally functioning trabeculectomy bleb the axial length can increase by 0.1 to 0.2 mm when the eye pressure increases. That effect is magnified in the presence of hypotony and its resolution. For example, I had a patient who had refractively very similar eyes prior to a blunt injury to her left eye that resulted in a cyclodialysis cleft and an IOP of 2 mmHg. When I did her IOL calculations, the axial length in that eye was nearly 3 mm shorter than in the right eye. (See last figure) If I had just used those measurements to determine what IOL power to implant, without taking the hypotony into consideration, the numbers would have called for an 8-D stronger IOL than she actually needed after the hypotony resolved. She would have been pretty unhappy with me!
The other thing that can be altered by hypotony is the corneal shape; keratometry readings can shift significantly. As a result, you have to be very wary of implanting toric lenses when measurements may have been made in the presence of hypotony.
For example, I’ve seen instances in which keratometry done on an eye with a pressure of 0 mmHg showed what appeared to be 3 D of regular with-the-rule astigmatism; when the IOP was raised to a physiologic pressure, the astigmatism disappeared completely. If you’d placed a toric lens in this eye, you would have ended up actually inducing astigmatism after a more normal pressure was restored.
The bottom line is, if the eye has significant hypotony and you’re starting from a very low IOP, I’d recommend addressing the hypotony first and performing cataract surgery later. You’ll end up with much more accurate preoperative calculations and more predictable outcomes.
There will be situations in which the pressure is just a little low, and the patient doesn’t have maculopathy or visual distortions. In that case I might decide to wait and address the low IOP during or after the cataract surgery, to avoid having to take the patient to the OR twice.
Correcting Low IOP
There are a number of techniques for addressing low IOP, but I’ve found three to be particularly helpful. The first is surgical revision of the trabeculectomy. This will give you the biggest increase in IOP, and this is the approach I’d typically recommend doing before cataract surgery. The second method is using fewer postoperative steroids following the cataract surgery. This is useful when you’re just looking to nudge up the IOP. The third option I sometimes use is an autologous blood patch. It is easy to do in clinic and can help to raise the IOP a few points, and can be done either preoperatively or postoperatively, if cutting back on the steroids didn’t quite raise the pressure enough.
Let’s look at each of these more closely:
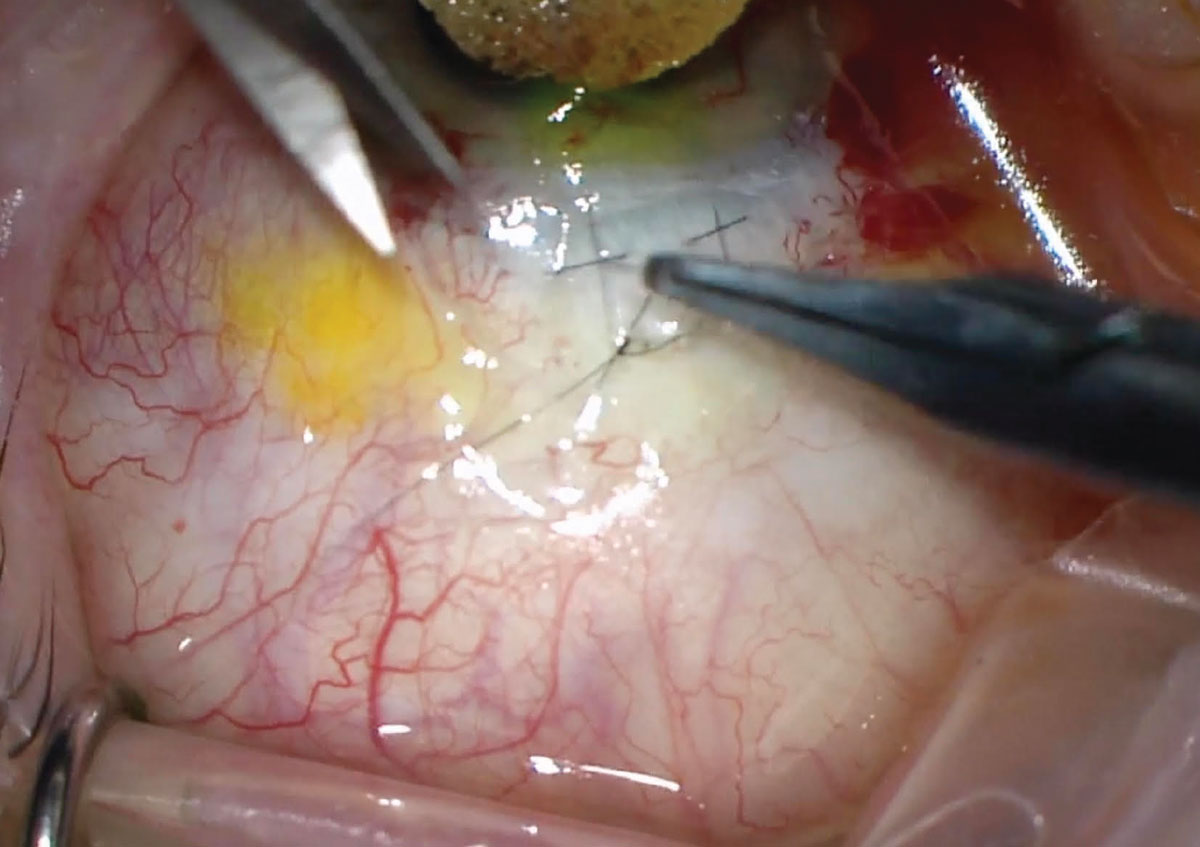
• Perform a surgical revision. This is useful if you’re trying to increase the IOP by a significant margin. Often this involves replacing the nylon sutures in the scleral flap as a way to decrease the flow through the trabeculectomy flap. This has to be done in the OR and it takes time, both for the surgeon in the OR and for the patient through recovery. However, if you’re starting from a point at which the patient is significantly hypotonous and vision is symptomatic, this is the best route to go, even though it means an extra trip to the OR.
In terms of the benefits of choosing this option, it’s the most effective way to increase the IOP. By decreasing the outflow through the trabeculectomy flap, you’re getting to the root of the problem. The primary downside is that you could unintentionally trigger the original problem that caused the patient to need a trabeculectomy in the first place: too high a pressure. If the IOP climbs too high, you’ll need to be prepared. Are you willing to do laser suture lysis? Bleb needling? Placing a tube shunt at some point in the future?
This means that if you close off the trabeculectomy and decrease the flow, you have to be ready to deal with any unintended consequences. You have to be thinking about the next step, just in case you’re too successful at getting the pressure back up.
One other caution: When you do this in the OR, do a more thorough conjunctival closure than you might do in an initial trabeculectomy surgery, because this eye’s already been operated on, and the tissues may have already been exposed to mitomycin-C or other antimetabolites that can make the conjunctival tissue less robust.
Some patients will have a low pressure but be largely asymptomatic, so doing a surgical revision is probably not necessary. A patient like that might be on the edge of hypotony, but not yet in trouble. In that situation, it would make me feel better knowing that the intraocular pressure was a little bit higher, a little more physiologic, so I might use one of the next two techniques to nudge the IOP up just a little.
• Use fewer postoperative steroids. When doing a normal cataract surgery on a patient who doesn’t have a trabeculectomy, my normal postoperative steroid regimen begins at four times a day, followed by a weekly taper. If a cataract patient has a well-functioning trabeculectomy, I revise this protocol. Studies have shown that performing cataract surgery on a patient with a trabeculectomy can cause the bleb profile to become smaller, and generally causes an IOP increase on the order of 2 to 4 mmHg.1 Often, I’m looking to preserve flow through a trabeculectomy, so to help prevent the IOP rise, I increase the use of steroids, starting at every two hours.
In hypotony, I suggest taking advantage of this phenomenon instead. If the patient has just a small amount of hypotony—not enough to justify a trip to the OR for a flap revision—I’d complete a normal cataract surgery and then simply use fewer or no postoperative steroids. The idea is that the small amount of inflammation stirred up by the cataract surgery—if we don’t temper it with steroids—may be enough to promote subconjunctival scarring. This can decrease the flow through the trabeculectomy, thus raising the IOP by a few points.
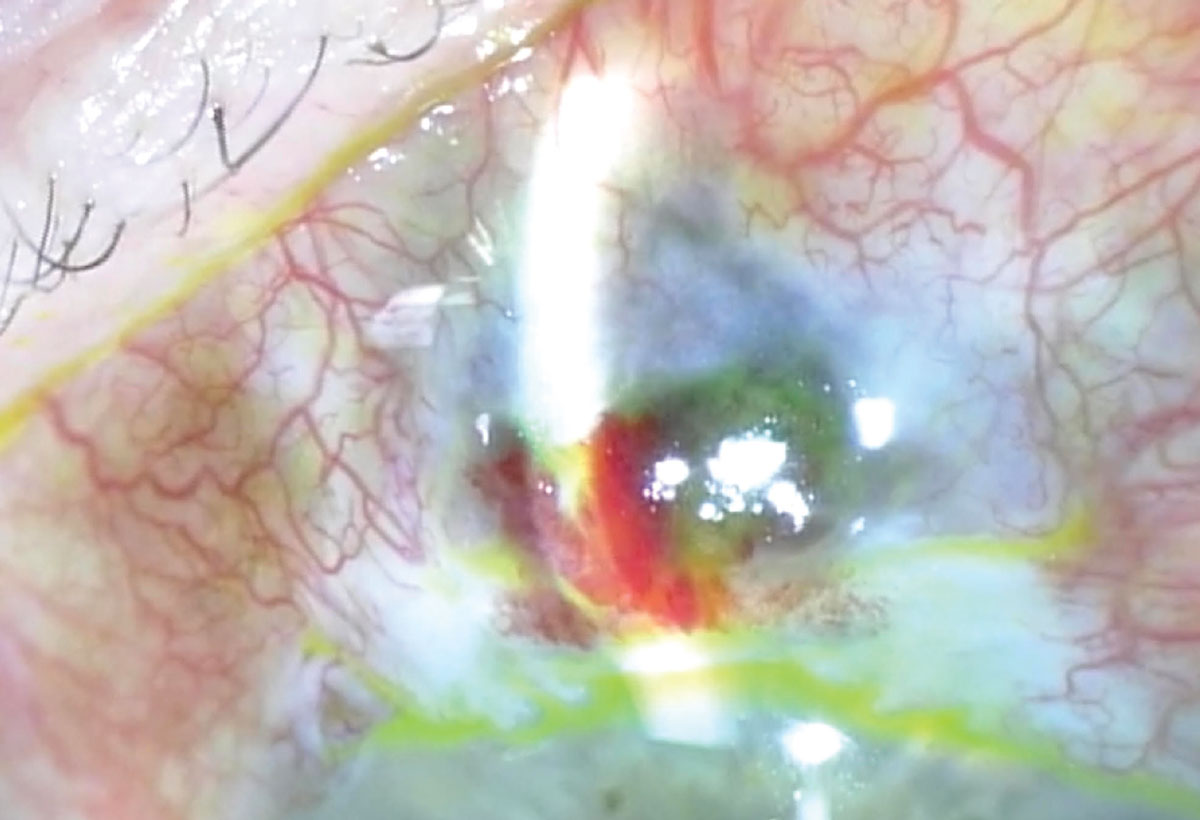 |
| If the patient has a low IOP related to an overfiltering trabeculectomy, a blood patch can be used to elevate IOP a little. This involves injecting a little bit of the patient’s blood into the bleb to promote conjunctival scarring and thus decrease aqueous outflow by a small amount. |
The biggest benefit of this approach is that it’s very easy to do—you’re simply using fewer or no postoperative drops following an otherwise normal cataract surgery. The downside is that you should only expect a small pressure increase. This strategy certainly won’t cause the pressure to rebound from 0 mmHg, for example, but it’s a really good technique if you’re starting from 6 or 7 mmHg and just trying to get the IOP up by a small amount.
• Try using an autologous blood patch. The blood patch is another option that only creates a small IOP increase; it involves injecting a little bit of the patient’s blood into the bleb to promote conjunctival scarring and thus decrease outflow by a small amount.
The technique should be familiar to many surgeons; it’s a lot like needling a bleb. We prep the eye much as we would for needling. Then, I have an assistant help draw up the patient’s blood. The assistant immediately hands me a syringe containing a small amount of blood, and I add a 27- or 30-gauge needle. Starting away from the bleb, I tunnel underneath the conjunctiva and inject a little of the patient’s blood into the bleb. (In needling, I’d be trying to break through the scarring and loculations; here I’m just trying to enter the bleb and loculations with as little disruption as possible.) It doesn’t require much blood to achieve the desired effect.
This is not a novel technique, but it’s certainly worth revisiting. It was first described in 1993 by James Wise, MD.2 In his series, he found that doing this increased IOP from 5.5 to 8.2 mmHg, on average. Although this is a small increase, it’s enough to improve visual acuity from average of 20/148 to 20/30, making a significant clinical difference for these patients. My experience has been similar.
Since this is done in clinic, you can use a blood patch to nudge up the pressure at any point. Also, you can use this in conjunction with the previous technique, in which you try to nudge the pressure up by using fewer postoperative steroids, if you didn’t get enough effect.
The biggest advantage of this technique is that it’s also very easy to do; it uses tools and techniques that a lot of us already have. The downside is that, like cutting back on the postoperative steroids, it will only give you a small IOP increase. So, you have to set appropriate expectations going in. You definitely can’t use this to resolve hypotony starting at a pressure of 0 mmHg.
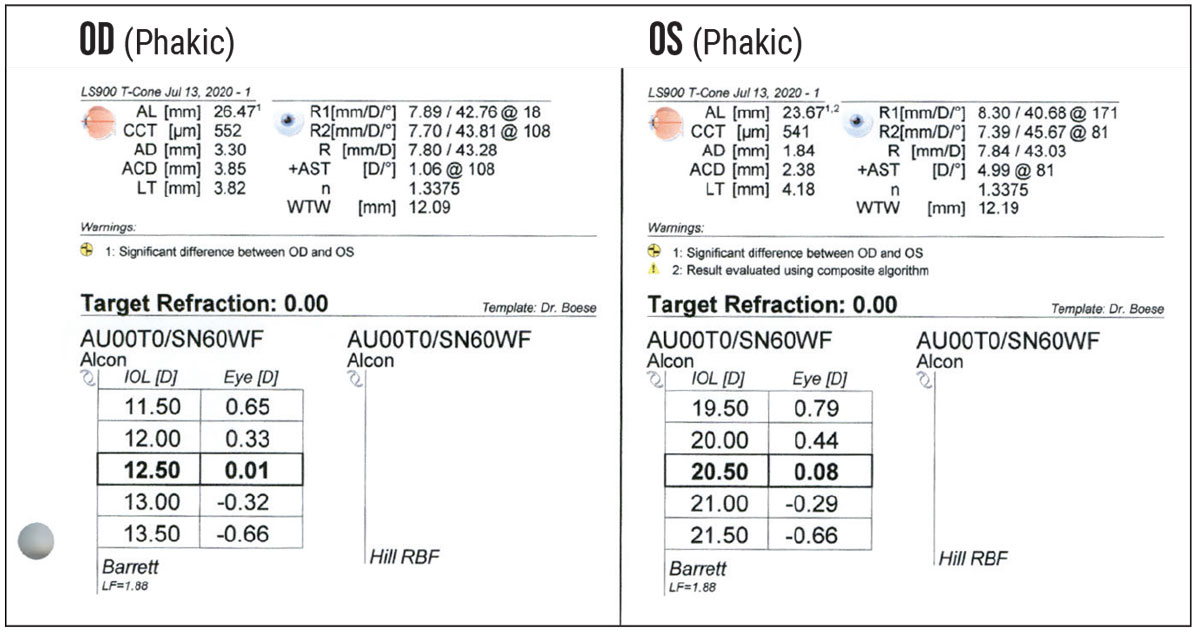 |
| Intraocular lens calculations for a patient with hypotony in her left eye caused by a traumatic cyclodialysis cleft. Measurements found a nearly 3-mm difference in axial eye length between her eyes, resulting in an 8-D difference in IOL power. |
Intraoperative Considerations
Whenever I have a cataract surgery patient with a trabeculectomy, I recommend approaching the cataract surgery a little differently:
• Use a lower bottle height. The idea is to reduce the turbulence during the surgery. Excess flow can cause a subconjunctival donut, limiting visualization. It can also inadvertently land you in a position where the integrity of the bleb could be compromised, inviting an unexpected and complicated surgery to repair the damage.
• Take extra precautions to avoid nicking the conjunctiva when making your clear-cornea incision. You don’t want to nick the conjunctival vessels, potentially causing a leak.
Interestingly, if the eye has a mature bleb, I don’t find that the fluidics change much, even if the bleb is overfiltering. However, be wary of performing cataract surgery on an eye with a recently performed trabeculectomy; you may end up with a very unstable chamber.
Ensuring a Good Outcome
To summarize: When you’re thinking about cataract surgery and the patient has an overfiltering trabeculectomy, there are a few different approaches that can be used, depending on the degree of hypotony. If the patient has clinical signs of hypotony, steps should be taken to raise the IOP before performing the IOL power calculations and cataract surgery. This will require two trips to the OR, but it’s worth it; you’re going to get better IOL power calculations, more controlled outcomes and happier patients.
On the other hand, if the patient has a low IOP with minimal or no hypotony, using fewer or no postoperative steroids after a standard phacoemulsification can cause decreased flow and increased IOP. If that isn’t enough, then an autologous blood patch is a great clinical technique to augment the pressure.
No matter which approach you use, it’s important to address hypotony to ensure the best possible outcome.
Dr. Singh is a professor of ophthalmology and chief of the Glaucoma Division at Stanford University School of Medicine. Dr. Netland is Vernah Scott Moyston Professor and Chair at the University of Virginia in Charlottesville.
Dr. Boese is a clinical assistant professor and glaucoma specialist at the University of Iowa. She is a past winner of the American Glaucoma Society’s Young Clinician Scientist Award and the David Epstein Clinician-Scientist Research Award. She reports no financial ties to anything discussed in this article.
1. Rebolleda G, Muñoz-Negrete FJ. Phacoemulsification in eyes with functioning filtering blebs: A prospective study. Ophthalmology 2002; 109:2248-2255.
2. Wise JB. Treatment of chronic postfiltration hypotony by intrableb injection of autologous blood. Arch Ophthalmol 1993;111:827-830.



