Here, surgeons who offer corneal inlays—both the Kamra and the defunct Raindrop—weigh in on who’s getting them, the mechanics of implanting them, their pros and cons, and where they think the future of inlays is headed.
Slow Adoption
John A. Hovanesian, MD, clinical instructor at the Jules Stein Eye Institute, University of California, Los Angeles, and in practice at Harvard Eye Associates in Laguna Hills, believes that incorporating corneal inlays into refractive practice is well worth the effort, but notes that they haven’t penetrated the market deeply. “I think we surgeons as a population have been pretty hesitant to take up inlays. There is a learning curve for us, and a phase of patient education that we need to go through,” he says. He says ReVision Optics’ closing and discontinuation of the Raindrop was a result of several factors. “The technology itself was a good performer,” he says. “It was good enough for me to implant two inlays in close, personal friends, both of whom were quite happy. Personally, I believe the slow adoption of the Raindrop inlay was attributable to the ‘competition’ of great results with LASIK and premium IOLs. While neither procedure is ideally suited to the emmetropic presbyope who was a candidate for Raindrop, both have received wide public acceptance and adoption by surgeons. In addition, achieving a quiet eye with the Raindrop inlay required more follow-up and diligence after surgery than other refractive procedures.”
Currently, ophthalmology has been slow to dive into inlays. It’s possible that, as Dr. Hovanesian notes, surgeons aren’t interested in cresting a new learning curve. In terms of safety and efficacy, in the absence of a lot of large-scale, postmarket data, U.S. ophthalmologists have the FDA trials to go on for the Kamra (AcuFocus; Irvine, California) and the discontinued Raindrop. The FDA’s summary
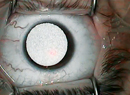
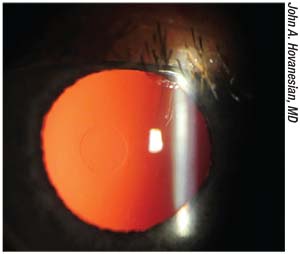
 |
| Because it is made of dark polyvinylidene fluoride, the Kamra small-aperture inlay may be visible in eyes with light-colored irises. |
“We know they can work, because there are practices that are really succeeding with them,” Dr. Hovanesian says. “We refractive surgeons need to try and make this a successful addition to our surgical armamentarium.”
Who’s Getting Them?
Surgeons say that, in the right patients, the inlays can work well.
Dr. Hovanesian says that inlays are aimed at emmetropic presbyopes, who are a tricky group to satisfy. “These patients have low refractive error but desire freedom from eyeglasses for reading. Such patients tend to be in their late 40s to 50s,” he says. “They don’t have significant cataract yet and they’re highly motivated to do something. They have heard of LASIK; most of them have heard of monovision, but many have a bias against it. A traditional approach is unlikely to apply very well to them, making inlays a good fit.”
Jeffery J. Machat, MD, FRCSC, DABO, medical director of Nvision Eye Centers in Toronto and San Francisco, became part of the inlay market in August 2012, when he decided to get a Kamra implanted in his own eye. “There’s sort of a moment that hits you where all of a sudden, you feel your age,” he says. “For me, it was the size of the font on my iPhone—and my teenage daughter who tormented me about it for an entire day. I said to myself, ‘Okay, that’s it. I need to do something.’ ”
A refractive surgeon with 27 years of experience at the time, Dr. Machat sought a treatment with a high safety profile. “A corneal inlay made a lot of sense to me,” he recalls. At the ASCRS meeting that year, he listened to John A. Vukich, MD, present early FDA data on the Kamra. Dr. Vukich closed with a case presentation, in which he revealed that he was in fact the subject. Dr. Machat recalls that he was convinced to proceed after questioning Dr. Vukich post presentation. “I went ahead and had it done myself with Dr. Minoru Tomita in Japan, and I was really thrilled. I had a very fast visual recovery. The very next day I was already J1, and three days later I was operating,” he says.
Shortly after the procedure, Dr. Machat integrated the Kamra into his Toronto practice. “We got approval [from Health Canada] in September 2012. At that time, they were still doing thick corneal flaps, not pockets, for insertion of the inlay. But we rapidly learned that a pocket deeper in the cornea was a better approach surgically and we got far better results, so there was definitely a learning curve,” he says.
The current version of the Kamra inlay is a dark polyvinylidene fluoride ring etched with perforations, 6 µm thick and 3.8 mm in diameter. Its central aperture is 1.6 mm, and it is placed over the first Purkinje image when implanted into a stromal pocket 200 to 250 µm deep. Long-term data suggest that the Kamra results in notably improved monocular and binocular uncorrected near and intermediate vision, with a small loss of monocular and binocular uncorrected distance visual acuity. In a study with five-year follow-up, mean UNVA at 60 months was improved from J7/J8 preoperatively to J3 ±2 lines. Of 32 patients, two required recentration of the inlay at six months; one Kamra was explanted due to unsatisfactory hyperopic shift; one patient had epithelial ingrowth in the early postop period.5 Notably, the study patients got their inlays from 2006 to 2007, and so were implanted with an earlier version of the Kamra that was 10 µm thick, etched with fewer holes and that allowed more unfocused light onto the retina.
John A. Vukich, MD, associate clinical professor of ophthalmology at the University of Wisconsin Madison School of Medicine and in private practice at Davis Duehr Dean Eye Care in Madison—and the impetus for Dr. Machat’s decision to get his own inlay—says that most of his inlay patients present as prospective LASIK patients. “The most common inlay patients that we treat are individuals who are interested in LASIK to begin with, and then this creates a value-added option,” he explains. “Patients who are looking for LASIK in the presbyopic range are generally either higher myopes (-4, -5, -6 D) or they are hyperopic. They understand that they have to wear reading glasses over their contact lenses if they’re hyperopic; or if they’re myopic above -4 D, they can’t take their glasses off and read comfortably. These individuals all understand the inconvenience of presbyopia, and they also understand that being able to have that extended depth of focus and freedom from reading glasses—or a least a significantly diminished need for them—is a real benefit,” says Dr. Vukich, who offers the Kamra inlay to his patients.
Making It Work
Dr. Hovanesian notes that a patient’s preop refraction is important when placing an inlay. “I tend to prefer the Kamra for patients who are slightly myopic,” he says. “As we know, the ideal patient for the Kamra is about -0.75 D. For the Raindrop, the ideal patient was more like a +0.75 D.
“Another thing to consider is that there is a little cosmetic concern with the Kamra, particularly for people with lighter-colored eyes, because it can be visible to the patient,” continues Dr. Hovanesian. “I’ve not actually had anyone who’s received it and been unhappy with it, regardless of eye color, but I think it’s a conversation worth having with patients.” Of the 44 explanted Kamras in the FDA pivotal study cohort, two were removed for cosmesis.3
When he combines inlays with LASIK, Dr. Hovanesian notes it’s important to adjust the refractive target. “In those who are more myopic it’s best to undercorrect the nondominant eye with the intention of later putting in a Kamra,” he explains.
Dr. Hovanesian looks forward to the FDA approval of the Flexivue Microlens (Presbia Coöperatief U.A.; Irvine, California), a refractive inlay 3 mm in diameter made of clear UV-blocking copolymer. The central zone has zero refractive power and a 0.15-mm hole. Its peripheral zone comes with add powers ranging from +1.25 to +3.5 D in 0.25-D increments. The Microlens varies in thickness from 15 to 20 µm, depending on add power. “It’s still undergoing FDA trials. But so far, the data look good and it should offer promise as another valuable entrant into this market,” he says. The multicenter Phase III trial will follow approximately 412 patients between 45 and 60 years old implanted with the Microlens. The study is expected to wrap up in early 2019 (ClinicalTrials.gov Identifier: NCT02110472).
In a study of 47 emmetropic presbyopes with the Microlens inserted in a femtosecond laser-created corneal pocket 280 µm deep, no complications occurred over the 12-month follow-up period, and 75 percent of the patients achieved uncorrected near visual acuity of 20/32 or better in the operated eye. The operated eyes’ mean uncorrected distance acuity dropped from 20/20 preop to 20/50 (p<0.001), while mean binocular UDVA did not change significantly (p=0.516).6
“I’ve done the Microlens in Canada,” says Dr. Machat. He observes that patients could start with one Flexivue lens power and then replace it with a higher one as presbyopia progresses, but also that patients getting inlays generally won’t do this. “We have found in our very limited experience that patients do not want to put in an inlay and then come back in two or three years for another one. From a patient’s-reality perspective, most people will just put in a +2.25 D Microlens and that’s it. Patients were losing more distance than we expected, but getting good reading,” he says.
Lifelong Implant
“I’m excited about corneal inlays because I think of them as a lifelong procedure for patients. With the Kamra, we’re altering the cornea to allow depth of focus, and that change in shape lasts the rest of the patient’s life, even after a cataract surgery,” says Dr. Hovanesian. “We have in fact done cataract surgery on patients who have previously undergone Kamra as part of the FDA study prior to approval, and those patients have done very well.”
Dr. Machat concurs that corneal inlays can last a lifetime without complicating future ophthalmic interventions. “The Kamra inlay and the Raindrop inlay continue to work until someone develops a cataract,” he says. “I’m going to leave my corneal inlay in once I develop lenticular opacities, and just put in a monofocal IOL and target -1 D for reading. I won’t need to put a multifocal in my left eye; I won’t need to remove it. I won’t need to do anything,” he says.
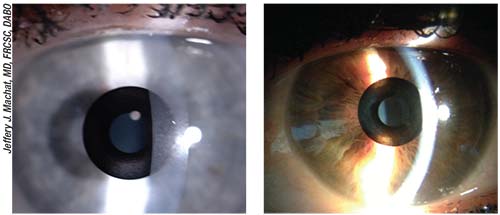
Dr. Machat
 |
| A surgeon opens the pocket in preparation for sliding in the Kamra presbyopic intracorneal inlay. |
“I’ll do LASIK for about 80 percent of my corneal inlays,” Dr. Machat continues. “So this has increased my LASIK practice. We often have patients who are early presbyopes and we just leave them a little bit undercorrected; that’ll put off their need for readers for about five years, and then they’ll come back as soon as they need a corneal inlay. All of a sudden, that inlay takes the -0.75 D and gives them 3 D of accommodative range, so they’re thrilled. We’ve done them in pseudophakes; we’ve done them in post-LASIK patients and post-PRK patients, as well as in virgin corneas. It’s definitely worked well for us.”
“In terms of this being a treatment for life, our experience has been that you can certainly do a cataract surgery with these inlays in place, and it really doesn’t get in the way,” concurs Dr. Vukich, who also says that the majority of his Kamra patients need to be brought to plano or -0.5 to -0.75 D of sphere correction in their nondominant eye to prepare for the inlay.
The Kamra obstructs the view of a small portion of the retina. The FDA summary report on the Kamra warns that medical laser treatments for certain eye conditions may warrant extra caution or even removal of the inlay.3 “Retinal surgeons initially felt like there might be some obstructed view, but that hasn’t turned out to be the case,” says Dr. Vukich. “You can see around them quite easily.”
Dr. Hovanesian doesn’t think they pose much of a visibility problem in the event of future retinal evaluation and treatment, either. “Some retinal specialists are concerned about this with the Kamra, but if you have a pupil that dilates reasonably well then it’s really not an issue to see around it,” he says. “It’s like looking around a tiny corneal scar: You still see around it if the cornea is clear outside the area of the inlay.”
Challenges with Inlays
Some surgeons think the slow adoption rate of corneal inlays among surgeons may just be explained by their relative novelty on the refractive scene.
“The challenge with inlays is a lack of familiarity on the part of the general public,” says Dr. Hovanesian. “When we started doing LASIK years ago, it was perceived as a cutting-edge, possibly risky new procedure. People had questions about safety; they had questions about long-term stability of results. Today, 20 years later, everyone has friends who’ve been through LASIK and who’ve had positive things to say about it. Inlays are like LASIK was 20 years ago. We have to help patients understand what they are, how they work, and what their benefits are.”
“It’s not unlike the early days of LASIK surgery,” agrees Dr. Vukich. “It took a couple of years before patients really understood and knew someone who’d had it done,” he says. “It’s true that we’re not seeing huge numbers at this point, but it is quietly and steadily gaining momentum.”
Dr. Machat introduces a corneal inlay as an improvement on LASIK alone. “We present it to patients as an upgrade, he says. “If you get LASIK, you’re going to get distance vision but you’re going to need reading glasses. Patients ask if there are any other options. We like the corneal inlay because patients retain binocular distance vision. If someone has -1 D monovision, that monovision will only
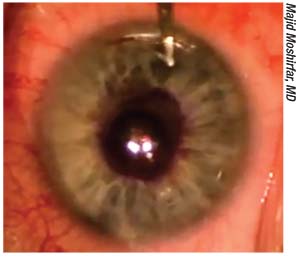
 |
| The Raindrop was a nonrefractive inlay made of clear hydrogel. It approximated the cornea’s refractive index. |
“The word of mouth has been quite dramatic,” Dr. Machat continues. “If you think of myopes, one in four of their friends are myopic: When you think of presbyopes, 100 percent of their friends are presbyopic. Having presbyopic solutions that go beyond multifocal IOLs is a vital part of any refractive practice.”
Dr. Hovanesian says that his staff and co-managing optometrists help get the word out about corneal inlays. “We have folks in the practice who do that very well, along with some docs outside. Just like there was with LASIK, there’s a bit of education mode that the co-managing doctors have to engage in,” he says.
“Train your staff,” urges Dr. Machat. “Get them on board. Really make sure that they understand, because this is a new but highly effective treatment. Also, have an age-appropriate patient consultant. We hired patient consultants who were in their 50s, because someone who’s in their 50s doesn’t want to talk to a 24-year-old. They want to talk to someone who can actually relate to them and understand presbyopia. I gave a patient consultant on my staff LASIK because she was a moderately high myope, and I inserted a Kamra inlay. She was then able to really talk to our patients about it.”
In addition to educating patients about the benefits of corneal inlays, setting their expectations is also key. “You have to tell patients ahead of time that vision does improve, but it may take a couple of weeks, and sometimes, it may take even a little longer before they get the full effect,” stresses Dr. Vukich. “I simply tell patients, ‘It’s going to take a little while, so if you’re not getting the full effect, we anticipate that. It takes awhile for things to settle down and for the ocular surface to optimize and for the healing to take place,’” he says. “Patients need to know what to expect.”
Fine-tune Your Follow-up
“There is clearly a period of postoperative care that is necessary with inlays,” Dr. Vukich continues. “These patients are treated with steroids, typically for up to a month or longer after the procedure on a tapering schedule. Typically, we see them at one day, one week, and one month, but of course we’d adjust that as necessary.”
Dr. Hovanesian says that you may need to train your staff to do a little more handholding for postoperative inlay patients than for post-LASIK patients. “There’s a little bit of healing time. There’s a little bit more follow-up care,” he notes. He adds that some inlay patients may need a reminder of their preop vision to appreciate how far they’ve come postoperatively. “Some patients get an inlay, and six months later they kind of forget what their preop vision was like. One thing that we actually learned to do from the FDA study—and I recommend this to all surgeons—is to take a little handheld 8.5 x 11-inch reading card, and have the patient read the smallest print they can on it. Have them sign it, and put it in their chart. Later, if they’re wondering if their inlay is doing anything for them, you can pull that card out and show them. They can always read much better after the procedure than before and sometimes they’re amazed at what a difference it’s made. They simply forgot how bad their previous reading vision was. Sometimes you just have to remind patients of what you’ve done for them.”
Having experienced the Kamra as both a patient and a surgeon affords Dr. Machat insight when answering patients’ questions about potential near-vision difficulty under mesopic conditions. “All presbyopes have trouble when it’s dark,” he says, “but it’s not like the inlay makes your vision much darker, so that you suddenly have to use a light when you didn’t previously. But there is also retinal adaptation occurring. It’s very interesting.” Dr. Machat says he experienced this adaptation firsthand as his vision in low-light conditions steadily improved during the postoperative months. Dr. Machat’s clinical director, Sondra Black, OD, reported the same thing after her Kamra procedure, he says. “She found that her vision under low light improved over an entire year. When you talk to scientists like Jay Pepose, he says that this is exactly what occurs. I got to live it. I was very surprised by it and it didn’t make sense to me, but it’s true,” he says.
For all the potential benefits corneal inlays can confer, the procedure also confers the risks that come with putting a foreign body into the eye. “There is no such thing as a surgery that has a zero complication rate. Anytime we do something, there’s the possibility of an unexpected or untoward outcome,” Dr. Vukich notes of his experience with the Kamra. “One of the things we have seen is epithelial implantation: At the time the implant was placed, a nest of epithelial cells was brought in with the implant. We believe it occurs in less than a fraction of 1 percent of patients, and it’s easily fixed. We can simply rinse out the epithelial cells. We’ve also had one patient in which the implant was slightly irregular because of a micro-fold. That was early on in my experience, so there is a bit of a learning curve in terms of how to place the implant quickly, atraumatically and in the location that you’re looking for,” he says, “but inlay surgery is well within the skill set of any anterior segment surgeon.”
One potential plus of corneal inlays is that they are strictly additive and removable. “There’s no such thing as a reversible operation, but the inlay is clearly removable. So to the extent that we can restore the native architecture—with the exception of the incision we’ve made—by removing the implant, I think people find that reassuring,” says Dr. Vukich, who reports that he has explanted one Kamra. Although patients who have their refraction set for anisometropia in anticipation of an inlay are left in that state if the inlay later comes out, Dr. Vukich says that this has not been problematic over the course of his experience with the Kamra. “If and when an implant needs to be removed, the opportunity for enhancement to bring patients to emmetropia exists and we’ll tell them we can do that, but we really have not had anyone ask for it,” he says, adding that patients enjoy the near component created by LASIK in the nondominant eye despite a slight loss of distance visual acuity.
Check Your Technology
Dr. Machat notes that you need the right tools to offer corneal inlays. “You have to keep a really high-quality femtosecond laser with a really tight raster pattern,” he says. “So that was one of the advantages of using the Raindrop: You just needed to make a flap that was one-third of the central corneal thickness, so you didn’t need pocket software,” he says.
Although he acknowledges that obtaining the requisite technology for corneal inlays might be prohibitively costly for surgeons not currently offering LASIK, Dr. Vukich says that investment is minimal for those already offering it. “For a surgeon who is already doing LASIK surgery, there is almost no startup cost to this,” he says.
Dr. Machat says he purchased the AcuTarget HD, the forerunner of the HD Analyzer (Visiometrics; Costa Mesa, California) when he started offering the Kamra. The costly imager is pretty much a must-buy for Kamra surgeons, a fact that may have discouraged some from getting involved with Kamra. Dr. Machat also suspects that the system’s name at that time led to some surgeons declining to adopt inlays because of a mistaken belief that the AcuTarget was only good for inlay centration. “What they’re not realizing is that I use it for Kamra only 5 percent of the time; 95 percent of the time, I use it for refractive lens exchange, dry eye and other procedures,” he says.
Dr. Vukich also says that the HD Analyzer is a great help with inlays, but that it its use isn’t limited to that area of practice. “I think that in the setting of using inlays it’s quite valuable to have, but quite frankly, we use it far more widely than just for implanting inlays,” he says. REVIEW
Dr. Hovanesian was a consultant for ReVision Optics and consults for AcuFocus. Dr. Machat is on the medical advisory board for AcuFocus and is a consultant for Viseometrics. Dr. Vukich is a consultant for AcuFocus, and was an investigator and part of the FDA regulatory team.
1. Holden BA, Fricke JR, Ho SM, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol 2008;126:1731-39.
2. Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther 2017;6:55-65.
3. Food and Drug Administration. FDA summary of safety and effectiveness data (SSED). PMA P120023. https://www.accessdata.fda.gov/cdrh_docs/pdf12/P120023B.pdf. Retrieved 1/17/2018.
4. Food and Drug Administration. FDA summary of safety and effectiveness data (SSED). PMA P150034. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150034B.pdf. Retrieved 1/17/2018.
5. Dexl AK, Jell G, Strohmaier C, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg 2015;41:3:566–75.
6. Limnopoulu AN, Bouzoukis DI, Kymionis GD, et al. Visual outcomes and safety of a refractive corneal inlay for presbyopia using a femtosecond laser. J Refract Surg 2013;29:1:12-18.