 |
Should you lift the flap or leave it in place? The question continues to divide refractive surgeons when they discuss how to enhance post-LASIK patients. In this update, practitioners weigh in on this issue and discuss other personal approaches, providing insights on the timing of procedures, preop and postop evaluations, epithelial ingrowth, billing and make-or-break ways to ensure that initial imperfections don’t prevent you from eventually optimizing vision.
Which Side Are You On?
Edward Manche, MD, division chief of the cornea and refractive surgical service at the Byers Eye Institute at Stanford University School of Medicine, says he typically performs enhancements with a flap lift, when necessary, during the first 12 to 24 months after primary surgery. “Beyond that time frame, I turn to surface ablation,” he says. “If you do a lift during the first year or two, the risk of ingrowth is fairly low, about 1 to 2 percent. If you do it beyond that, the incidence increases dramatically.
After determining that an enhancement is indicated, Minneapolis surgeon Elizabeth A. Davis, adjunct assistant clinical professor at the University of Minnesota, says she uses PRK with mitomycin-C over the flap in 99 percent of her cases. “We did a study that demonstrated that nearly one-third of patients who underwent a flap lift experienced epithelial ingrowth,” says Dr. Davis. “The only rare time I might consider lifting a flap for an enhancement is if I find epithelial ingrowth under a flap, creating a refractive error. Then I lift and perform a small enhancement, though you must be careful in those cases because you don’t know what the refractive error might be once you remove the ingrowth. I might also consider lifting the flap for a significant hyperopic refractive error because, in my experience, hyperopic LASIK produces a better outcome than hyperopic PRK.”
 |
Dr. Davis proceeds with all enhancements only after confirming evidence of post-LASIK stability, as reflected in the refraction and topography. “For LASIK, my general rule of thumb is to enhance no earlier than three months after primary surgery, but it’s one month per diopter of myopia and three months per diopter of hyperopia,” she explains. “So if the patient’s a 1-D myope, I’ll do an enhancement at three months. If the patient’s a 6-D myope, I’ll do it at six months. If the patient’s a 1-D hyperope, it’ll be at three months.”
Deepinder K. Dhaliwal, MD, director of refractive surgery and the cornea service at the University of Pittsburgh Medical Center, says she prefers to lift the flap for enhancements, but only if she was the one who performed the primary surgery and only after meticulously evaluating the patient to determine if an enhancement is needed. “I’m a flap-lifter,” admits Dr. Dhaliwal. “If I’ve created the LASIK flap, I know it’s been created well, either with a microkeratome or a femtosecond laser. I have a special way of lifting the flap, scoring the edge at the slit lamp with a 30-gauge needle and then marking it with a pen. After that, I gently use a Sinskey hook, open the entire flap edge, peel it back and perform the enhancement. We then typically put a bandage contact lens over the eye. It’s a nice technique—very predictable and reproducible.”
Dr. Dhaliwal says careful assessment is essential to confirm that the patient is a good candidate for an enhancement. “This step is often overlooked,” she adds. “I’ve seen more complications after LASIK enhancements, usually ones referred to me, than after primary LASIK.”
To Enhance or Not
Before performing an enhancement, Dr. Dhaliwal images the cornea to find out what type of flap was initially created. “In the early days of microkeratomes, it was a bit like the Wild West,” she says. “If you’re going to lift, you really have to understand what’s going on. A buttonhole or some other unusual situation could be involved. Then, obviously, the surface laser is going to be a much better option. If the flap is not of good quality and integrity, I treat the surface.”
 |
When she decides to lift the flap, she doesn’t use a wavefront-guided approach. “I want to remove as little corneal tissue as possible,” she explains. “So I offer a conventional laser enhancement. Sometimes, when you attempt a custom treatment, challenging aberrations can result in a lot of tissue ablation. I try to keep it simple. We have to remember that we’re going in a second time. You want to minimize the risk of ectasia.”
Dr. Dhaliwal says she also holds off on patients who are approaching presbyopia. “They’ll need reading glasses if you take away the mild myopia,” she points out. “We do a contact lens trial to simulate the effect of the enhancement and determine if they really want it.”
When appropriate, Dr. Dhaliwal says she lifts a flap confidently, even years after primary surgery, without risking the development of epithelial ingrowth. “The way we do it, we usually don’t see epithelial ingrowth,” she says. “Of course I’ve had some, but the problem can be eliminated if you identify it early enough. (For strategies for managing epithelial ingrowth, see “After the Surgery” on page 14.)
Preparing for Enhancements
Many surgeons mentally prepare patients for LASIK enhancements before the primary procedure. “If you’re offering surgery to a younger cohort of patients, say 18 to 20 years old, even if they’ve gone one or two years without a change in glasses and their vision is defined as stable by FDA guidelines, that doesn’t mean they won’t experience progression,” says Dr. Manche. “I tell younger patients they’ll likely need additional surgery at some point. I even tell high myopes to wait until after age 30 before undergoing LASIK. Even then, there’s a risk of further progression.”
Dr. Davis prepares LASIK candidates for the eventual need for enhancements if they have high refractive errors—higher levels of myopia, higher levels of astigmatism or hyperopia. “Even though the overall percentage of patients who need an enhancement after LASIK is 5 percent, the risk for these patients may be greater than this,” she observes. “Not only that, if they have a higher refractive error, they’re going to have to wait longer for an enhancement to achieve stability.”
 |
Dr. Manche individualizes his preop patient communication based on the possibility of enhancements. “Our patients go into the first LASIK surgery fully informed,” he says. “For example, a preop patient may be at -8 D plus 3.5 D of cylinder. After surgery, the patient may be 20/30, but she understands the need to wait three to sixth months before we do a touch-up to try to get to 20/20.”
Despite clear communication, however, Dr. Manche acknowledges many patients perceive outcomes differently than surgeons do. “When we help a
-8 D patient end up at -0.5 D, at 20/25, and then we do a touch-up to get the patient to 20/20 or 20/15, we think, ‘Wow, look how well this case turned out.’ The patient’s view, however, is: ‘I had LASIK. It didn’t work at first and I had to go back and get it done again.’ It’s a different perspective that’s worth keeping in mind. I also make sure patients understand that I may need to lift the flap or perform PRK in one to two years, even after a perfect initial outcome.”
Dr. Davis also recommends a discussion of billing up front. “Surgeons take different approaches to billing,” she says. “I feel that, during the first year after surgery, I shouldn’t bill for enhancements for patients who aren’t on target after the first treatment. However, if we do achieve the target outcome and they come back in one, five or 10 years with changes in their vision that aren’t related to the primary surgery, then we bill them.”
Dr. Dhaliwal says some patients have unrealistic expectations. “They might think they’ve paid for a lifetime warranty, which is promised by many of the discount LASIK providers,” she observes. “You may encounter patients who feel ‘entitled’ to undergo a free enhancement, even though they’ve had very little education about the risks and benefits of the procedure. I consulted with one patient who developed infectious keratitis after undergoing a LASIK enhancement at one of the discount places. The patient said, ‘You know, if I thought there was a risk of infection after an enhancement, I wouldn’t have gotten this done.’ She felt her vision wasn’t that bad before the enhancement. But because she paid for a lifetime guarantee, she decided to take what she could get. So we have to be very careful about offering more surgery to these patients.”
After the Surgery
At some point, of course, all surgeons confront the challenges of minimizing or eliminating the threat of postop epithelial ingrowth, which can develop after primary surgery or after re-lifting the flap.
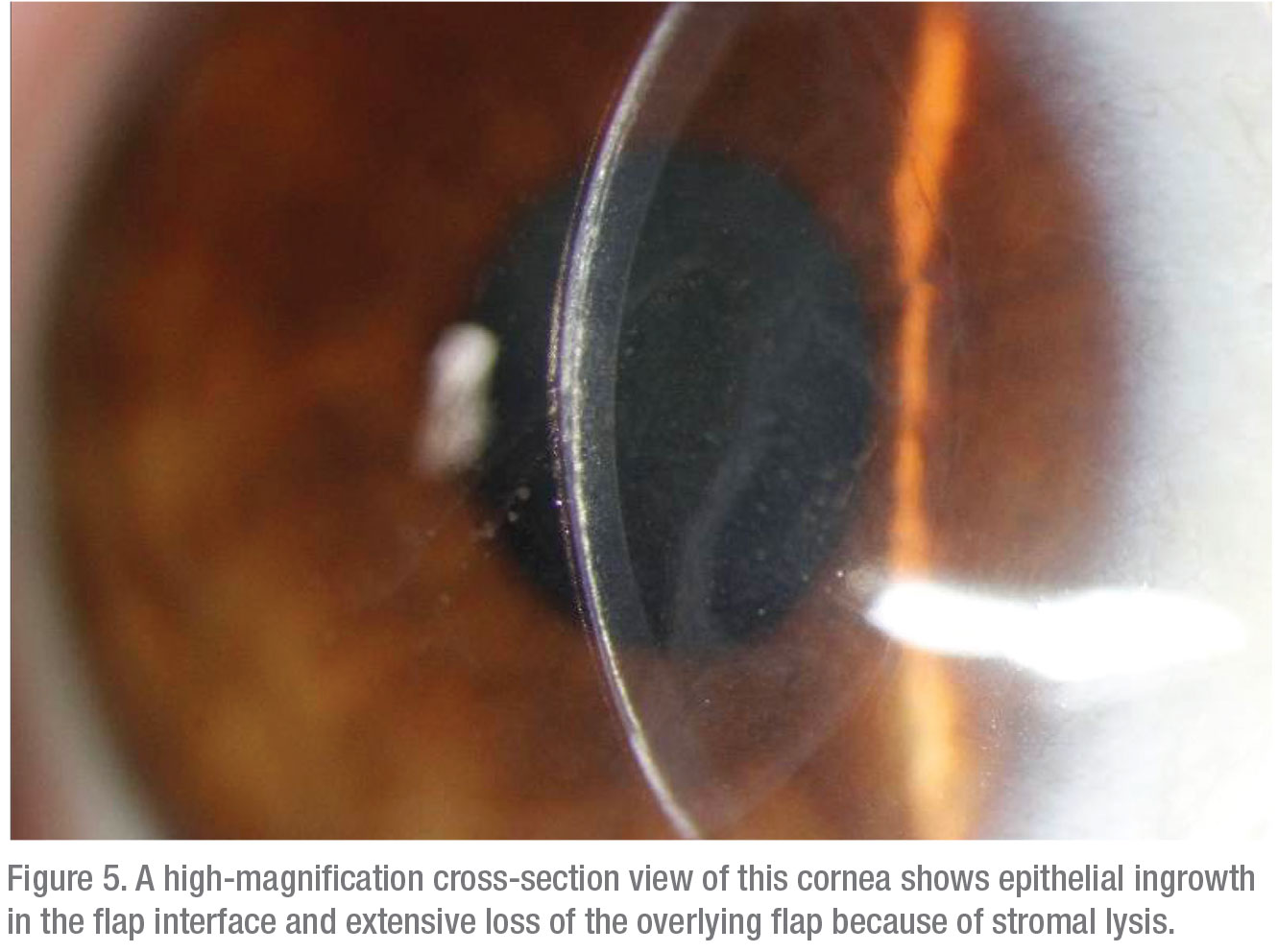
“In the past, I’ve had to manage patients who’ve developed significant epithelial ingrowth. Basically, when you recognize it, you have to re-lift the flap,” says Dr. Dhaliwal. “However, if it’s mild, less than 1 mm into the stromal surface, if there’s no associated flap melting and if it’s not causing any irregular astigmatism or refractive changes, then I leave it alone. If it’s growing and affecting the patient’s vision, then I’ll lift the flap and deal with the epithelial ingrowth.
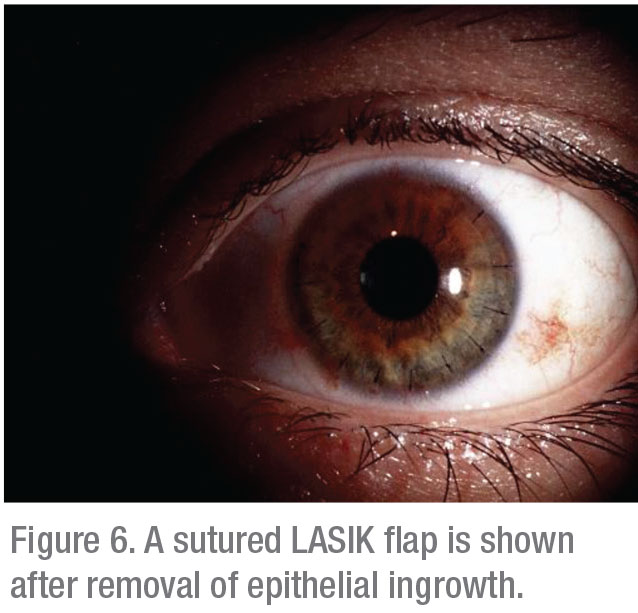
“I lift the flap and remove the ingrowth from both stromal surfaces, from underneath the flap and from the stromal bed,” she continues. “Then I replace the flap. I allow a long drying time of five minutes each in these cases, and I suture the flap down if it’s problematic, particularly if it’s the second time I’m lifting the flap. I’ll also use Tisseel fibrin glue (Baxter Healthcare) to keep it down. If it’s a high-quality flap, and I’ve made it myself and I know what’s going on, I prefer to lift it, as I mentioned.”
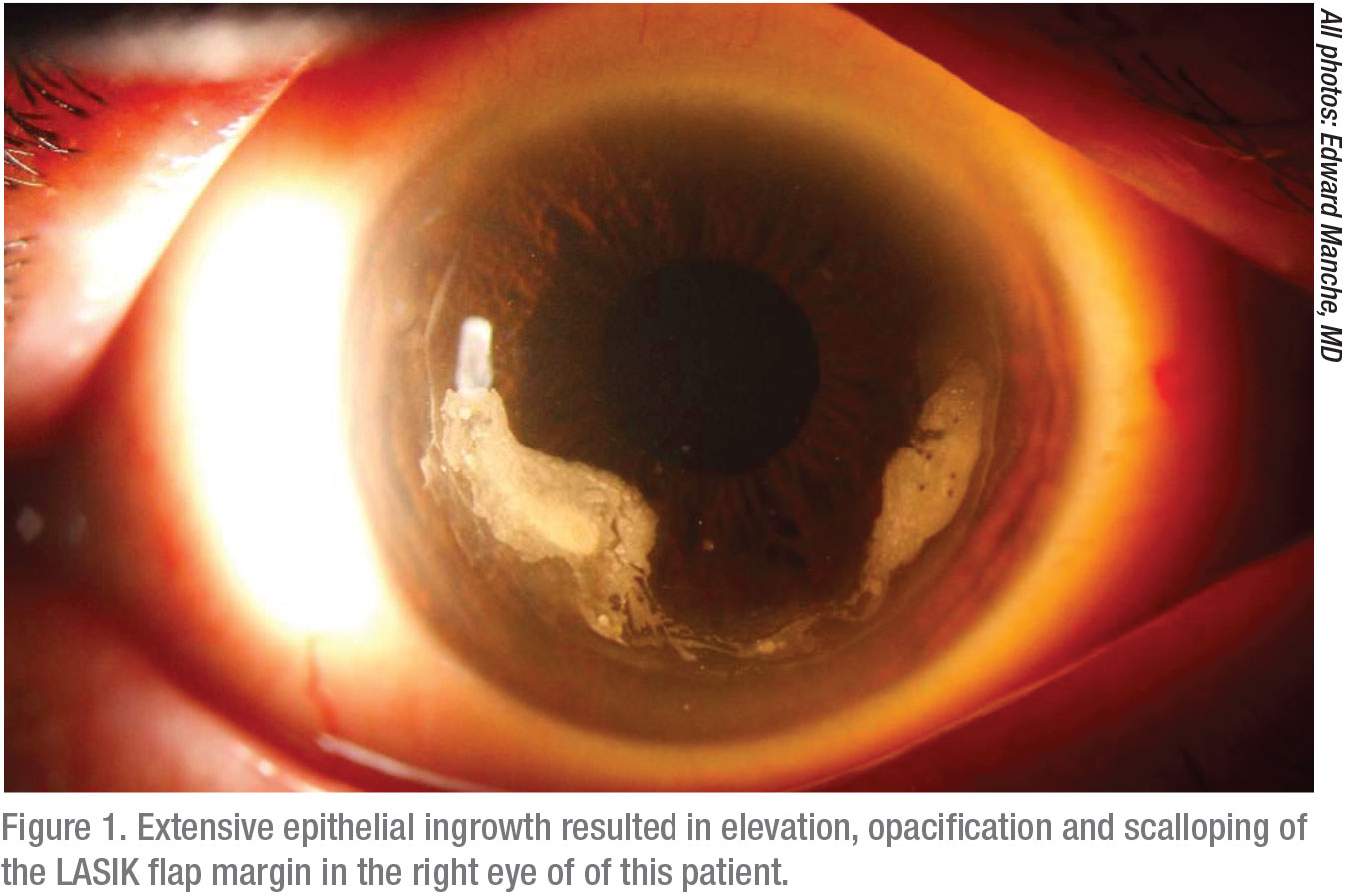
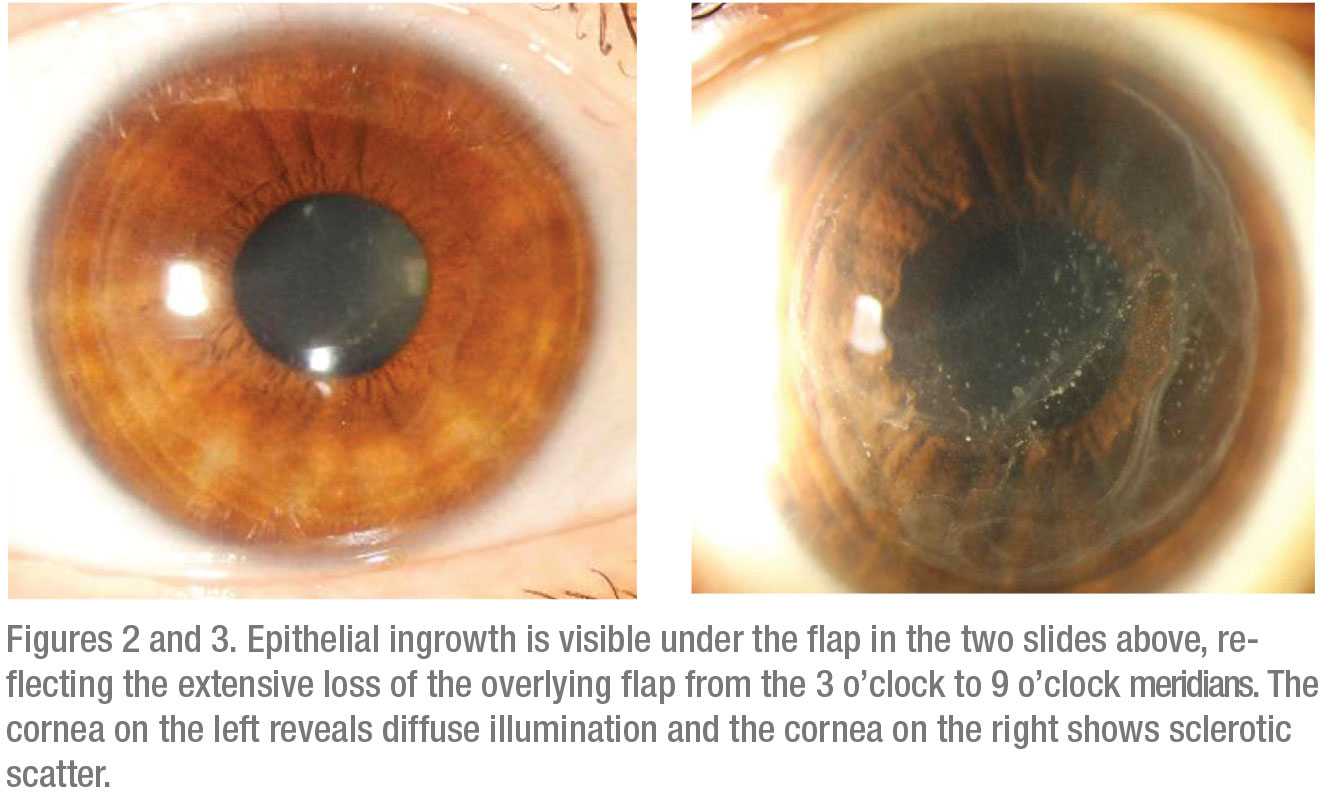
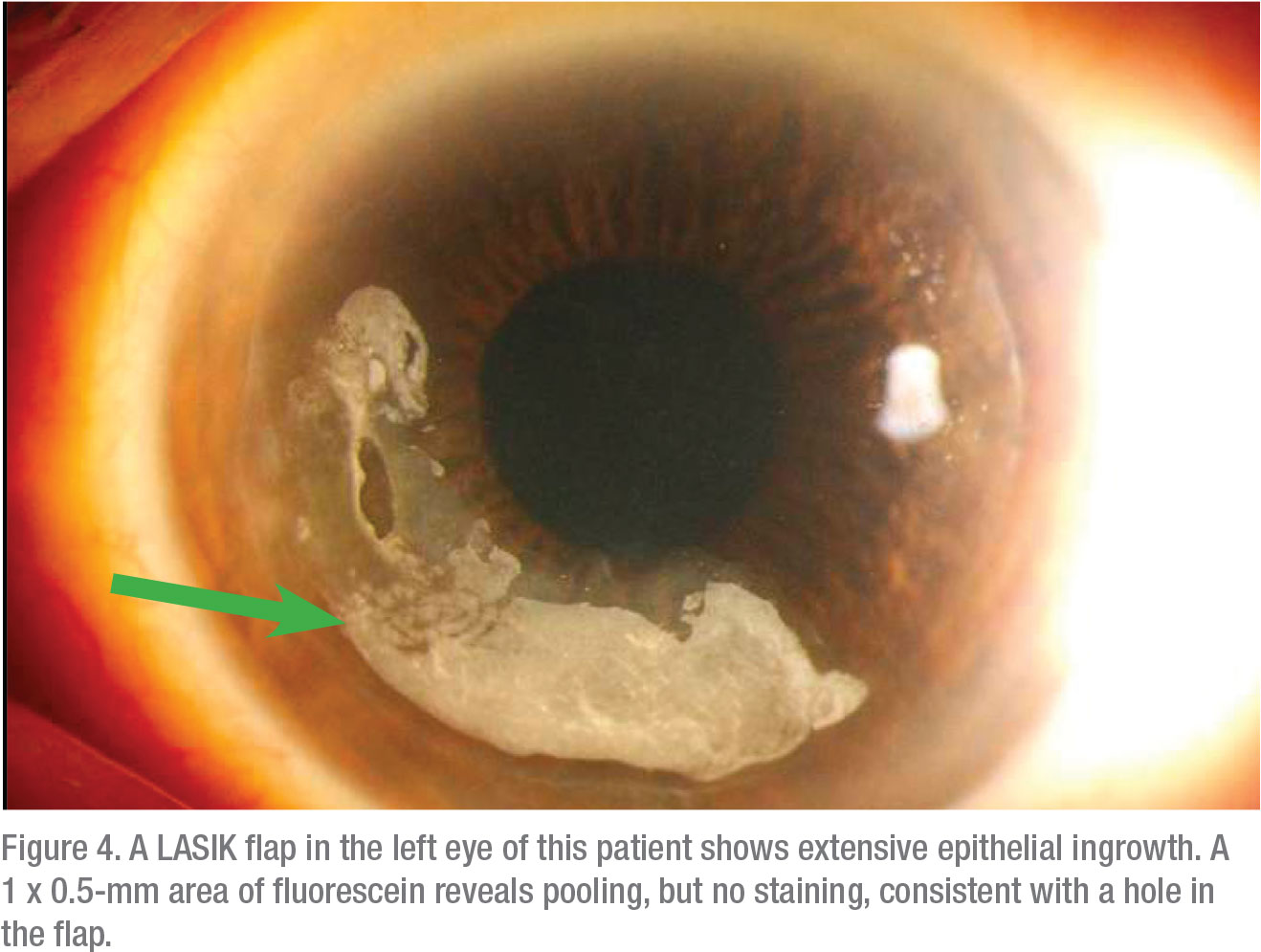
Although most epithelial ingrowth develops after enhancements, Dr. Manche cautions against overlooking the possibility of it developing after primary surgery. “You’ll see ingrowth in patients who have had complications from the original LASIK surgery, the most common complications being epithelial defects, epithelial sloughs and other issues of that nature,” he says. “If you develop epithelial ingrowth after primary surgery, for whatever reason, in most cases, identification and prompt intervention are critical.”
 |
These patients respond well to a lift-and-scrape technique, he notes. “You don’t need adjunctive therapies,” he says. “In most cases, if you identify epithelial ingrowth in the first month or two, you can just lift the flap and remove the ingrowth mechanically, then replace the flap, and that’s usually curative. Commonly, the location of the epithelial defect is where the epithelial ingrowth first develops. If the patient is yours, take meticulous notes after surgery, focusing on the area of the defect. During the first week, epithelial ingrowth is hard to see because it’s relatively transparent, forming almost a little ghost line under the flap. At three to four weeks, though, it starts to become more opaque and much more obvious. You can sometimes see elevation of the flap or—where the flap edge starts to get eaten away—scalloping of the flap. You want to be careful to look at the flap at the slit lamp for these changes. Occasionally, you’ll see changes in corneal topography, but by then the epithelial ingrowth has become fairly advanced. Looking for it early is very important.”
Managing epithelial ingrowth after an enhancement can be more complicated than after primary surgery, Dr. Manche notes. “It tends to be more recurrent than after the primary surgery,” he says. “I see a lot of patients sent to me for second opinions who’ve had either longstanding epithelial ingrowth or who’ve had one or two procedures to remove the ingrowth.”
In these cases, Dr. Manche lifts the flap, removes the epithelial ingrowth and uses adjunctive treatments, such as Tisseel glue or ReSure ocular sealant (Ocular Therapeutix), a polyethylene glycol hydrogel, to secure the flap in place. “In these cases, when you’ve had a recurrence, you really need to use the adjunctive treatments,” he notes. “I’ve had excellent results with both of those modalities. However, we occasionally get a case in which the epithelial ingrowth recurs even after we’ve used the adjuncts. In such a situation, I’ll suture the flap down. That’s the definitive treatment for epithelial ingrowth.”
Dr. Davis tries to avoid ingrowth at all costs. “I think the risk of epithelial ingrowth has motivated a lot of surgeons to move toward not lifting the flap,” she says. “That’s why more of us are choosing PRK to enhance these patients.” Once epithelial ingrowth takes hold, it can be very difficult to eliminate, she adds, noting, “even when you get rid of it, it tends to grow back and become a recurrent problem.”
In most cases, when she sees epithelial ingrowth, Dr. Davis says she lifts the flap and goes in with an instrument such as a PRK spatula. “I find it comes off easily in a sheet,” she says. “I also remove the epithelium beyond the perimeter of the flap for a couple of millimeters, and then remove the epithelium from the back of the flap when I position it down. I apply Tisseel fibrin glue over the whole surface and put a bandage contact lens over it. What I’m trying to do when using that technique is to give the flap a head start in sealing before the epithelium regrows, approaches the flap junction and dives under the edge of the flap.”
Other Sequelae
Besides epithelial ingrowth, refractive regression and other issues can challenge you after surgery.2 “When you’re evaluating a patient for regression, distinguish between progression changes and regression of effect,” says Dr. Manche. “If your patient is young, they may still be experiencing an increase in their axial myopia.”
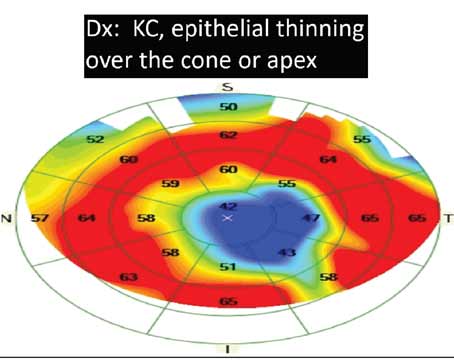
One way to be sure is to look at topography, he continues. “Let’s say you have a patient you performed LASIK on five years ago and you have yearly follow-up data. You need to evaluate any changes carefully. If topography shows that the keratometry values were K1 of 44 D by K2 of 44 D preop, K1 of 40 D by K2 of 40 D at one year postop and then K1 of 41 D by K2 of 41 D at five years postop, regression could be due to corneal epithelial hyperplasia. If the K readings are exactly the same as they were five years earlier, then the axial length is increasing, so it’s progressive myopia.
“There’s a difference,” continues Dr. Manche. “If it’s progression, and not just regression, you want to make sure the patient is stable. Consider having a couple of measurements many months apart to make sure the patient isn’t continually progressing. If it was regression or progression, but now it’s stable, I follow my usual protocol for performing an enhancement: At one to two years postop, a flap lift, provided the thickness of the cornea permits it; after two years postop, surface ablation.”
Dr. Davis watches closely for regression after PRK. “I’m not aware of any way to prevent it,” she says. “I’d say if you’re getting a lot of regression, you ought to reassess your treatment nomogram. Rather than basing it on one-month outcomes, perhaps you need to look at six-month or one-year outcomes and adjust the nomogram accordingly.”
Says Dr. Dhaliwal: “In terms of regression—as opposed to progression of myopia, or myopic progression due to a cataract—you really have to understand what’s going on with your patient. For example, in the case of a postop patient who truly has myopic regression within three months of surgery, if I think the patient was left with a primary undercorrection, then proceeding with an enhancement is reasonable. But to be honest, I have to say we’re not really seeing a lot of those cases anymore; our laser technology has gotten so much better.”
 |
In terms of progression of myopia over time, Dr. Dhaliwal adds, “if it’s only a small amount and a patient who’s nearing presbyopia needs just a bit of myopic correction for night-time driving, I often tell the patient to hold off. I discuss presbyopia and how he or she may hate wearing reading glasses more than wearing night-driving glasses. Discussing indications for a LASIK enhancement before doing the procedure is important.”
Dr. Dhaliwal also emphasizes the importance of avoiding ectasia, a major risk factor associated with enhancements. “You have to be aware of how much thickness is left,” she says. “If you don’t have the measurements of the stromal bed thickness, look at OCT measurements to understand the actual residual stromal bed thickness. I like to preserve 50 percent of the preop total corneal thickness or 250 microns, whichever is greater.”
She recommends the use of a Pentacam (Oculus) or other appropriate imaging technology to rule out elevations of the posterior cornea, such as what’s seen in forme fruste keratoconus. “I had a patient referred to me with significant post-LASIK ectasia that got a lot worse after her enhancement,” Dr. Dhaliwal recalls. “I later discovered she had pre-enhancement posterior elevation, as evidenced on topography and tomography. So, really, she shouldn’t have been referred for an enhancement. That’s a very important point. I also tell any patient on whom I’m doing an enhancement to refrain from eye rubbing postop, obviously, because rubbing the eyes contributes to the risk of ectasia.”
When using PRK for LASIK enhancements, Dr. Davis also watches for haze. If she sees it, she typically reduces her steroid treatment. “I don’t believe that issue is as common when you enhance a patient by lifting the flap,” she notes.
Prepare for Success
In most cases, surgeons say, if managed carefully, LASIK enhancements are effective and meet patient expectations.
“Laser vision correction is highly successful,” says Dr. Davis. “The vast majority of cases produce an excellent outcome after a single treatment. But like everything in medicine, there’s a Gaussian distribution. Just because 95 percent of patients need only a single treatment, obviously your patient isn’t one of them if he or she needs an enhancement. Emphasize that the patient is unique; it’s important to say that you can provide overall percentages, but not an individual percentage. There’s no way to determine preoperatively if your patient will be an under-responder or an over-responder on an individual basis.” REVIEW
Dr. Manche is a consultant for Allergan, Avedro, Zeiss and J&J Vision. He also provides sponsored research services for Allergan, Alcon, Avedro, Zeiss, J&J Vision and Presbia. He owns equity in RxSight and Vacu-Site. Dr. Dhaliwal is a consultant for Novartis, J&J Vision, Trefoil, receives lecture fees from Ocular Therapeutix and Starr Surgical and receives grant support Noveome. Dr. Davis reports no relevant commercial relationships.
1. Caster AI, Friess DW, Schwendeman FJ. Incidence of epithelial ingrowth in primary and retreatment laser in situ keratomileusis. J Cataract Refract Surg 2010;36:1:97-101.
2. Moshirfar M, Jehangir N, Fenzl CR, et al. LASIK enhancement: clinical and surgical management. J Refract Surg. 2017:1;33:2:116-127.