Clear lens extraction or refractive lens exchange has gained popularity in recent years for the treatment of patients with high degrees of myopia, hyperopia and astigmatism who are unsuitable for laser refractive surgery. Additionally, presbyopia treatment with RLE corrects refractive errors, while eliminating the need for cataract surgery.
“As technologies have improved, the patient population has expanded,” says Bloomington, Minnesota, surgeon Y. Ralph Chu. “Now, we can offer reading vision with RLE that can’t always be offered to presbyopic patients with LASIK. However, when performing RLE on myopes, you want to be aware of and discuss the risks of retinal issues with these patients. The low-hanging fruit are the hyperopes that aren’t candidates for LASIK. Now, presbyopia options with lens implants has expanded the patient base for RLE.”
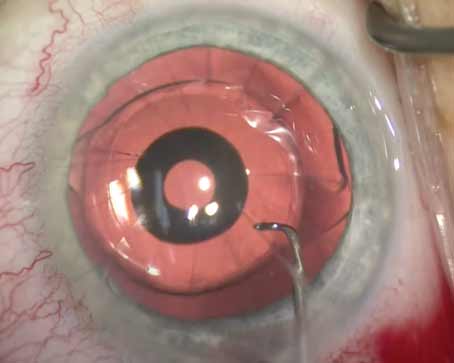
 |
| When doing RLE in a high myope, one potential risk is that the anterior chamber can get overly deep. Photo: Uday Devgan, MD. |
He adds that the quality of vision can be better with RLE than with LASIK, especially for patients with certain types of astigmatism or higher degrees of myopia or hyperopia. “That dictates a large part of the conversation. LASIK is also limited in that it doesn’t treat presbyopia beyond offering monovision in the United States, and so when patients want more than just distance vision, RLE enters the conversation,” Dr. Chu adds.
According to Daniel Durrie, MD, in practice in Overland Park, Kansas, RLE and laser refractive surgery are for different patient populations. “Laser vision correction, whether it’s SMILE, LASIK, or PRK, is really for congenital refractive errors, like myopia, astigmatism, and certain levels of hyperopia that people are born with,” he says. “Surgeons don’t start thinking about RLE until a patient is presbyopic. I think it should be discussed with patients older than 43 because, many times, it takes a couple of years for people to make the decision to have this kind of surgery because they haven’t thought about having their lens replaced, and they didn’t know it was an option.”
Who’s a Good Candidate For RLE?
Dr. Chu notes that prime candidates for refractive lens exchange are those patients who are out of the range of LASIK. “Higher hyperopes are prime candidates because they’re not the greatest LASIK candidates,” he avers. “Additionally, good RLE candidates are typically older than 50 years of age because IOLs offer presbyopia correction.”
He’s cautious with lower myopes (-2 D or lower), because these patients already have a good range of near vision, and the lens implant technologies still have the risk of some dysphotopsias and night-vision issues. “In our practice, it’s not an absolute contraindication, but there’s a longer discussion about the potential trade-offs and assessment in patients with low degrees of myopia,” he says.
John Hovanesian, MD, who is in practice in Laguna Hills, California, considers two criteria—age and refractive error—when looking at RLE as an option. “An older patient who is a +3 D or a +4 D is sometimes a better candidate for RLE than for laser refractive surgery,” he says. “Even if the refractive error is within the labeled indication of the laser, the quality of vision with hyperopic LASIK may not be good. Additionally, one might argue that the threshold goes down even below +4 D, especially with older age. As the patient approaches 50, hyperopic laser procedures really are less satisfying. There are exceptions, but most patients have some dysfunctional lens syndrome or early cataract signs that indicate the direction that their vision’s going. Obviously, accommodation is already partially lost by age 50, but lens clarity is beginning to decline as well, and that’s when we start to think about RLE.”
For patients with higher levels of myopia, the decision to pursue RLE has to be balanced against the risk of retinal detachment. “However, most patients who are highly myopic (in the range beyond where LASIK works well) have a posterior vitreous detachment that has previously occurred,” Dr. Hovanesian says, and any patient undergoing lens-based surgery who’s had a previous vitreous detachment is at significantly less risk for retinal detachment. So, although the traditional dogma is that higher myopes have a greater risk of retinal detachment, that’s not always the case if they’ve had a posterior vitreous detachment.”
Dr. Durrie adds that patients who are good candidates for RLE need to have a healthy tear film and no other ocular comorbidities that would prevent them from healing well. This includes significant iritis, corneal guttata or other conditions that would make a surgeon think twice about operating on either the lens or the cornea. “Uncontrolled glaucoma and uncontrolled diabetes are also contraindications to the procedure,” he adds. “Sometimes, we combine MIGS procedures with RLE, but, generally, the patient needs a healthy eye, a healthy tear film, and realistic expectations.”
Dr. Durrie underwent RLE in his nondominant eye 12 years ago to improve his near vision, and he just underwent RLE with a Light-Adjustable Lens on his dominant eye two months ago because he was starting to have decreased distance vision. “I was still 20/20 best-corrected, so I would be considered an RLE, not a cataract,” he says. “I was getting to the point where my quality of vision wasn’t as good, so I just had my lens replaced, and now I don’t need glasses at all. Another benefit is that RLE prevents cataracts, which is a big statement [for a patient]. We can replace your lens, improve your distance and near vision, and prevent cataracts. Many patients don’t realize that once you’ve had your lens replaced, you can’t get a cataract.”
Any premium IOL can be used for refractive lens exchange. Some surgeons who perform premium cataract surgery also perform RLE. “If you’re not doing premium cataract surgery, you’re probably not going to think about replacing somebody’s lens that doesn’t have a cataract yet, so the practice growth usually comes from premium lenses,” says Dr. Durrie. “Or, it can go the other way where you have a refractive surgeon who does corneal refractive surgery, does implantable contact lenses, and then decides to get into refractive lens exchange. I’ve had several practices do that lately, where they either brought in a surgeon to do those lens procedures or refreshed those skills from residency doing lens replacement. But, some purely corneal refractive surgeons that have been building up their practices are now adding RLE.”
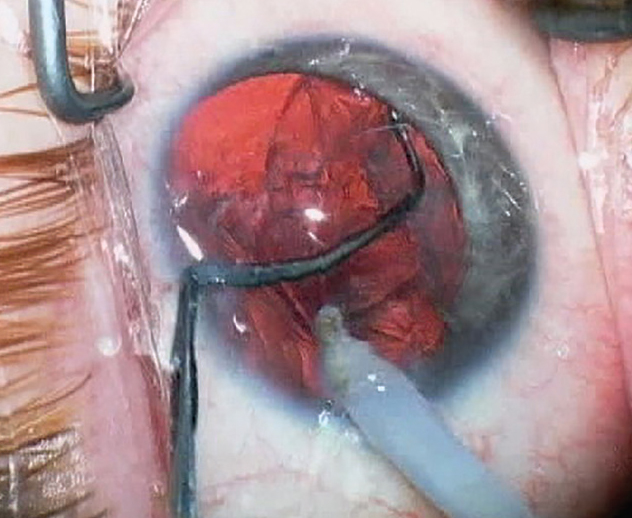
.png) |
| These are just some of the premium lenses surgeons can choose from for refractive lens exchange. |
ICLs
Dr. Hovanesian notes that laser refractive surgery and RLE aren’t the only options for patients. “The decision between laser refractive surgery and RLE isn’t binary, because there’s an in-between option with the implantable contact lens,” he notes. “Phakic IOLs have been around for decades, but a recent advance with the Staar ICL has made it even more patient-friendly. The EVO model, which has now been approved in the United States, has an opening in the center of the lens, so it’s no longer necessary to perform a peripheral iridotomy. It’s now a one-and-done type of procedure.
“Many surgeons are doing these bilateral sequential on the same day,” Dr. Hovanesian continues, “and some are performing them in office-based surgery centers rather than in outpatient ambulatory surgery centers, which means we can reduce some of the costs of anesthesia and facility fees, making it both more affordable and almost as simple as LASIK because it’s bilateral same-day.”
ICLs are only approved in the United States for myopic patients, and they offer the advantage of better-quality vision, especially for higher corrections, users say. “With LASIK, higher corrections have a more significant risk of causing aberrations that degrade the quality of vision,” Dr. Hovanesian adds. “With an ICL, those patients are in the sweet spot of that technology, and they really achieve better uncorrected vision after surgery than their best-corrected vision before surgery. That’s a big statement.”
Pros and Cons of RLE
According to Dr. Chu, the main downside of RLE is matching the right IOL technology to the patient’s needs.
With the multitude of intraocular lens choices, including monofocal IOLs, extended depth of focus, light-adjustable and accommodating, as well as multifocal lenses, preoperative education becomes the most critical component for selecting RLE for a specific patient. Understanding patients’ lifestyle needs, including whether or not they tolerate monovision, also helps guide which lens choices are a possibility as well if the patient is a good candidate for refractive lens exchange. “Therefore, it’s not just looking at a patient’s age and degree of refractive error, rather it’s understanding the strengths and weaknesses of each of the available lens technologies and matching it to the specific lifestyle needs and visual demands of each patient,” he says.
As IOL options have improved and surgery has become safer, this has allowed more patients to become candidates for lens replacement surgery at younger ages and at earlier stages in their dysfunctional lens syndrome journey. “Because of this, training the clinic staff and keeping up with the advances in the technologies has been the most challenging part in a surgical practice,” Dr. Chu adds.
Another downside is that it’s more invasive than laser refractive surgery, and most surgeons operate on one eye at a time. “It has all of the potential complications of an intraocular procedure, such as retinal detachment and endophthalmitis, which isn’t a meaningful risk with PRK and LASIK,” Dr. Hovanesian adds.
While it does have some downsides, it also has some significant benefits, proponents say. One advantage is that it’s the last eye procedure most patients will ever need. “It’s highly accurate, it obviates the future need for cataract surgery, and it can give the patient multifocality or a range of vision that LASIK can’t,” Dr. Hovanesian says. “LASIK is a depreciating asset for the patient. As the lens becomes more mature, the quality of vision changes, the refraction may shift, and the patient may lose accommodation. Whereas, with a lens-based procedure like RLE, the quality of vision typically improves immediately and stays that good for life. Patients don’t have to undergo future surgery, and most patients are very pleased with the range of uncorrected vision that they can achieve.”
According to Dr. Chu, an advantage of RLE is that a lens implant can be removed and exchanged if the patient is unable to adapt to unwanted visual side effects. The typical scenario involves exchange of a multifocal lens for a monofocal lens due to intolerance to dysphotopsia. A light-adjustable lens can also be considered as a replacement lens in this situation. “Exchanges are more straightforward when performed before YAG capsulotomy, but can also be done post-YAG capsulotomy,” he explains.
The Future
Dr. Chu notes that lens implants have been around since 1949. “Patients always ask about switching out their current lens if something better comes along in the future,” he says. “Right now, my answer is still most likely not. After a certain amount of time, it becomes more difficult to remove the lens, and most of the new lens technologies require a pristine capsular bag for stability and good outcomes. We tell patients that we usually have one chance to put in the best lens for your eye. Early on, lenses can be exchanged, but down the road, don’t expect that the lens implant can be swapped out like snow tires.”
Going forward, RLE may continue to grow in popularity.
“More people are becoming interested in refractive lens exchange because it’s a presbyopic solution,” says Dr. Durrie. “Presbyopia is a lens disease, not a corneal disease, so it should be treated with a lens exchange.”
Dr. Durrie is a consultant for RxSight, and Dr. Chu is a consultant for Carl Zeiss Meditec, Bausch and Lomb, and RxSight. Dr. Hovanesian has no relevant financial interests.