 |
Ptosis of the upper eyelid, or blepharoptosis, though ostensibly a straightforward problem, can actually be a challenge to diagnose and repair, thanks to its many possible causes and the strengths and weaknesses of the various surgical approaches. Here, I’ll provide advice on how to evaluate a case of acquired adult blepharoptosis, root out its cause and manage it successfully.
Anatomy
A review of the lid anatomy can help when planning blepharoptosis surgery. Elevation of the upper eyelid is a process controlled by three retractors. The first retractor, levator palpebrae superioris, is a striated muscle in the upper eyelid innervated by the oculomotor nerve and is primarily responsible for opening the eyelid. The second, Müller’s muscle, is a sympathetically innervated smooth muscle posterior to the levator and is responsible for about 2 mm of eyelid opening. Finally, the third and weakest retractor is the frontalis muscle in the forehead, which is innervated by the facial nerve, and can indirectly raise the upper eyelid by lifting the eyebrows. Any direct or indirect impact on these muscles can result in blepharoptosis.1
Classification
Ptosis can result from a number of causes, some of which are quite serious and warrant investigation. The condition can be unilateral or bilateral and can occur in varying degrees of severity that lead to cosmetic and/or functional deficits.
• Aponeurotic ptosis. This is the most common form of ptosis, and is due to chronic dehiscence of the levator aponeurosis due to normal aging changes. It’s usually bilateral but is often asymmetric. The changes to the muscle can be accelerated by common events such as long-term contact lens use or intraocular surgery. Despite the severity of the ptosis, the levator function often remains normal.2
• Myogenic ptosis. This form of ptosis stems from a myopathy, with the most common diagnoses being a chronic progressive external ophthalmoplegia (CPEO), myasthenia gravis, myotonic dystrophy or oculopharyngeal-muscular dystrophy (OPMD). The myopathy typically progresses, with worsening ptosis correlating with a decrease in levator function. The exception is myasthenia gravis, which is characterized by a fluctuating ptosis with variable levator function. These myopathies also tend to be associated with a constellation of systemic findings, such as a heart block along with CPEO in Kearns-Sayre syndrome, and dysphagia and proximal limb weakness with OPMD.3
• Neurogenic ptosis. This variety is uncommon but can signal a serious underlying issue. It can stem from a problem of the oculomotor nerve most commonly due to ischemia from diabetes, but can also indicate an aneurysm, stroke or tumor. A congenital or acquired form of Horner syndrome can also result in mild ptosis from Müller’s muscle being affected, and can be a manifestation of a stroke, tumor (including pulmonary tumors) or vascular disease. Aberrant regeneration of the facial nerve can result in a synkinetic ptosis associated with perioral contraction. A number of supranuclear conditions can also result in neurogenic ptosis as well, such as strokes, multiple sclerosis and brain injury.4-6
• Mechanical ptosis. This results from lesions in the lid either weighing it down or preventing it from lifting. Examples of such lesions include eyelid malignancies and symblepharon formation secondary to ocular cicatricial pemphigoid and Stevens-Johnson syndrome.3
• Traumatic ptosis. Traumatic ptosis can result from a variety of direct or indirect mechanisms, the most obvious being direct laceration of the lid muscles and nerves. It can also arise from blunt trauma, edema or hemorrhage that causes dehiscence of the levator.7
 |
Evaluation
A proper evaluation of the blepharoptosis patient includes a good history, clinical exam and an appreciation for what I call the eyelid “vital signs.”
• History. Patients with ptosis often report both cosmetic and functional complaints. Ptosis can diminish the peripheral visual field and can result in difficulty with daily activities of living. The “drowsy” appearance and the aging effect of ptosis are also bothersome for patients, especially if the case is asymmetric. The age of onset and the duration of the ptosis are also important, since they can indicate a more serious underlying problem. In such cases, seek out associated symptoms, such as diplopia, diurnal variation and trouble swallowing. Take a thorough ocular and medical history of the patient and the family, and note any history of surgery or trauma.
• Clinical exam. A full ophthalmic exam is warranted, watching for anomalous head positioning, facial asymmetry, synkinesis and abnormal speech. Neutralize any frontalis excursion to eliminate raised eyebrows so you can accurately assess the eyelid position.
Evaluate the acuity and pupil, paying special attention to the presence of anisocoria. Watch for strabismus in primary gaze and perform a thorough motility exam. Note other signs, such as Cogan’s lid twitch (overshooting of the upper lid from downgaze to upgaze) and von Graefe’s sign (lagging of the upper lid on downgaze). Rule out fatigable upgaze, supplementing your exam with an ice test if there’s a high level of suspicion for myasthenia gravis. Assess any proptosis or enophthalmos with an exophthalmometer, and perform a slit lamp exam, looking particularly for signs of dry eyes. Postpone your dilated fundus exam until you’ve done a full lid exam, since dilating eye drops (i.e., phenylephrine) can temporarily raise the lid position.
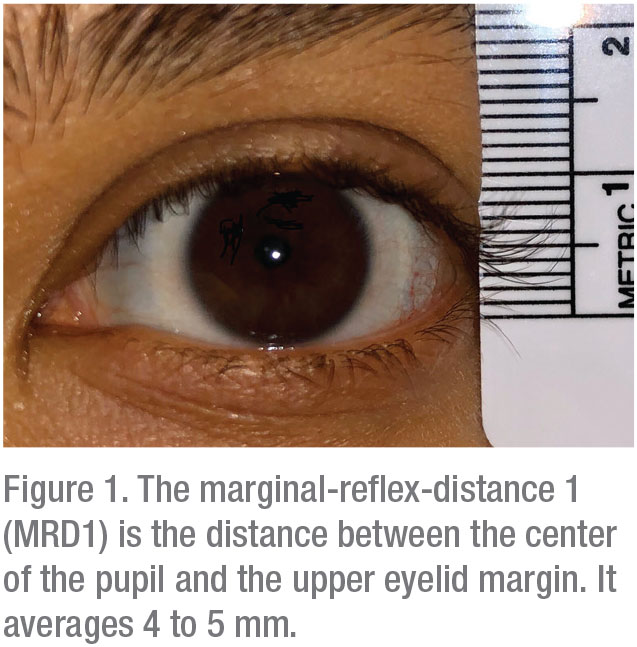
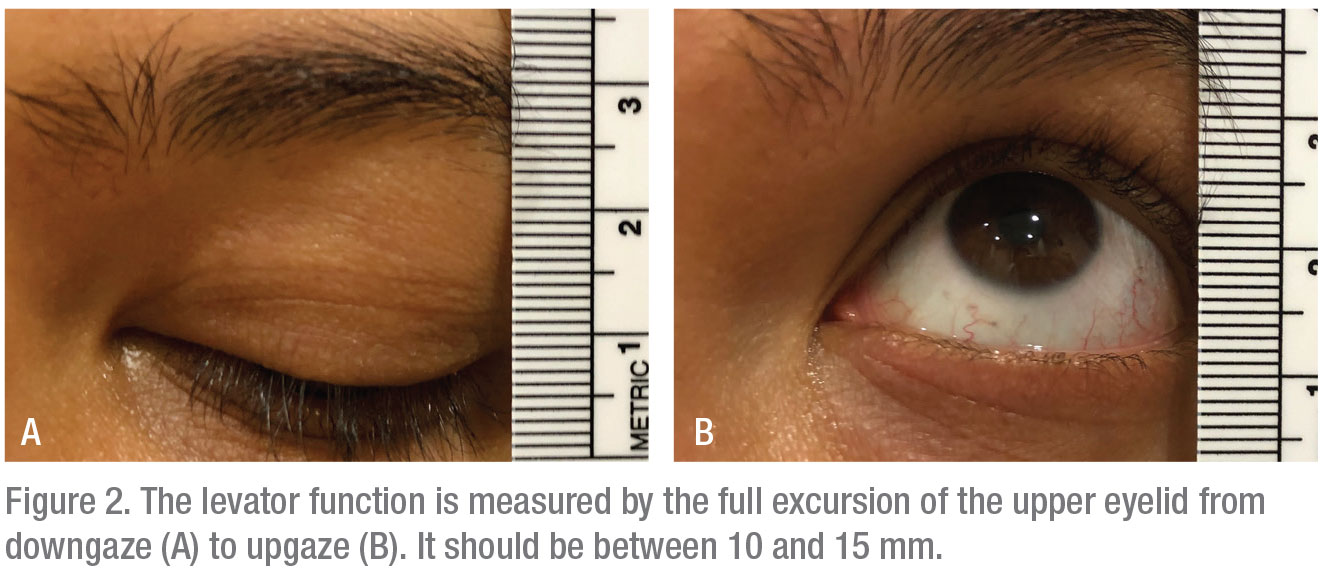
• Eyelid “vital signs.” The vertical palpebral fissure (the distance between the upper and lower lid margin) should be approximately 10 mm. The normal position of the upper lid margin is about 0.5 mm to 2 mm below the superior limbus. The marginal-reflex-distance 1 (MRD1) is the distance between the center of the pupil and the upper eyelid margin and averages 4 to 5 mm (Figure 1). The levator function is measured by the full excursion of the upper lid from downgaze to upgaze and should be between 10 to 15 mm (Figures 2A and 2B). Deviations from these average values confirm the presence of ptosis; an evaluation of the levator function can help to narrow down the etiology.8
• Ancillary testing. Initiate a workup if the underlying etiology is unclear. A basic workup can include a comprehensive metabolic panel, complete blood count, erythrocyte sedimentation rate and C-reactive protein. Thyroid function panel and acetylcholine receptor antibodies are common workups if thyroid disease and/or myasthenia gravis are suspected. In cases where a myopathy like CPEO is suspected, you can perform genetic testing, electromyography or even muscle biopsy. If orbital signs are present, including an abnormal pupil exam or other cranial neuropathies, neuroimaging may be in order. You can also order CTA or MRA if you suspect an aneurysm.3 If you suspect Horner syndrome, perform pharmacological testing as well.5
Non-surgical Treatment
Some cases of blepharoptosis don’t need surgery, and are better treated with the following approaches.
Observation is an acceptable response to entities such as traumatic ptosis or some forms of neurogenic ptosis (e.g., oculomotor palsy from ischemia), which can improve spontaneously. Observation can also be appropriate in cases of aponeurotic ptosis that don’t yet bother the patient.
Some cases respond best to a pharmacologic treatment. You should have optimal titration of systemic medication in myasthenia gravis patients and stability in thyroid patients prior to surgery. In cases of aberrant regeneration of the facial nerve resulting in synkinetic ptosis, botulinum toxin to the orbicularis oculi can improve the ptosis.66
Surgery
 |
Ptosis repair can be classified into anterior and posterior approaches.9 The etiology, severity of ptosis, and levator function will often determine the most appropriate method. Regardless of the technique, ptosis repair can be performed in the office setting with local infiltrative anesthesia, or in the operating suite, the latter typically involving sedation.
The anterior approaches consist of:
• External levator advancement. This is the most common procedure. Though it can address a wide range of ptosis, it relies on the presence of a functioning levator. In the procedure, the surgeon advances the attenuated or dehisced levator musculo-aponeurotic junction inferiorly onto the superior border of the tarsus.10 Small-incision techniques can offer the benefit of minimal scarring,11 but a traditional incision allows you to perform a simultaneous blepharoplasty (Figure 3).
• Frontalis suspension. This procedure is a great option when there’s minimal or no levator function.12 It allows you to bridge the frontalis muscle to the superior tarsal plate so that raising the brows will result in a more successful elevation of the lid. The bridging material can be autoplastic (i.e., autogenous tensor fascia lata) or alloplastic (i.e., silicone rods, alloderm). Alloplastic materials, especially silicone rods, are most widely used in adults due to their ease of placement and adjustability.13
If you feel a posterior approach would be better, consider:
• Müller’s muscle conjunctival resection (MMCR). This requires excellent levator function and is ideal for mild degrees of ptosis (1 to 2 mm). It does, however, require preoperative phenylephrine testing to ensure the viability of the Müller’s muscle and the ideal candidacy for MMCR. MMCR would be indicated if you measure 1 to 2 mm of elevation of the upper lid 10 minutes after instillation of 2.5% phenylephrine. Surgical resection ranges between 6.5 and 9.5 mm, following the 4:1 rule: Perform 4 mm of resection for every 1 mm of elevation.14-16 MMCR remains a popular choice for mild ptosis because it’s easy to perform and its results are predictable. Also, patients like that it doesn’t result in a visible scar. However, conjunctival scarring and contour issues can be problematic.
• Fasanella-Servat procedure. This procedure involves resection of the conjunctiva, Müller’s muscle and the superior border of the tarsal plate.17 The surgeon usually performs 1 mm of lift for every 2 mm of tarsectomy or 2 mm of conjunctival-Müller resection.18 It, too, offers the benefit of avoiding a scar. However, tarsal instability and resection of accessory lacrimal glands often lead to dry eye, so this procedure has fallen out of favor.19,20
Both anterior and posterior approaches are very successful in elevating the lid in the appropriate setting. Eyelid swelling, bruising, and varying degrees of discomfort are to be expected during the immediate postoperative period. Common complications include overcorrection, undercorrection, asymmetry and contour issues, thus making it one of the most challenging surgeries.3,12
In conclusion, though the cause of a patient’s blepharoptosis can be challenging to pin down, and you have to weigh the pros and cons of several surgical approaches, a thorough exam and careful surgery can usually help you achieve good results. REVIEW
Dr. Kim is an associate professor of Oculoplastics, Orbital and Cosmetic surgery at Emory University in Atlanta.
1. Sand JP, Zhu BZ, Desai SC. Surgical anatomy of the eyelids. Facial Plast Surg Clin N Am 2016; 24:89-95.
2. Godfrey KJ, Korn BS, Kikkawa DO. Blepharoptosis following ocular surgery: Identifying risk factors. Curr Opin Ophthalmol 2016;27:31-37.
3. Wong VA, Bechingsale PS, Oley CA, Sullivan TJ. Management of myogenic ptosis. Ophthalmology 2002;109:5:1023-31.
4. Averbuch-Heller L, Leigh RJ, Mermelstein V, et al. Ptosis in patients with hemispheric strokes. Neurology 2002;58:4:620-4.
5. Walton Kam, Buono LM. Horner Syndrome. Curr Opin Ophthalmol 2003;14:357-363.
6. Chen C, Malhotra R, Muecke J, et al. Aberrant facial nerve regeneration (AFR): An under-recognized cause of ptosis. Eye (Lond) 2004;18:2:159-62.
7. Jacobs SM, Tyring AJ, Amadi AJ. Traumatic ptosis: Evaluation of etiology, management, and prognosis. J Ophthalmic Vis Res 2018;13:4:447-452.
8. Neimkin MG, Holds JB. Evaluation of eyelid function and aesthetics. Facial Plast Surg Clin N Am 2016; 24:97-106.
9. Allen RC, Saylor MA, Nerad JA. Current state of ptosis repair: A comparison of internal and external approaches. Curr Opin Ophthal 2011;22:394-399.
10. Older JJ. Levator aponeurosis surgery for the correction of acquired ptosis. Analysis of 113 procedures. Ophthalmology 1983;90:1056-1059.
11. Frueh BR, Musch DC, McDonald HM. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology 2004;111:2158-2163.
12. Anh J, Kim NJ, Choung HK, et al. Frontalis sling operation using silicone rod for the correction of ptosis in chronic progressive external ophthalmoplegia. Br J Ophthalmol 2008;92:1685-1688.
13. Lamont M, Tyers AG. Silicone sling allows adjustable ptosis correction in children and in adults at risk of corneal exposure. Orbit 2010; 29:102-105.
14. Putterman AM, Fett DR. Muller’s muscle in the treatment of upper eyelid ptosis. Ophthalmic Surg 1986;17:354-360.
15. Weinstein GS, Buerger GF Jr. Modification of the Muller’s muscle-conjunctival resection operation for blepharoptosis. Am J Ophthalmol 1982;93:647-651.
16. Perry JD, Kadakia A, Foster JA. A new algorithm for ptosis repair using conjunctival mullerectomy with or without tarsectomy. Ophthal Plast Reconstr Surg 2002;18:426-429.
17. Fasanella RM, Servat J. Levator resection for minimal ptosis: another simplified operation. Arch Ophthalmol 1961;65:493-496.
18. North VS, Campbell AA, Callahan AB, et al. Enahanced Fasanella-Servat procedure for the graded repair of blepharoptosis. Ophthal Plast Reconstr Surg 2017;33:474-476.
19. Dailey RA, Saulny SM, Sullivan SA. Muller muscle-conjunctival resection. Ophthal Plast Reconstr Surg 2002;18:421-425.
20. Bodian M. Does conjunctival resection in ptosis surgery lead to dry-eye syndrome? Ann Ophthalmol 1989;21:213-216.



