Most refractive surgeons have experienced the thrill of having a patient see 20/20 after LASIK, only to have that thrill quickly fade as they realize that the patient is not happy with the outcome.
Patients can be 20/unhappy after refractive surgery for a variety of reasons, ranging from unrealistic expectations to dry eye to residual refractive error. In some cases, treatment is necessary, and in other cases, a wait-and-see approach is best.
Dry Eye
It is widely known that LASIK disrupts the tear film and causes dry eye, and this is a common cause of patient unhappiness. In a recent study, 20 percent of eyes undergoing LASIK experienced chronic dry eye that persisted for six months or more.1
In this retrospective case series, 190 eyes that underwent LASIK were examined for dry-eye syndrome. None of the eyes had dry-eye symptoms before surgery. Patients' mean age was 31 years. Assessments included subjective complaints of dry eye, tear breakup time, corneal staining, corneal sensitivity test and Schirmer I test. According to the study results, risk factors for chronic dry eye included higher attempted refractive correction, greater ablation depth and female gender.
According to David R. Hardten, MD, it is important to assess patients who are 20/unhappy for dry eye, because they may not specifically complain of dry-eye symptoms. "Patients can have 20/20 vision, but it can seem smeary or blurry to them. Having a poor tear film is like having a dirty windshield. Many times, people don't necessarily recognize their eyes as dry. They just notice that their vision fluctuates, and that it's blurry. We look for dry eye pretty aggressively, and we treat it aggressively if we find it," adds Dr. Hardten, who is in private practice at Minnesota Eye Consultants in
While many patients have dry eye that is induced by LASIK, others can have dry eye preoperatively. According to Dr. Hardten, assessing for dry eye preoperatively is imperative. "Clues to dry eye are contact lens intolerance, tired eyes and fluctuating vision with reading. Patients need to understand that LASIK will not make dry eye better. In fact, it can make it temporarily worse," he says.
Elizabeth A. Davis, MD, who is in practice with Dr. Hardten, agrees that the most common cause of patients being 20/unhappy is dry eye. "The tear film is an important refractive component of the ocular system," says Dr. Davis, who is director of the Minnesota Eye Laser and
Patients' tear film typically returns to normal four to six months after LASIK, and patients' dry-eye symptoms will improve. In the meantime, treatment may be needed. "I like to use Restasis (cyclosporine 0.05% ophthalmic emulsion) to treat these patients," says Karl G. Stonecipher, MD, who is director of the
Low-contrast
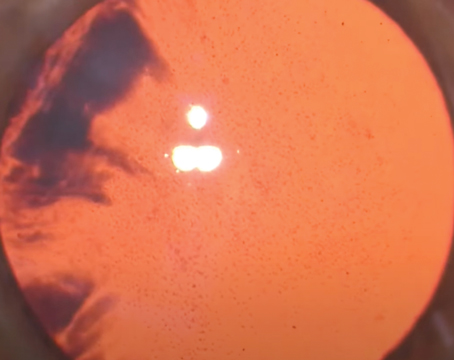
According to Dr. Stonecipher, another cause of patients being 20/unhappy after LASIK is reduced low-contrast vision, and he notes that patients' low-contrast visual acuity is often not measured after LASIK.
A study conducted at the Ohio State University found that clinically meaningful postoperative changes in low-contrast visual acuity were noted in patients undergoing LASIK and that these changes were more significant for high myopes, compared to low myopes.2
The study found that, for all subjects, surgery had a significant effect on nondilated low-contrast visual acuity. Pre-operative low-contrast visual acuity scores were significantly different from three-month and six-month scores for patients undergoing LASIK. Under dilated conditions, surgery had a significant effect on high- and low-contrast visual acuity. However, only changes in low-contrast visual acuity were clinically meaningful.
Additionally, a relationship has been established between ocular higher-order aberrations and contrast sensitivity after conventional LASIK. A Japanese study found that conventional LASIK significantly increases ocular higher-order aberrations, which compromises the postoperative contrast sensitivity function.3
This study included 200 eyes of 110 consecutive patients undergoing LASIK. Patients' mean age was 32.7 years. Ocular aberrations and contrast sensitivity function were determined before and one month after surgery. The amount of myopic correction ranged from 1 to 13 D.
The Hartmann-Shack wavefront analyzer was used to measure higher-order aberrations. The study found that LASIK significantly improved best-corrected visual acuity, but significantly reduced contrast sensitivity function and low-contrast visual acuity. Total higher-order, coma-like and spherical-like aberrations were significantly increased after LASIK. This study also found that eyes that achieved greater amounts of myopia correction had more significant changes in contrast sensitivity function and ocular higher-order aberrations.
Residual Refractive Error or Astigmatism
Even though they measure 20/20, many patients still have residual refractive error or residual astigmatism after LASIK. Dr. Davis notes that even patients with 20/20 acuity may have a small amount of myopia postoperatively, which can reduce nighttime visual acuity and lead to glare and haloes. "At night, when the pupil dilates and exposes more of the periphery of the crystalline lens, patients become even more myopic, compounding their pre-existing myopia. That reduces their acuity and leads to glare and haloes at night," she says.
She says that surgeons should look for residual refractive error because some patients can be 20/20 but have complaints due to a small refractive error, particularly if there is a disparity in acuity between the two eyes.
Another possibility, according to
"They may have been 20/15 preoperatively with contacts, especially if they were wearing rigid gas-permeable lenses, because these lenses provide the sharpest clarity," says Dr. Rajpal, who is in private practice at Cornea Consultants and See Clearly Vision Group in
Surgeons should evaluate patients' corneal topography to rule out irregularity or asymmetry in their corneal curvature. "The first thing we look at is topography," Dr. Rajpal says. "Second would be wavefront analysis to see if patients have higher-order aberrations that have been induced by the surgery. Sometimes, that can cause a distortion or it can cause patients' perception of their vision to not be clear even though they can still read 20/20 on the chart."
Other conditions, such as having the earliest stage of a cataract, can decrease quality of vision without limiting how well a patient can read the chart.
When to Retreat
Surgeons agree that retreating a patient who is 20/20 is not ideal and that the risks and benefits must be weighed carefully. In many instances, patients just need time to become accustomed to their surgical outcome.
"I don't typically operate on people who are 20/20 unless their complaints are significant, says Doug Katsev, MD, who is in private practice at the Sansum Santa Barbara Medical Foundation in California. "I really want these people to consider re-treatment carefully. For patients who are 20/20 and unhappy at distance and are 45-years-old and older, I carefully look at how well they can read. Some people who have a little bit of irregular astigmatism can still read well. You need to make sure that you don't give them perfect distance vision, because then their next complaint will be that they can't read. In saying that, I still have some incredibly happy patients who were 20/unhappy and, after a CustomVue re-treatment (Visx), are 20/20 ecstatic."
Dr. Davis notes that patients who are overcorrected need time to stabilize and possibly regress. If a patient's vision doesn't improve, she will then consider a hyperopic enhancement. Patients may also be 20/unhappy because of intolerance to monovision. "When doing monovision, it is important that the distance eye be as close to 20/20 as possible, because now they only have one eye for sharp acuity at distance," she says. "I'm much more likely to enhance an eye that is 20/25 at distance with monovision than I am in a patient who is bilateral distance and one eye is 20/20 and the other eye is 20/25."
She also explained that patients can undergo neuroadaptation after LASIK, but that it can take time. "Patients will sometimes just get used to their vision," she says. "Abrupt change is hard to deal with. Enhancements can't be done for quite a few months, so during that time, patients may adapt to their vision. Especially with monovision, patients need to get used to it. The brain pays attention to new things and changing things."
Dr. Rajpal agrees. He says that he only performs further surgical treatment if the patient has an irregular flap seen on topography or if wavefront analysis reveals a major aberration that needs to be treated. "Adaptation occurs over time, so patients adjust to how they are seeing," he says. "This is especially true with higher levels of correction. Patients' quality of vision and the way they are processing vision are very different after LASIK than they were with thick glasses or even contacts. Usually, adaptation takes between a few weeks and two to three months."
Dr. Stonecipher notes that patients with residual astigmatism of greater than 0.75 D tend to have more visual complaints. Research has shown that patients with 0.75 D or more of astigmatism tend to have decreased mesopic vision, so if the residual astigmatism is greater than 0.75 D, he will consider an enhancement.4
Preoperative Counseling
Surgeons feel that they and their staff are counseling patients to ensure appropriate expectations. Patients may rarely harbor inappropriate expectations nonetheless. "There are definitely high expectations out there, probably appropriately so, simply because the technology is that good and it does deliver excellent outcomes. Every now and then, you do have a patient who has inappropriate expectations," Dr. Davis says.
Dr. Hardten adds, "We tell patients that it won't be perfect for everyone, but every patient wants to be the one who ends up being perfect. It's really hard for patients to express their expectations. If a patient said the outcome had to be perfect or he or she would not be happy, then obviously we wouldn't do surgery. This is just one of those things that is almost impossible to counsel for preoperatively because patients get their expectations from their friends."
Regardless of the surgical outcome, some patients will never be happy. "A certain group of patients will just complain about anything. In those patients, I point out how well they are doing and how happy I am with their outcome," Dr. Katsev says.
1. Shoja MR, Besharati MR. Dry eye after LASIK for myopia: Incidence and risk factors. Eur J Ophthalmol 2007;17(1):1-6.
2. Bailey MD, Olson MD, Bullimore MA, Jones L, Maloney RK. The effect of LASIK on best-corrected high- and low-contrast visual acuity. Optom Vis Sci 2004;81(5):362-368.
3. Yamane N, Miyata K, Samejima T, et al. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci 2004;45(11):3986-3990.
4. Kezirian GM, Stonecipher KG. Subjective assessment of mesopic visual function after LASIK. Ophthalmol Clin North Am 2004;17(2):211-224.