|
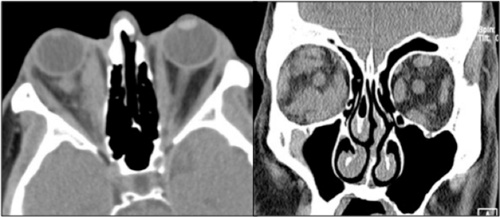
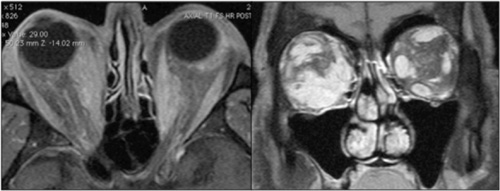
Review of the patient’s original CT scan demonstrated soft tissue abnormalities inconsistent with TED (See Figure 2). Because of these atypical findings, additional laboratory testing and neuroimaging was ordered. Thyroid function tests were within normal limits, as were thyroid stimulating immunoglobulin (TSI), angiotensin converting enzyme, and anti-neutrophil cytoplasmic antibody (ANCA). MRI showed enlarged right medial and inferior rectus muscles, with significant irregularity of the intraconal soft tissue (See Figure 3). On the left, there was enlargement of the medial rectus with nodularity of the muscle contour.
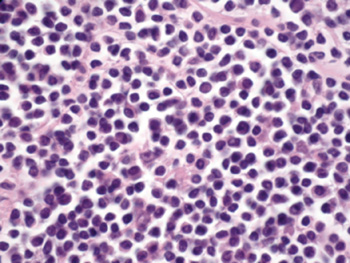
Given the atypical clinical and radiologic findings and lack of thyroid dysfunction, the patient underwent right orbitotomy with biopsies of the involved orbital fat and inferior rectus muscle.
Histopathology demonstrated an atypical lymphoid proliferation (See Figure 4). Flow cytometry confirmed a population of surface kappa-biased B cells positive for CD19 and CD20, and negative for CD5 and CD10. This was consistent with an extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (EMZL/MALT). The patient underwent PET/CT imaging for staging and was referred to an oncologist for further management. The PET/CT revealed increased standardized uptake values (SUVs) in the region of the extraocular muscles in addition to the left axillary lymph nodes, consistent with stage T2a EMZL/MALT.
Because of the stage of his disease, the patient underwent three cycles of systemic therapy with rituximab and bendamustine. Orbital swelling clinically improved and a repeat PET/CT demonstrated a decrease in both size and SUVs of the extraocular muscles and left axillary lymph nodes.
Discussion
The American Thyroid Association predicts that 12 percent of the U.S. population will develop thyroid dysfunction at some point in their lifetime. Depending on diagnostic criteria, up to 50 percent of patients with thyroid dysfunction will develop TED. Patients with TED may be euthyroid at presentation, but 25 percent will develop laboratory-evidenced thyroid dysfunction within one year, and 50 percent will do so within five years. Importantly, approximately 90 percent of patients with TED will demonstrate upper eyelid retraction on clinical exam, a feature notably absent in our patient.
|
Ocular adnexal lymphoma is a monoclonal proliferation of lymphoid cells, usually of B-cell origin. This is postulated to occur from dysregulation in immunomodulation and chromosomal mutations that eventually select for a predominant monoclonal population. The process appears be tied to either chronic antigenic stimulation or autoimmune disease. Monoclonality derives from a precursor B-cell (or T-cell) at a specific phase of maturation. Lymphoma subtypes can be classified according to the recently updated 2008 WHO classification. Importantly, each lymphoma subtype carries independent prognostic and treatment implications and should be considered as a distinct entity. Put succinctly, indolent ocular adnexal (OA) EMZL/MALT differs significantly from more aggressive and life-threatening subtypes, such as diffuse large B-cell and mantle cell lymphomas.
|
Newer therapies include immunotherapy (e.g., rituximab) and radioimmunotherapy, with further investigations under way. It is also important to remember that since OA-EMZL/MALT tends to follow a relatively indolent course, in some fragile, elderly patients with significant comorbidities, conservative observation is an acceptable alternative to systemic therapy. Ultimately, the single most important feature in the management of OA lymphoma is the subtype of the tumor.
Given the ubiquity of thyroid dysfunction in the general population and the fact that the majority of extraocular muscle enlargement is indeed due to TED, it is not surprising that ophthalmologists generally ascribe all muscle enlargement to TED.
Alternative diagnoses should be considered when the patient exhibits atypical clinical or radiologic features, including persistent euthryoidism, lack of upper eyelid retraction or adduction deficits on extraocular motility examination (the vast majority of TED external ophthalmoplegia presents with some combination of abduction and vertical duction deficits). Atypical radiologic features on CT or MRI include isolated lateral rectus muscle enlargement, nodularity of the enlarged muscles (“bumpy muscles”) or significant infiltration of the intraconal fat. In such cases, biopsy of the involved tissue should be strongly considered before instituting empiric corticosteroid or radiation therapy.
The author would like to thank Jurij R. Bilyk, MD, of the Oculoplastic and Orbital Surgery Service and Ralph C. Eagle Jr., MD, of the Ocular Pathology Service.
1. American Thyroid Association: www.thyroid.org/about/pressroom.html.
2. Bartley GB, Fatourechi V, Kadrmas EF, et al. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 1996;121:284-90.
3. Lacey B, Chang W, Rootman J. Nonthyroid causes of extraocular muscle disease. Surv of Ophthalmology 1999;44(3):187-213.
4. Murchison AP, Bilyk JR. Ocular Adnexal Lymphoproliferative Disease. In Black EH, Nesi FA, Calvano CJ, Glastone GJ, Levine MR (Eds.). Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. New York: Springer, 2012:959-92.
5. Politi LS, Forghani R, Godi C, et al. Ocular adnexal lymphoma: diffusion-weighted MR imaging for differential diagnosis and therapeutic monitoring. Radiology 2010;256(2):565-74.
6. Stefanovic A, Lossos IS. Extranodal marginal zone lymphoma of the ocular adnexa. Blood 2009;114(3):501-10.
7. Slamovits TL, Burde RM. Bumpy muscles. Surv of Ophthalmology 1988;33(3):189-99.
8. Watkins LM, Carter KD, Nerad JA. Ocular Adnexal Lymphoma of the Extraocular Muscles: Case Series From the University of Iowa and Review of the Literature. Ophthal Plast Reconstr Surg 2011;27(6):471-76.