Presentation
A 16-year-old Caucasian male presented to the Wills Eye Emergency Room with bilateral ocular irritation. Redness, foreign body sensation and crusting started in the right eye six days prior and then spread to the left eye four days later. This was associated with skin lesions over the forehead, cheeks, posterior occipital region, and bilateral upper and lower eyelids. Two days earlier, his primary ophthalmologist suspected vernal conjunctivitis and started prednisolone acetate hourly, moxifloxacin four times daily and olopatadine ophthalmic drops in both eyes. In addition, his dermatologist took cultures of the skin lesions and his pediatrician started him on oral amoxicillin. On review of systems, he noted a sore throat, cough, fever, nausea and general malaise.
Medical History
The patient’s past ocular history was significant for soft contact lens use. His past medical history was significant for acne and seasonal allergies. His chronic medications included isotretinoin and occasional oral antihistamines. He was up-to-date on his immunizations, including herpes zoster. He denied sexual activity, alcohol, tobacco or recreational drug use. He did not have pets at home, had no recent travel, but did play multiple sports including wrestling, football, baseball and weightlifting.
Examination
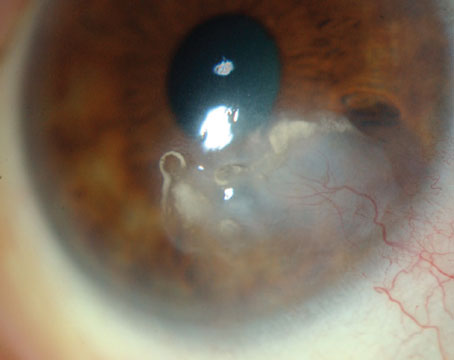
The patient had a corrected visual acuity of 20/40, pinhole to 20/30 in the right eye and 20/30 in the left eye. He had normal pupils. Goldmann applanation tonometry intraocular pressures were 12 mmHg in both eyes. External evaluation revealed posterior occipital, cervical and pre-auricular tender lymphadenopathy. There were honey-crusted lesions over the mid-forehead, upper and lower lids, upper cheeks, and posterior neck (See Figure 1). A survey of his arms, legs and abdomen revealed no additional skin lesions. He had giant papillae of the superior palpebral conjunctiva and follicles on both lower lids (See Figure 2). Corneal sensation was intact. The conjunctiva was injected bilaterally with corneal dendrites seen near the limbus (See Figure 3). He was noted to have patchy subepithelial infiltrates in both eyes without anterior chamber reaction. The dilated funduscopic exam was normal, without retinal necrosis.
|
What is your differential diagnosis? What further workup would you pursue?