A. No. Several influences affect the 2016 MPFS. The 2016 conversion factor published in November was $35.8279, which was a slight decrease from the 2015 conversion factor of $35.9335. It included a budget neutrality adjustment of -0.02 percent, an increase of 0.5 percent resulting from the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and a 0.77 percent target recapture amount (decrease) from the Achieving a Better Life Experience (ABLE) Act of 2014. Relative value unit changes occurred at the beginning of January (see below left). The January fee schedule update reduced the conversion factor to $35.8043. The end result is an approximately 1 percent reimbursement reduction for ophthalmology services overall.
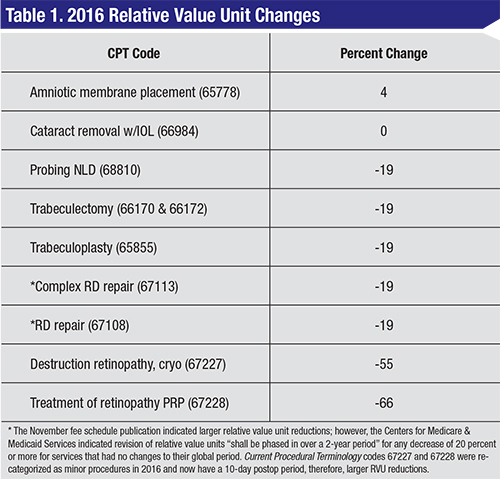
Q. What type of relative value unit changes occurred on January 1, 2016?
A. Several changes exist in the Medicare Physician Fee Schedule, published in January. See Table 1, left, for examples of some RVU changes and the percentage of change from 2015.
Q. What is the target recapture?
A. In the Protecting Access to Medicare Act of 2014, Congress set a target for adjustments to misvalued codes for calendar years 2017 to 2020. The target was 0.5 percent of the estimated expenditures under the MPFS for each of the four years. The ABLE act moved up the timeline and target to apply the adjustments for 2016 through 2018. It set the target to 1 percent for 2016. If the net reductions in misvalued codes in 2016 were not equal to or greater than 1 percent of the estimated expenditures under the fee schedule, a reduction equal to the percentage difference between 1 percent and the estimated net reduction in expenditures resulting from misvalued code reductions must be made to all MPFS services. The net reduction resulting from relative value unit adjustments is 0.23 percent for 2016. The target was missed by 0.77 percent, resulting in reductions to the MPFS in 2016.
 |
Q. What happened with ambulatory surgery center facility fees in 2016?
A. For 2016, the wage adjustment for budget neutrality, in addition to the multifactor productivity adjusted update factor, increases the ASC conversion factor by 1.3 percent for those meeting the quality reporting requirements, resulting in small increases in facility reimbursement. Ambulatory surgical centers began the reporting of National Quality Forum Measures in October 2012. The reporting of these measures affects reimbursement. Nonparticipation or failure to meet the necessary requirements results in a 2-percent reduction to facility Medicare reimbursement.
Q. Did hospital outpatient department rates increase similarly to ASC facility rates?
A. No. Various adjustments to hospital reimbursements result in a hospital outpatient department rate decrease of -0.3 percent.
Q. Were there any Category III code changes published in 2016?
A. There were a number of changes. Code changes are released semiannually by the American Medical Association; a new Category III code implemented on July 1, 2015 appears in the Current Procedural Terminology 2016 handbook:
• 0402T – Collagen cross-linking of cornea (including removal of the corneal epithelium and intraoperative pachymetry when performed) (Do not report 0402T in conjunction with 65435, 69990, 76514).
One revised Category III code exists in 2016, with additional verbiage underlined below:
• 0308T – Insertion of ocular telescope prosthesis including removal of crystalline lens or intraocular lens prosthesis.
Coverage and payment for Category III codes remains at the discretion of the Medicare Administrative Contractor.
Q. What changes were published with Category I codes in CPT 2016?
A. The 2016 CPT coding manual contains a number of new codes, revisions, and deletions applicable to ophthalmology. Category I CPT code changes are as follows:
New code:
• 65785 – Implantation of intrastromal corneal ring segments, replaces 0099T.
Revised codes:
 |
• 65855 – Trabeculoplasty by laser surgery;
• 67227 – Destruction of extensive or progressive retinopathy (e.g., diabetic retinopathy), cryotherapy, diathermy;
• 67228 – Treatment of extensive or progressive retinopathy (e.g., diabetic retinopathy), photocoagulation.
The “one or more sessions” verbiage was removed from these three procedures.
The following codes contain language changes reflected by underlines:
• 67101 – Repair of retinal detachment, 1 or more sessions; cryotherapy or diathermy, including drainage of subretinal fluid when performed;
• 67105 – photocoagulation including drainage of subretinal fluid, when performed;
• 67107 – Repair of retinal detachment; scleral buckling (such as lamellar scleral dissection, imbrication or encircling procedure), including, when performed, implant, cryotherapy, photocoagulation, and drainage of subretinal fluid;
• 67108 – … with vitrectomy, any method, including, when performed, air or gas tamponade, focal endolaser photocoagulation, cryotherapy, drainage of subretinal fluid, scleral buckling, and/or removal of lens by same technique;
• 67113 – Repair of complex retinal detachment … with vitrectomy and membrane peeling including, when performed, air, gas, or silicone oil, tamponade, cryotherapy, endolaser photocoagulation, drainage of subretinal fluid, scleral buckling, and/or removal of lens;
• 99174 – Instrument-based ocular screening (e.g., photoscreening, automated-refraction), bilateral; with remote analysis and report.
These changes do not affect reimbursement.
Deleted in 2016:
• 67112 – by scleral buckling or vitrectomy on patient having previous ipsilateral retinal detachment repair(s) using scleral buckling or vitrectomy techniques.
Q. Were there any changes to diagnosis codes or issues with the implementation of ICD-10?
A. No new ICD-10 codes were published in October 2015. Since implementation on October 1, 2015, the ICD-10 transition has been relatively smooth. Contractor policies continue to be updated with missing ICD-10 codes not brought forward from the ICD-9 covered lists. Claim denials due to this issue should be brought to the attention of the payer and appealed.
Q. What types of regulatory issues were identified in the annual Office of Inspector General’s Work Plan as areas of concern for ophthalmology in 2016?
A. The annual publication of the OIG Work Plan included a series of initiatives that will continue in 2016 with a small number of new initiatives pertinent to ophthalmology. The continuing targets for scrutiny include:
• Payments for drugs;
• Ambulatory surgical centers – payment system;
| Eligible professionals who did not successfully report PQRS in 2014 are penalized 2 percent …in 2016. |
• Anesthesia services – payments for personally performed services.
New issues include:
• Anesthesia services – non-covered services;
• Physicians – referring/ordering Medicare services and supplies;
• Prolonged services – reasonableness of services;
• CMS management of the ICD-10 implementation;
• Ambulatory surgery centers – quality oversight; and
• Risk adjustment data – sufficiency of documentation supporting diagnoses.
Q. Are there penalties and/or bonus dollars for participation in the Physician Quality Reporting System in 2016?
A. The Patient Protection and Affordable Care Act made PQRS mandatory by 2015. Those eligible professionals who did not successfully report PQRS in 2014 are penalized 2 percent off of their MPFS reimbursements in 2016. Bonus payments ended with the 0.5-percent bonus paid to successful reporters in 2014.
Q. Are there any major changes to PQRS reporting requirements in 2016?
A. No. The requirements for successful reporting in 2016 are unchanged from 2015. Eligible professionals must include at least nine measures via claims and/or registry-based reporting covering at least three National Quality Strategy domains. In 2016, one measure must be from the cross-cutting measure set. Eligible professionals reporting fewer than nine measures are subject to the Measure Applicability Validation process to determine if additional measures apply. The MAV process may determine that the eligible professional successfully reported even though nine measures were not reported.
Q. Are there continued penalties for those without electronic health records or those that fail to successfully report meaningful use?
A. Yes. For those without EHR and those who did not qualify for a hardship exemption or complete their meaningful use attestation for 2014, a penalty of 2 percent of their MPFS applies for 2016.
Q. What Medicare Part B changes affect beneficiaries in 2016 from a cost perspective?
A. The Medicare Part B premiums remain $104.90 for most beneficiaries. The Part B deductible increases to $166. This is the first deductible increase since 2013. REVIEW
Ms. McCune is vice president of the Corcoran Consulting Group. Contact her at DMcCune@corcoranccg.com.



