This year some new eye-care CPT codes went into effect on January 1, 2021. Though there aren’t as many new codes as in years past, they’re important. (As always, be sure and use codes and their related guidelines in effect for that date-of-service [DOS]).
In this installment of Medicare Q&A, we’ll review the new 2021 eye-care CPT codes and some of the key things to know about them. We’ll also discuss the (actual) final Medicare Physician Fee Schedule (MPFS) changes as those are significant too.
What are the CPT Category I code changes that went into effect last month that might affect eye care?
Regarding exams, as we discussed in a previous article, CMS implemented a new set of rules for office or other outpatient evaluation and management services (9920x, 9921x). The definitions for E/M codes within CPT have been changed to emphasize medical decision-making and to give physicians the option to select a level of service based solely on physician time spent (uncommon for most of eye care). The actual E/M exam code numbers didn’t change. Code 99201 has been deleted (but it was rarely, if ever, used by eye doctors anyway). No changes will be made to the requirements for eye codes (920xx). (For more information on this topic, refer to our column in the November 2020 issue of Review.)
The “finally final” 2021 MPFS published in early January assigns higher values to E/M codes than the corresponding eye codes, which strongly suggests reversing the traditional preference for eye codes over E/M codes. The differences are most stark on established patients, for whom you may wind up using different codes than you have in the past or with certain payers.
For infrequent situations where the physician spends more time tending to a patient than 60 to 74 minutes (for a new patient) or 40 to 54 minutes (for an established patient), CPT created a new add-on code, +99417, for prolonged services. The code description reads:
Prolonged office or other outpatient E/M service(s) beyond the minimum required time of the primary procedure which has been selected using total time, requiring total time with or without direct patient contact beyond the usual service, on the date of the primary service, each 15 minutes of total time.
- List separate in addition to 99205, 99215;
- Do not report 99417 for any time unit less than 15 minutes
CMS didn’t accept CPT’s definition for +99417, so they created their own HCPCS code, G2212 instead. The code descriptor is similar but has a significant difference (note the use of the phrase “beyond the maximum” in the description):
Prolonged office or other outpatient evaluation and management service(s) beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service; each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact. (List separately in addition to CPT codes 99205 or 99215 for office or other outpatient E/M services.)
The difference between the two is the starting point for prolonged services. In the Medicare definition, you start only at the “maximum required time” for the primary procedure (level 5 exam). Of course, for Medicare claims, use the Medicare code G2212 instead of 99417.
In terms of other codes, the CPT code for UBM (anterior segment ultrasound 76513) has been revised. It’s now a “unilateral or bilateral” code. On 2021 claims for reimbursement, bill it once per patient on a day, and not once per eye as it was billed in 2020.
The section of CPT devoted to remote imaging of retina was thoroughly revised (i.e., 92227, 92228) and appended (i.e., 92229).
- 92227: Imaging of retina for detection or monitoring of disease; with remote clinical staff review and report, unilateral or bilateral;
- 92228: with remote physician or other qualified health care professional interpretation and report, unilateral or bilateral;
- 92229: point-of-care automated analysis and report, unilateral or bilateral
These codes aren’t to be reported on claims in conjunction with other in-office imaging services such as posterior segment OCT or fundus photography.
In the midst of the public health emergency due to COVID-19, CPT created 99072, covering:
- Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a Public Health Emergency as defined by law, due to respiratory-transmitted infectious disease.
Medicare treats personal protective equipment (and therefore the code) as an incidental expense and doesn’t pay for it separately.
What about Category III CPT codes in 2021?
There are new codes for remote imaging with OCT performed at home.
- 0604T: Optical coherence tomography (OCT) of retina, remote, patient-initiated image capture and transmission to a remote surveillance center, unilateral or bilateral; initial device provision, set-up and patient education on use of equipment;
- 0605T: remote surveillance center technical support, data analyses and reports, with a minimum of 8 daily recordings, each 30 days;
- 0606T: review, interpretation and report by the prescribing physician or other QHP of remote surveillance center data analyses, each 30 days
There is also a new code for eye movement analysis for concussion.
- 0615T: Eye-movement analysis without spatial calibration, with interpretation and report
There are three new codes for use when an artificial iris is implanted. While they’re each for a specific phakic-or-not status, all three go with the already existing HCPCS code for the related device C1839 (iris implant).
- 0616T: Insertion of iris prosthesis, including suture fixation and repair or removal of iris, when performed; without removal of crystalline lens or intraocular lens, without insertion of intraocular lens;
- 0617T: with removal of crystalline lens and insertion of intraocular lens;
- 0618T: with secondary intraocular lens placement or intraocular lens exchange
There are two new codes to report laser trabeculostomy, with or without endoscopy, a new MIGS procedure currently in clinical trials.
- 0620T: Trabeculostomy ab interno by laser;
- 0621T: with use of ophthalmic endoscope.
- Do not report in conjunction with 92020.
I heard that Omidria (Omeros) still has coverage in 2021. Is that true?
Yes, but it is different in a subtle way. In the final rule for the Outpatient Prospective Payment System (OPPSA), CMS stated that Omidria (J1097) qualifies as of October 1, 2020 for separate payment in ASCs, but is now under the policy for non-opioid pain surgical management.
What about ICD-10 in 2021?
New 2021 ICD-10-CM codes went into effect on October 1, 2020. Below is a list of the new and revised codes by chapter in ICD-10-CM for conditions that you might encounter:
Chapter 3. Diseases of the Blood and Blood-Forming Organs and Certain Disorders Involving the Immune Mechanism (D50-D89) - D57: Sickle-cell. (Increased specificity)
Chapter 7. Diseases of the Eye and Adnexa (H00-H59)
- H18.5: Hereditary Corneal Dystrophies (This area includes Fuchs’ and some others. All the existing codes in this area gained laterality.)
- H55.8: Deficient smooth pursuit eye movements. (This is a 4 character code and has no laterality.)
Chapter 18. Symptoms, Signs, and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified
- R51: Headache (this can no longer be “just” a 3-character code.)
Chapter 19. Injury, Poisoning and Certain Other Consequences of External Causes (S00-T88)
- T86.84: Corneal Transplant (Every code in this set gained a 7th character for laterality.)
Chapter 20. External Causes of Morbidity (V00-Y99). These codes are only required on claims if the payer demands them (Medicare does not).
- Y77.11: Adverse incidents with contact lenses;
- Y77.19: Adverse incidents with other ophthalmic devices.
Chapter 21. Factors influencing health status and contact with health services (Z00-Z99).
- Z03.82: Encounter for observation for suspected inserted (injected) foreign body ruled out (Gained laterality).
- Z88: Allergy status. (Minor changes in wording.)
Chapter 22. Codes for Special Purposes (U00-U85).
- U07.0: Vaping-related disorders;
- U07.1: COVID-19 (This code is more specific than existing code B34.2, coronavirus infection, and should be used for SARS-CoV-2 disease only.)
What about the physician reimbursement under Medicare for 2021?
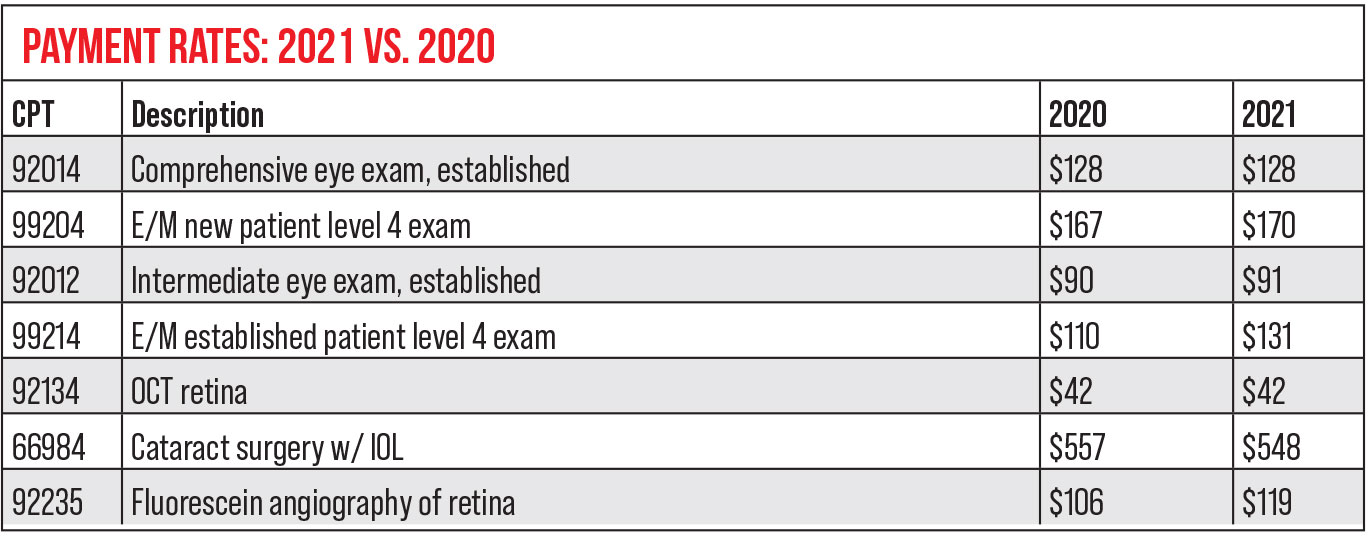
The table below has a comparison of 2020 to 2021 national payment rates on some common codes after Medicare published the final physician numbers in early January that included a one-time infusion of billions of dollars and the three-year hold on implementation of the “Complex patient” add-on code G2211 into the system; before these two major changes, eye doctors would have taken a much larger hit.
The other big potential change is the “Most Favored Nation” drug model for Part B drugs used in the office. It would only affect three of our drugs, Lucentis, Eylea and Botox, but the rule is currently in abeyance due to a court order through at least January 26, 2021. (More to come later in the year.)
For facilities, what are the biggest Medicare changes in 2021?
For CY 2021, Medicare increased the ASC conversion factor by 2.4 percent. While the Quality Reporting program threatens payment reductions for those not meeting the requirements, they stipulated that no ASCs will get a reduction in 2021 in light of the pandemic. (Few ASCs get the penalty anyway since they meet the Quality requirements.) CMS increased reimbursement for hospital outpatient departments by the same 2.4 percent. Most code payments are pretty flat in 2021, but blepharoplasty (15823), laser PI (66761), iStent/Hydrus (0191T) and cataract/IOL surgery all went up for each facility type.
 |
What about changes to Medicare beneficiaries’ obligations and other administrative changes for my office?
The 2020 Medicare Part B deductible rose to $203, so you’ll need to collect for this greater amount beginning in January. In 2020 this was $198. For information on the revised Advance Beneficiary Notice of Noncoverage, see the Medicare Q&A in the September 2020 issue of Review.
I have a lot more Part C (Medicare Advantage) patients than ever before and wondered if it’s just in my area.
You’re not alone; and signs point to this trend continuing. The Congressional Budget Office estimated that the enrollment will continue to rise to about 51 percent of eligible beneficiaries by 2030.
I just revalidated with Medicare and, when I did, the CMS files didn’t reflect the change. Is there something I missed in the new 2021 regulations?
During the pandemic, CMS hasn’t enforced its regulations on revalidation. After the public health emergency (PHE) declaration ends, be sure to check your status again, because deactivations will resume soon afterwards according to Medicare. In the meantime, you can still revalidate as you noted you did, but the site won’t reflect your activity. Print and save your finalized recognition. Remember that failure to revalidate once the PHE ends could result in a hold on your Medicare payments or deactivation of billing privileges.
Are there any significant changes in the Quality Payment Program (QPP) or the Merit-based Incentive Payment System (MIPS) this year?
Yes, and they’re important but mostly related to the scores you need to get.
The QPP continues and there are only modest revisions to the MIPS that most providers use. The maximum negative payment adjustment will remain at 9 percent for the Medicare payments you get in 2023 (from reporting in 2021), although the minimum composite score you need to achieve in order to avoid a penalty has risen a lot, all the way to 60 points from the 45 you needed last year. This change may make it more difficult for providers and practices to earn a bonus. Additionally, if CMS allows another MIPS Hardship exception for COVID-19, there won’t be as many penalized. Also, since the MIPS program is designed to be budget-neutral, fewer penalties means those that do well won’t get as much as they might otherwise.
Exceptional bonuses remain excluded from this budget-neutral calculation, but providers must achieve 85 points, which is potentially more difficult for cataract surgeons due to the Routine Cataract w/ IOL Implantation cost measure still in effect.
In MIPS, there have been changes in the weighting of the “Quality” and “Cost” measures for 2021. This year, they change from 45 percent for Quality and 15 percent for Cost to 40 percent and 20 percent, respectively. The current regulation has them both becoming 30 percent in 2022, which may make high scores and bonuses even more difficult to get. Last year, CMS put the new MIPS Value Pathways system on hold and has done so again for 2021.



