 |
This year we have some new CPT Category I and Category III codes effective for use in eye care on January 1, 2022. We also have changes to several codes. The impact of the Medicare Physician Fee Schedule especially seems to have negatively impacted payment in the glaucoma laser and surgery area.
While Medicare has reduced the values on many of our commonly used codes, it is possible Congress will act in late December or in the first part of the year to mitigate some of the cuts —so reimbursement values might rise after this article is published (they shouldn’t go down any further, though).
(Note: There aren’t many updates to ICD-10 for eye care in 2022, and we covered those in our November 2021 column.)
Q: What are the CPT Category I code changes that go into effect on January 1, 2022 that might affect eye care?
In terms of exam coding, last year we had a momentous change to E/M coding. Though the effect of that change remains, we’d all like to see a bit more clarity in some circumstances; but we’ll have to wait and see. The Eye exam codes remain unchanged for coding. 99211 had a small change in the code descriptor, but we’ll see if it turns out to be significant. Any words deleted in the language for codes shown in this article are in strikethrough text:
• 99211 Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional. Usually, the presenting problem(s) are minimal
In terms of new codes, we have three of importance and a fair number of changes to code descriptors. The new codes are:
• 68841 Insertion of drug-eluting implant, including punctal dilation when performed, into lacrimal canaliculi, (each)
The above code has a parenthetical instruction to report the actual drug-eluting implant separately.
• 66989 Extracapsular cataract removal w/IOL insertion, complex; with insertion of intraocular (e.g., trabecular meshwork, supraciliary, suprachoroidal) anterior segment aqueous drainage device, without extraocular reservoir, internal approach, one or more
• 66991 Extracapsular cataract removal w/IOL insertion; with insertion of intraocular (e.g., trabecular meshwork, supraciliary, suprachoroidal) anterior segment aqueous drainage device, without extraocular reservoir, internal approach, one or more
Both 66989 and 66991 are combination codes (they take two codes and combine them into a single code). In 2022, the pair only apply to devices such as iStent or Hydrus and there are some important Category III code changes that accompany them. Note also that you will no longer be able to code for more than one device or device insertion as that is baked into the new codes. The revised codes are:
• 67141 Prophylaxis of retinal detachment (e.g., retinal break, lattice degeneration) without drainage, one or more sessions; cryotherapy, diathermy
• 67145 Prophylaxis of retinal detachment (e.g., retinal break, lattice degeneration) without drainage, one or more sessions; photocoagulation
• 92065 Orthoptic and/or pleoptic training, with continuing medical direction and evaluation
 |
| Click image to enlarge. |
Q: What about Category III CPT codes in 2022?
We have three codes related to the new combination codes above; there is one new code—which has the “multiple devices” caveat as above—and two deleted codes. The new code, though valid, has the subtlety of being an off-label use of the only two valid devices, so it’s not likely to be payable under coverage policies until the manufacturers can change their approved FDA labeling. The codes are:
• 0671T Insertion of anterior segment aqueous drainage device into the trabecular meshwork, without extraocular reservoir, and without concomitant cataract removal, one or more
The pair of related but deleted codes:
• 0191T Insertion of anterior segment aqueous drainage device, without external reservoir; internal approach, into the trabecular meshwork
• +0376T Insertion of anterior segment aqueous drainage device, without extraocular reservoir; internal approach, into the trabecular meshwork; each additional device insertion
There’s not much information on what devices or material goes with the below codes at this point, but the codes are “live” nonetheless. Other new Category III codes for 2022 are:
• 0660T Implantation of anterior segment intraocular nonbiodegradable drug-eluting system, internal approach
• 0661T Removal and reimplantation of anterior segment intraocular nonbiodegradable drug-eluting implant
The above two codes have parenthetical notes to bill the medication separately.
• 0687T Treatment of amblyopia using an online digital program; device supply, educational set-up, and initial session
• 0688T Assessment of patient performance and program data by physician or other qualified health care professional, with report, per calendar month
• 0704T Remote treatment of amblyopia using an eye tracking device; device supply with initial set-up and patient education on use of equipment
• 0705T surveillance center technical support including data transmission with analysis, with a minimum of 18 training hours, each 30 days
• 0706T interpretation and report by physician or other qualified health care professional, per calendar month
The above five codes have parenthetical notes not to bill them with CPT 92065 and a few other codes.
• 0699T Injection, posterior chamber of the eye, medication
This last code goes with Dexycu, which already has an existing code valid for use (J1095).
Q: I heard that there were changes to the expiration dates on a couple of drugs with pass-through status. Can you tell me the details?
There are two eye-related codes that would have had their “Pass-through payment” status expire well before 2022 was over, but CMS noted it will extend this special privilege through 12/31/2022 in order to get another full years’ data on pricing for each. Those two codes are shown below; they go with Dexycu and Dextenza, respectively:
• J1095 Injection, dexamethasone 9 percent, intraocular, 1 microgram
• J1096 Dexamethasone, lacrimal ophthalmic insert, 0.1 mg
I’ll also comment on Omidria (J1097) here—which had its “pass-through” status expire way back in 2020 but still has its payment in 2022. As in 2021, this drug has coverage under the “Non-Opioid Pain Management Drugs and Biologicals that Function as Surgical Supplies” program.
Q: What about physician reimbursement under Medicare for 2022?
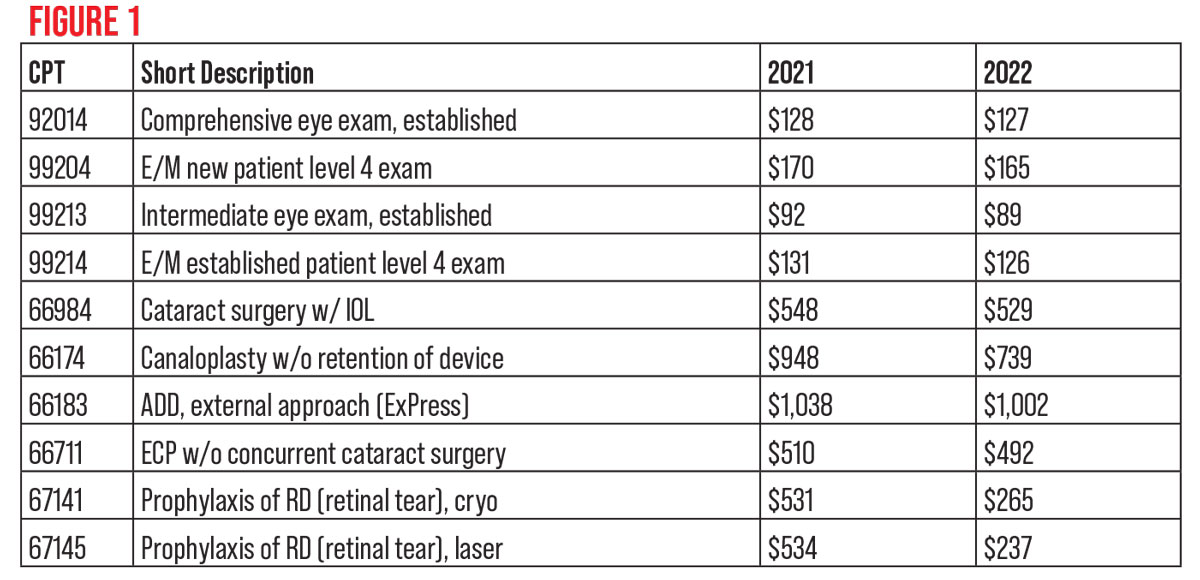
As the famous saying goes: “Aye, there’s the rub.” What you see in Figure 1 could change soon if Congress makes new legislation, because it’s not within CMS’ power to make the changes desired. As mentioned in the introduction to this month’s article, the payments listed in Figure 1 might have been changed by the time you read this. So, as of this writing, those are some 2021 vs. 2022 physician payments (payment shown is for “surgeon in facility,” not the office setting). Payments shown in the figure are rounded to the nearest whole dollar.
The large 67141 and 67145 payment decreases are largely because the global periods for this pair are now 10 days instead of 90. Exams for this treatment at the two-week interval would now be billable since there would be no global postoperative period in play then.
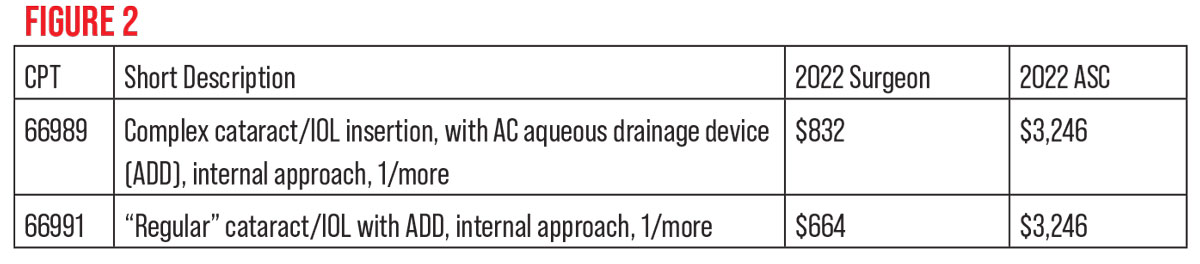
As of this writing, the 2022 payments for the new combination codes at the beginning of the article for surgeon in facility and ASC appear in Figure 2.
 |
| Click image to enlarge. |
The “Most Favored Nation” drug model for Part B drugs used in the office, that got a lot of publicity because of its onerous reimbursement provisions last year, got a stay in the Federal Courts early in 2021, and then CMS later placed it on hold. There’s no mention of it in the Final Rules for the 2022 Fee Schedules at all. Despite this, there’s a strong move afoot to allow Medicare to negotiate drug prices. We’ll see what the details are if it passes.
CMS changed the reimbursement status of remote imaging code 92229. It was changed from “contractor-pricing” in 2021. The main issue was that there were widely disparate payments as each MAC made its own decision. The payment now has a national rate of $45.36; as with most codes, payments vary slightly based on cost-of-living differences. The code 92229 is for “Imaging of retina for detection or monitoring of disease; point-of-care automated analysis and report, unilateral or bilateral.”
Q: For facilities, what are the biggest Medicare changes in 2021?
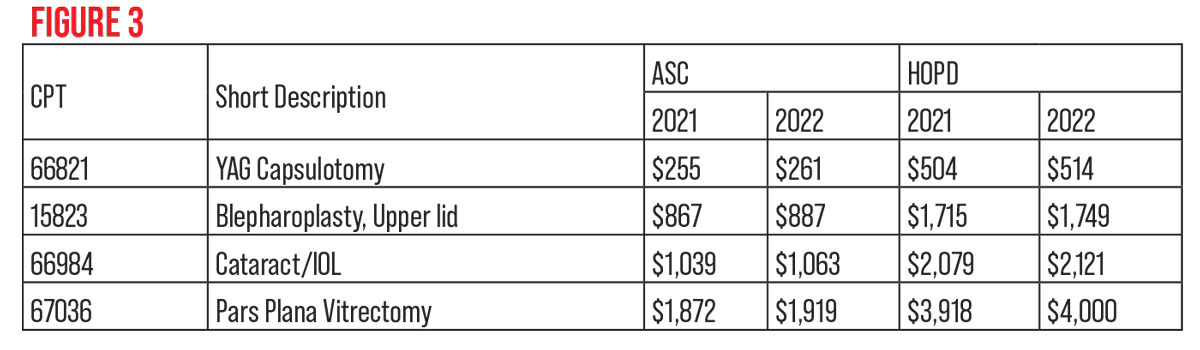
In 2021, Medicare increased the ASC conversion factor by 2 percent, and CMS increased reimbursement for hospital outpatient departments by the same amount. The prior authorization process CMS began last year for blepharoplasty, some ptosis codes and Botox injections and drugs continues for HOPDs; ASCs aren’t affected. Some 2021 vs. 2022 ASC and HOPD payments appear in Figure 3.
 |
| Click image to enlarge. |
Q: What about changes to Medicare beneficiaries’ obligations and other administrative changes for my office?
The 2022 Medicare Part B deductible rose to $233 (from $203 in 2021), so you’ll need to collect for this greater amount beginning in January. The revised ABN we wrote about in the September 2020 installment of Medicare Q & A may be used now but it becomes mandatory after the expiration of the Public Health Emergency declaration.
The monthly premium beneficiaries pay for Medicare Part B rose significantly, from $148.50 to $170.10 per month in 2022; we don’t typically discuss it here since it is paid by our patients, but in a public comment CMS stated why, and it succinctly illustrates the problems CMS has with continually rising drug prices. CMS noted three main reasons:
- rising prices and utilization;
- Congress lowered the amount of the planned increase in Part B premiums for 2021 (and CMS is obligated to make adjustments to keep the program solvent); and
- additional contingency reserves due to uncertainty over CMS paying for Aduhelm, the controversial and very expensive Alzheimer’s drug.
Q: Can you summarize the changes in the Quality Payment Program or MIPS for 2022?
Yes, and, though they’re important, they’re mostly related to the scores you need to get. The Quality Payment Program enters year six in 2022, and there are only modest revisions to the Merit-based Incentive Payment System that most providers use. The maximum negative payment adjustment will remain at 9 percent for the Medicare payments you get in 2024 (from reporting in 2022), though the minimum composite score to avoid a penalty increases a lot—all the way to 75 points from the 60 points needed in 2021. This change may make it far more difficult for providers to earn a bonus. On the penalty side, as in 2021, if CMS allows another MIPS Hardship Exception for COVID-19, there won’t be many penalized and, since the MIPS program is budget neutral, fewer penalties means those who do well won’t get as much as they might otherwise.
Exceptional Performance bonuses remain excluded from this budget-neutral calculation—but providers must achieve 89 points to get it—and 2022 is the last year for this special bonus.
In 2022, the weighting of Quality and Cost change to 30 percent for Quality and 30 percent for Cost. The weights of Improvement Activities and Program Interoperability remain unchanged. Last year, CMS put the new MIPS Value Pathways system on hold, but now it’s slated to go active in 2026. Few details are available so far, and CMS notes that more information will accompany future rulemaking.
Mr. Larson is a senior consultant at the Corcoran Consulting Group and is based in Tucson, Arizona. He can be reached at plarson@corcoranccg.com.



