Two recent presbyopia-correcting intraocular lens technologies, trifocals and extended-depth-of-focus lenses, aim at increasing the range of vision without compromising vision quality. In particular, both trifocals and EDOFs offer good quality vision at the intermediate range.
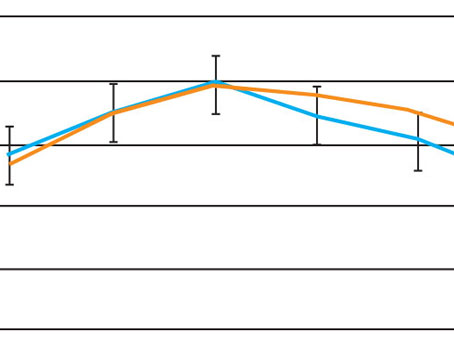
“Intermediate vision is a really valuable working distance for a lot of patients,” says Dagny Zhu, MD, FAAO, managing partner at Hyperspeed LASIK in Rowland Heights, California, and volunteer attending and lecturer at Los Angeles County+University of Southern California department of ophthalmology. “I’ve put in a lot of [bifocal] multifocals, and I’ve found that patients really appreciate the near vision, but some will notice that they struggle with anything around the intermediate range. If you look at the defocus curve for [bifocal] multifocals, it really drops off for anything between near and far,” she says. Some activities that benefit from good intermediate vision include computer work, looking at a GPS while driving, checking price tags and cooking. The challenge of producing good intermediate vision, however, lies in the fact that extending range of vision usually decreases overall image quality.
In this article we’ll take a look at some aspects of trifocals and EDOFs—how their lens materials contribute to visual performance and potential dysphotopsias, and how thorough patient counseling can improve overall satisfaction.
Trifocals and EDOFs
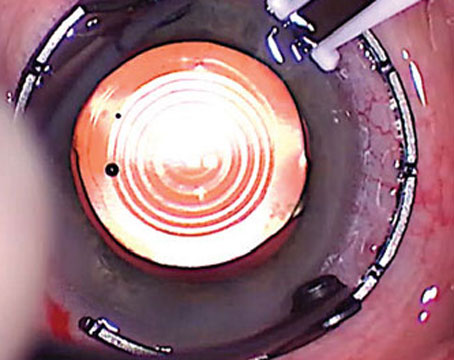
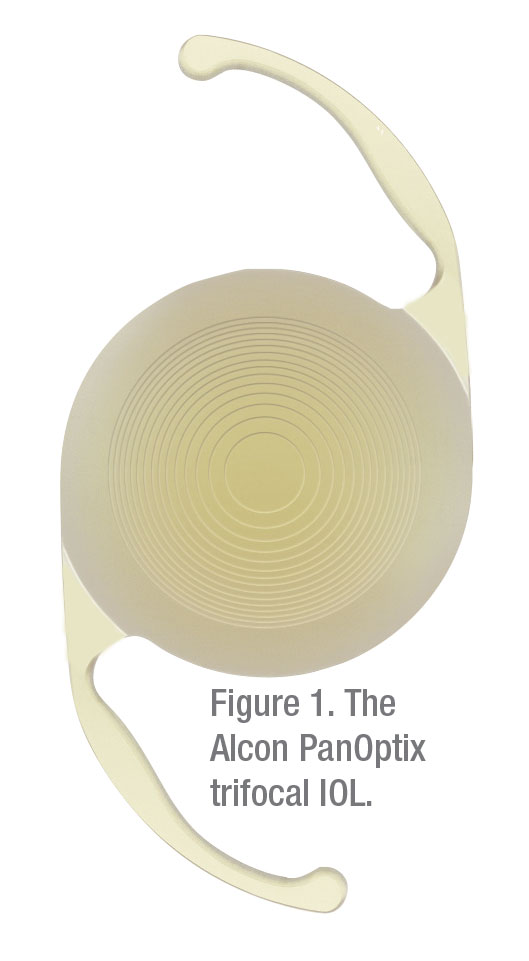
Alcon’s PanOptix trifocal, which gained FDA approval in August, is the only trifocal option currently available in the United States. Unlike bifocal multifocal IOLs, which split light in two ways to give near and distance vision, trifocals split light three ways to provide an intermediate focal point, typically around 80 cm (about 31 inches). The PanOptix trifocal’s intermediate point, however, is around 60 cm (24 inches). “Trifocals aren’t quite continuous [in terms of focus], but they’re better than [bifocal] multifocal IOLs and bifocal glasses,” says Daniel Chang, MD, of Empire Eye and Laser in Bakersfield, California, and member of the ASCRS Refractive Surgery Clinical Committee.
 |
Trifocals were found to provide better intermediate vision than multifocals with two focal points, according to a meta-analysis literature study conducted in 2017 that compared the two lens types’ clinical performance.1 In a similar study in 2018, researchers in South Korea found that trifocals outperformed bifocal multifocals in intermediate vision and provided similar or better distance and near vision without compromising visual quality.2
Dr. Zhu performed about 60 cases with trifocals in the two months following PanOptix’s approval by the FDA. She says her preliminary results have been fairly favorable, with many patients seeing 20/20 at distance, intermediate and near at one week postoperatively. “That’s just not been my experience with [bifocal] multifocals, which again do not give the same level of intermediate vision as trifocals,” she says. “It’s been quite excellent.”
Prior to the trifocal, the EDOF lens was the latest iteration of presbyopia-correcting lens technology. “In the U.S., the only true EDOF lens that we have is the Tecnis Symfony,” Dr. Zhu notes. “Unlike multifocals, which split light for specific focal distances, the EDOF extends the range of focus, so there’s no splitting of light at a discrete distance. In that sense, it gives the patient a more continuous range of vision without dropping out in between specific focal points.” However, while the Symfony provides good distance and intermediate vision, it doesn’t provide the same quality of near vision as a multifocal or a trifocal IOL, according to Dr. Zhu.
The bulk of the literature on trifocals has been published outside the United States, where the trifocal has been in use longer. “A couple of studies say different things, so I don’t think we can necessarily conclude anything in particular,” Dr. Zhu says. “The only thing that’s accepted is that the Symfony does not provide as much good near vision as the PanOptix trifocal. In terms of quality of distance vision and intermediate vision, I’ve seen studies saying it’s about the same among both. In terms of the degree of contrast sensitivity, I’ve seen some say it’s better, and some say it’s the same, so I don’t really think a conclusion can be drawn about that.
“The Symfony EDOF uses a completely different technology from multifocals,” Dr. Zhu continues. “[Bifocal] and trifocal multifocals tend to offer really good near vision at around 15 inches or 40 cm. I would say the Symfony is closer to 20 inches, so definitely not as much near vision.”
A 2019 prospective, consecutive, non-randomized study in New Delhi, India, compared the visual outcomes and clinical performance of diffractive trifocal and EDOF lenses over six months in 160 eyes of 80 patients who had bilateral cataract surgery with implantation of either a trifocal (FineVision, PhysIOL, not approved in the United States) (n=40) or an EDOF (Tecnis Symfony) (n=40).3 The study found that the trifocals performed better in near visual acuity, and that trifocals and EDOFs demonstrated comparable “excellent” distance and intermediate visual acuity and a high percentage of spectacle independence with minimal levels of disturbing photic phenomena.
 |
A 2018 study in France compared binocular and monocular uncorrected distance, intermediate and near visual acuity in patients randomized to receive trifocals—either FineVision or AcrySof IQ PanOptix—or the Tecnis Symfony EDOF. The researchers found that all three IOLs provided good distance visual acuity and reported that patients had few visual symptoms. They also found that the trifocal IOLs provided statistically better near vision than the EDOF IOL.4
“I’m sure down the road we’ll be able to offer extended depth of range up to a closer point,” says Dr. Zhu. “That would be ideal.”
Dr. Chang says he hasn’t implanted any trifocals yet; he currently uses the Symfony EDOF in his patients to offer intermediate vision. “EDOF lenses try to spread vision more evenly so that the overall quality of vision and night vision symptoms can be improved,” Dr. Chang explains. Expanding the depth of field and reducing night vision symptoms comes at the expense of some near vision, he notes.
A study conducted by university hospital researchers in Madrid and
Alicante, Spain, found that the Symfony EDOF lens showed statistically significantly better subjective and objective depth of field than the Mini Well (SIFI MedTech) EDOF, the FineVision (PhysIOL) and AT LISA Tri (Carl Zeiss Meditec) trifocals and the Tecnis ZMB and ZLB (Abbott Laboratories) bifocals.5
Torics
Dr. Chang says the toric versions of the Symfony EDOF and PanOptix trifocal are welcome additions to the surgeon’s armamentarium. “It’s good to be able to correct astigmatism with a lens instead of separate incisions on the cornea,” he adds.
Knowledge of astigmatic tolerance of IOLs is important for surgical planning and can help avoid the need for secondary management after implantation.6 It’s been estimated that multifocal IOLs in general can tolerate about 0.75 D of astigmatism,7 compared to EDOFs’ tolerance, which was found to be slightly better at 1 D in a study that compared relative indications and contraindications for implantation. The study also reported that trifocal users can tolerate about 0.5 D of astigmatism.8 “EDOF technology doesn’t give you as much range as a trifocal,” says Dr. Chang, “but the range it does give, at least in theory and in my experience, tends to be better. So even if you miss a little bit of astigmatism or the lens is positioned off by a little bit, it’ll tend to do a little better than a toric multifocal or a trifocal, in which nailing the alignment is really important.”
He points to another recent study that compared EDOFs to trifocals in terms of induced astigmatic defocus on visual performance.6 The study compared the reduction of mean monocular visual acuity at all defocus levels relative to no defocus and found it was significantly lower in the IC-8 (AcuFocus) EDOF group, compared to the FineVision, AT LISA and enVista (Bausch + Lomb), supporting other studies’ findings that EDOFs tend to provide a greater tolerance of induced astigmatic defocus.
 |
Chromatic Aberration
Contrast sensitivity improves when chromatic aberration is reduced. Dr. Chang explains that as light passes through a lens, it breaks into its component colors. Each wavelength focuses differently because the index of refraction of the lens affects each one differently. “With a good lens system, you can focus the image sharply,” he says. “But if you have too much separation of colors, you end up with a blurring effect—that’s chromatic aberration.”
The material of an IOL contributes to chromatic aberration. Both the Symfony and the PanOptix are built on proprietary hydrophobic acrylic platforms. Hydrophobic foldable acrylics are made of a series of copolymers of acrylate and methacrylate derived from PMMA to make them foldable and durable, and they have a refractive index between 1.44 and 1.55.9 Due to a high refractive index and low anterior curvature, hydrophobic acrylic tends to be associated with dysphotopsias more often than other acrylics, such as hydrophilic acrylic (typical refractive index: 1.43).9 However, materials with a high refractive index can be made much thinner, allowing, as in the case of the AcrySof material, the lens to have a full 6-mm refractive optic, even as the IOL power increases. In contrast, other materials may require a reduction of the effective refractive zone of the optic as the power increases in order to prevent variation in the lens’ central thickness.
The PanOptix lens material has an index of refraction of 1.55 and an abbe value of 37. The Tecnis lens material, a type of UV-blocking hydrophobic acrylic, has an index of refraction of 1.47 and an abbe number of 55.10
Dr. Chang says that chromatic aberration is often the culprit for unsatisfied patients. “We don’t see chromatic aberration at the slit lamp, and patients may not necessarily tell us, ‘I have a chromatic-aberration problem,’ ” he says. “But when there’s a dissatisfaction with image quality in spite of good Snellen acuity, you could be dealing with either a higher-order aberration, such as spherical aberration, or chromatic aberration. In my practice, I like to use a material that provides chromatic aberration correction to make it as little of an issue as possible. For any material, the higher the index of refraction, the higher the chromatic aberration.”
Dr. Chang says that patients may not notice chromatic aberration as much with monofocal lenses, but with diffractive lenses, image quality can become an issue.
Some image-quality issues and dysphotopsias are common to all multifocal lenses, including trifocals, notes Dr. Zhu. And even with EDOF lenses, patients still experience dysphotopsias such as glare, halo and starbursts.
 |
Dysphotopsias
While trifocals and EDOFs aim for reducing dysphotopsias, unwanted photic phenomena occur whenever the range of vision is extended. Dr. Chang says that these dysphotopsias are more evident in dim environments, particularly with night driving. “The amount of off-axis light is directly related to the amount of near vision that you get with a particular lens,” he says. “So if you look at the PanOptix versus the ReSTOR +3 D, I would expect more near and intermediate vision with PanOptix, and of course, a greater number of night-vision symptoms. If you look at the EDOF Symfony versus the Tecnis multifocal, I would expect fewer night-vision symptoms but not quite as much near vision.”
Dr. Zhu notes that the results from the PanOptix FDA trials showed that it had no more dysphotopsias than other trifocal or multifocal lenses. “Around the same level of decrease in contrast sensitivity was observed as well, which is common to all multifocal lens technology,” she says.
One of the common benefits cited in regard to EDOF lenses is that they have fewer dysphotopsias than multifocal IOLs. The [EDOF] AT LARA 829MP pre-clinical study report makes this claim, saying this EDOF’s diffractive optical design, called “light bridge,” corrects spherical and chromatic aberration and causes fewer visual disturbances than multifocal IOLs. For the Symfony, Johnson & Johnson reports a low incidence of visual symptoms.
A 2019 study in Heidelberg, Germany, evaluated the functional results and photic phenomena of the Mini Well Ready IOL (SIFI MedTech)—a single-piece hydrophilic acrylic EDOF with a hydrophobic surface that relies on spherical aberrations of opposite signs to create an elongated focus11—and found that it provided good distance and intermediate vision, improved reading-distance visual acuity and few to no dysphotopsias.
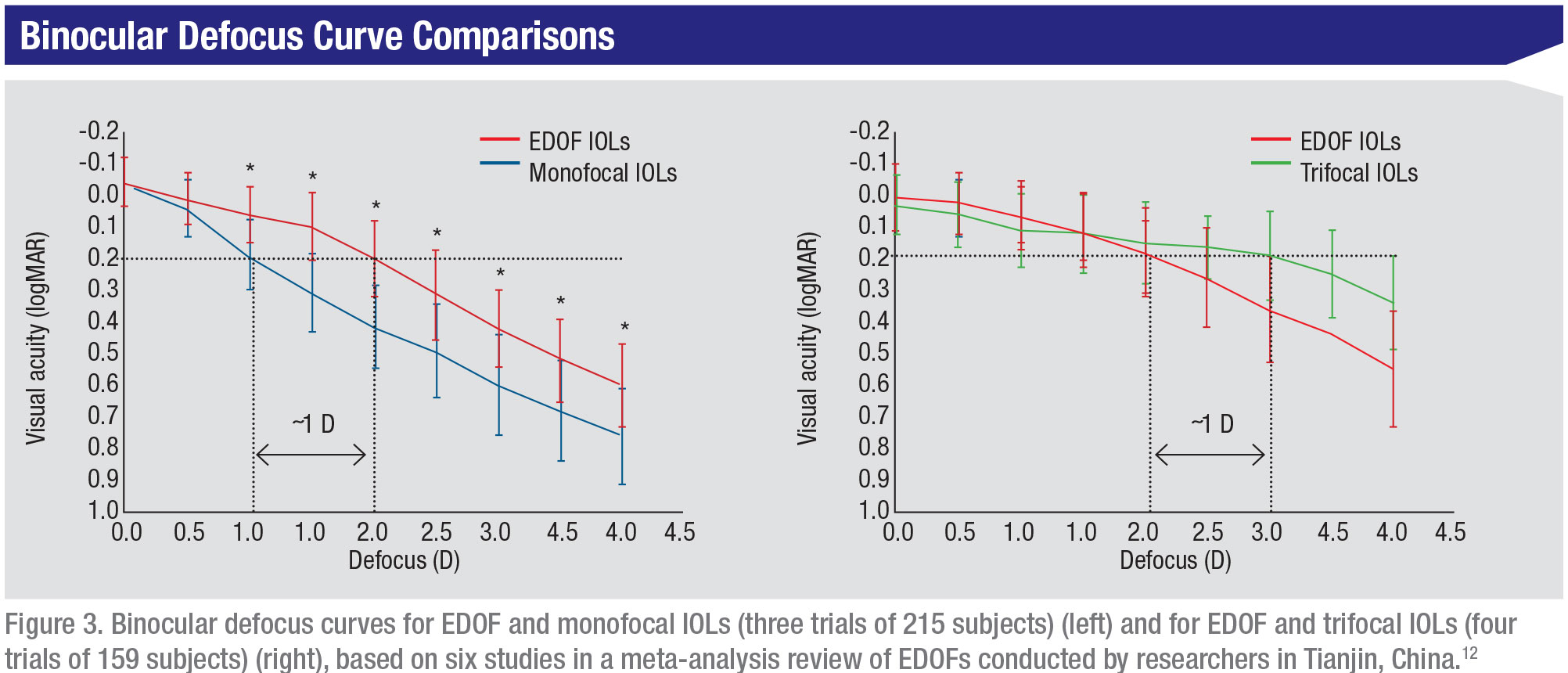
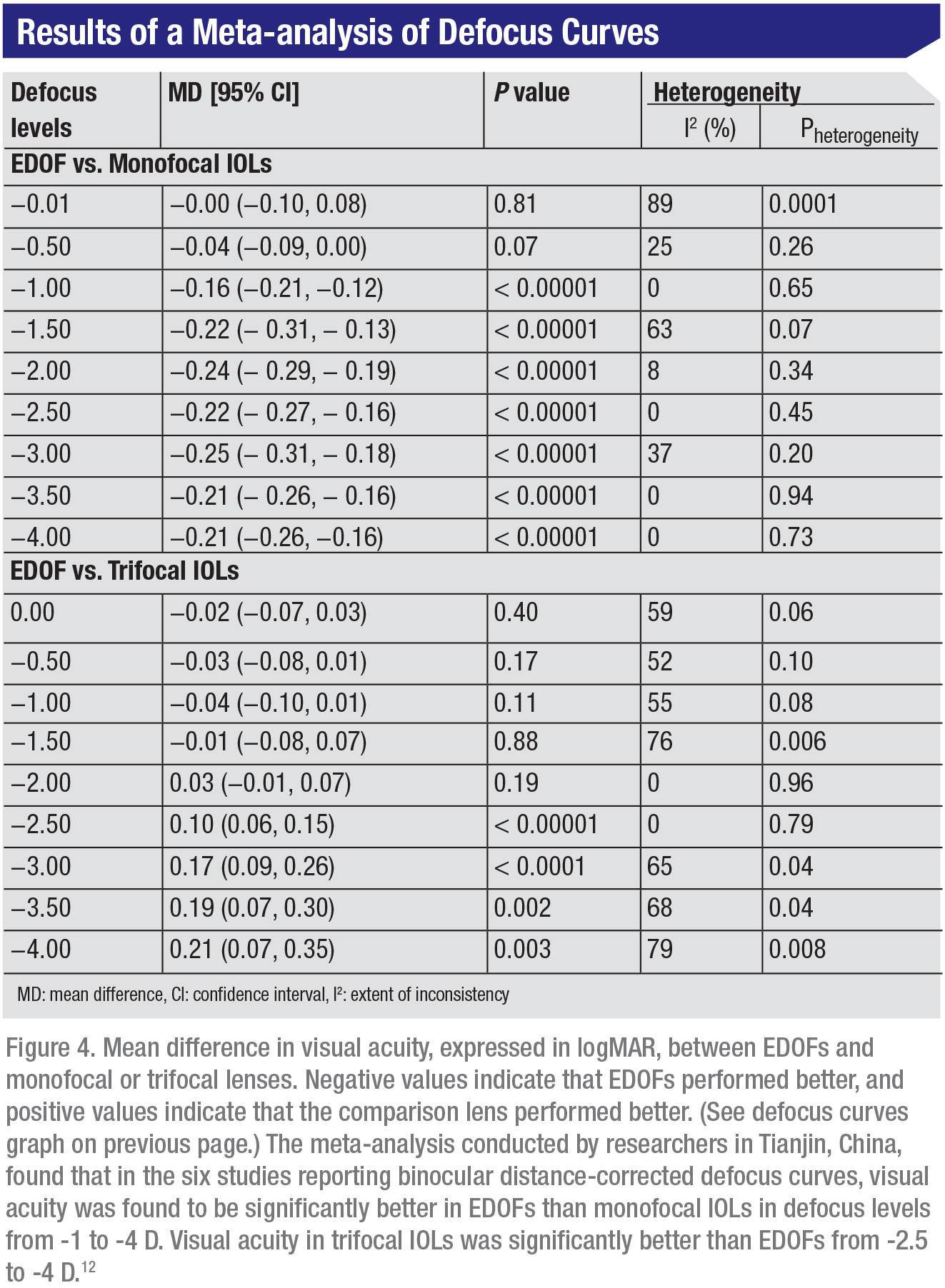
According to a meta-analysis of randomized and nonrandomized controlled studies by researchers in
Tianjin, China, compared to monofocals, EDOFs provided better intermediate and near visual acuity, but more contrast reduction and more frequent halos; compared to trifocals, EDOFs had better contrast sensitivity and comparable halo incidence.12 The researchers say they used only the Tecnis Symfony EDOF, due to a lack of studies on other EDOF lenses.
Patient Counseling
At the end of the day, all these lenses have some visual side effects, particularly at night. However, Dr. Chang says those side effects shouldn’t discourage qualified patients from seeking presbyopia-correcting IOLs. EDOF and trifocal IOLs may be safer alternatives to bifocal spectacles, which have been associated with a 2.3-fold increased risk of tripping and falling in the elderly because they throw off depth perception. Traumatic falls are the number one cause of injury and death among elderly Americans.13
“Right now the most important thing for surgeons to keep in mind is the kind of night-vision symptoms each lens produces so they can describe them appropriately to patients,” says Dr. Chang. He elaborates, saying that the Symfony produces different night-vision symptoms than other lenses. He explains that with traditional multifocals, there’s glare, which is blurring of light around a light source, and halo, which manifests as a ring around the light source due to the IOL’s single add power. On the other hand, in addition to some glare, the Symfony primarily produces multiple fine halos—depending on the color of the light—and also starbursts, which are streaks of light emanating from the light source. “It’s commonly been described as a spider web, Ferris wheel, daisy or digital pattern. Spider web is the most common term I use,” Dr. Chang says.
Dr. Chang adds that counseling patients and illustrating and explaining specific symptoms—whether it’s halos, glare, single or multiple halos or spider-web patterns—helps patients tolerate them better. “It can be disorienting for patients if they’re not prepared for it,” he says. “If we simply say glare and halos, patients may not necessarily know what we mean. They’ll say, ‘No, it’s not glare. There are big lines coming out.’ In my experience, when limitations are expected, patients tolerate them pretty well.”
Contraindications
“In general, the same exclusion criteria can be applied to both types of lenses,” says Dr. Zhu. She says that patients with any ophthalmic pathology, either in the macula, the optic nerve or the cornea, probably shouldn’t receive EDOFs or multifocals. “For all of these lenses there’s some decrease in contrast sensitivity,” she says. “You don’t want to use them in a patient who already has vision problems.” She says this is due to the fact that these lenses were designed to work in perfect eyes. “If the eye is malfunctioning in one way or another, patients probably won’t get the full value of the lens,” she adds. “When I advise patients and tell them they’re not candidates for EDOFs, [bifocal] multifocals or trifocals because of their pathology, I usually recommend using a monofocal lens and reading glasses for anything close up.
“Another strategy is to leave patients with a little monovision—a little myopia in their nondominant eye,” Dr. Zhu continues. “Those patients are typically still able to do a lot of things close up. They may still need reading glasses for very fine print, but most patients are okay with that; they understand that that’s the best option available, given their situation.”
There are also some patients whose pathology prevents their receiving traditional multifocals but for whom an EDOF might be the answer. Dr. Chang says that the chromatic aberration correction in the Symfony lens makes it a possible alternative to multifocals in some cases because the patient’s visual quality won’t be degraded to the same degree as it would be with a traditional multifocal.
A Personalized Approach
Intraocular lens selection is not a one-size-fits-all procedure, experts say. Focal points and ranges are just two dimensions of a lens that bear consideration in the process of lens selection. “We as surgeons need to learn about and understand all the lens options we have so we can use them in a customized fashion for our patients,” Dr. Chang says. “Instead of saying, ‘This is what I do,’ we need to have an approach for each patient based on who they are and what they do. The first eye may receive something a little different than the second eye, for example.”
In Dr. Zhu’s clinical practice, she talks to patients to get a sense of the visual distances that are important to them. “You really have to talk to the patients about what their day-to-day life is like,” Dr. Zhu says. “What do they do for a living? What do they value in terms of type of work and activities they do? There are some patients for whom I’ll favor implanting a trifocal lens over a [bifocal] multifocal lens—those who can’t sacrifice their intermediate vision, like chefs who need to cook at arm’s length or people who are on the computer quite a bit. At the same time, an EDOF would probably do very well in these same patients, but, if the patient also requires a lot of good near vision—because they like to read a lot, for example—then probably the trifocal would be better than the EDOF because you won’t sacrifice as much near vision.”
“There’s Snellen acuity and there’s patient happiness, and patient happiness may not necessarily reflect in your Snellen acuity data,” Dr. Chang says. “We all know of products out there that have been taken off the market or lost popularity—not because of poor objective outcomes, but because patients just aren’t quite happy with their quality of vision. It’s hard to capture that, even with contrast data. Sometimes a patient with 20/25 vision is happy and one with 20/20 is not so happy.”
Are Two Lenses Better than One?
Dr. Chang says that trifocal and EDOF lens technologies have been shown to have varying performance in different areas. “There have been some head-to-head studies comparing EDOFs to trifocals, and so far each tends to have comparable performance in certain areas and better performance in others,” Dr. Chang says.
He says some studies have examined combining lens technologies, such as implanting an EDOF in one eye and a multifocal in the other eye to get the strengths of both lenses. Other options may include implanting an EDOF and a toric lens for added depth of focus.14
Some enterprising companies are even combining the two technologies in one lens. For instance, a few years ago, a trifocal lens with EDOF features, the Acriva Reviol Tri-ED (VSY Biotechnology), was developed in the Netherlands. One study found that it provided good distance, intermediate and near vision.15 The study authors said that based on the clinical outcomes, they believe EDOF elements can be incorporated into a multifocal visual system. Long-term studies will have to be done to bear this out.
Ultimately, all intraocular lenses have benefits and drawbacks, says Dr. Chang. “It’s a matter for the surgeon to figure out what will work best for which patients.” REVIEW
Dr. Zhu reports no financial disclosures. Dr. Chang is a consultant and investigator for Johnson & Johnson. He’s also a clinical researcher for AcuFocus’ IC-8 lens.
1. Xu Z, Cao D, Chen X et al. Comparison of clinical performance between trifocal and bifocal intraocular lenses: A meta-analysis. PLoS One 2017 Oct 26;12:10:e0186522. PMID 29073156.
2. Yoon CH, Shin IS, Kim MK. Trifocal versus bifocal diffractive intraocular lens implantation after cataract surgery or refractive lens exchange: A meta-analysis. J Korean Med Sci 2018 Sept 27;33:44:e275. PMID 30369857.
3. Singh B, Sharma S, Dadia S, Bharti N et al. Comparative evaluation of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and an extended depth of focus intraocular lens. Eye Contact Lens 2019 July 5. [Epub ahead of print.] PMID: 31283552.
4. Cochener B, Boutillier G, Lamard M and Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg 2018;34:8:507-14.
5. Palomino-Bautista C, Sánchez-Jean R, Carmona-González D, et al. Subjective and objective depth of field measures in pseudophakic eyes: Comparison between extended depth of focus, trifocal and bifocal intraocular lenses. Int Ophthalmol 2019 Oct 3. Epub ahead of print. PMID: 31583551.
6. Ang RE. Comparison of tolerance to induced astigmatism in pseudophakic eyes implanted with small aperture, trifocal, or monofocal intraocular lenses. Clin Ophthalmol 2019;13:905-911. [Epub ahead of print.] PMID 31213762.
7. Braga-Mele R, Chang D, Dewey S et al [ASCRS Cataract Clinical Committee]. Multifocal intraocular lenses: Relative indications and contraindications for implantation. J Cataract Refract Surg 2014; 40;2:313-22.
8. Carones F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal and extended range of vision intraocular lenses (IOLs). Open J Ophthalmol 2017;7:1.
9. Bellucci R. An introduction to intraocular lenses: Material, optics, haptics, design and aberration. Cataract: ESASO Course Series. Basel, Karger 2013:3:38-55.
10. Abbe number and longitudinal chromatic aberration (LCA). Bausch Surgical. Accessed Nov 4 2019. https://bauschsurgical.eu/blog-learning/blog/abbe-number-and-longitudinal-chromatic-aberration-lca/
11. Giers B, Khoramnia R, Caradi D, Wallek H et al. Functional results and photic phenomena with new extended-depth-of-focus intraocular lens. BMC Ophthalmol 2019;19:197.
12. Liu J, Dong Y, Wang Y. Efficacy and safety of extended depth of focus intraocular lenses in cataract surgery: A systematic review and meta-analysis. BMC Ophtahlmol 2019;19;198.
13. Falls prevention facts. National Council on Aging. https://www.ncoa.org/new/resources-for-reporters/get-the-facts/falls-prevention-facts. Accessed 8 Nov 2019.
14. Calogero D. New categories of IOLs for improved near and intermediate performance. FDA/AAO Workshop: Developing novel endpoints for premium intraocular lenses. March 28 2014. https://www.fda.gov/media/88004/download.
15. Acar BT, Duman E, Simsek S. Clinical outcomes of a new diffractive trifocal intraocular lens with enhanced depth of focus (EDOF). BMC Ophthalmol 2016;16:208. PMID: 27899084.