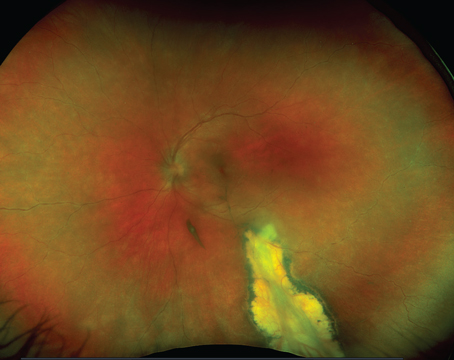
Retina specialists have been treating neovascular age-related macular degeneration with anti-vascular endothelial growth factor therapies for years. Though it’s been remarkably successful for many patients, there are still those few who don’t respond to their initial anti-VEGF treatment and need something more. Here, retina specialists discuss how they handle recalcitrant wet AMD.
Starting Treatment
The goal of managing any case of neovascular AMD is to preserve macular function, in particular, at the foveal center. “Typically, that means trying to control the exudation,” says New York’s K. Bailey Freund, MD. “If we’re not having success after a typical monthly loading phase, most retinal specialists, including myself, might try switching agents.”
 |
| Agents that act on different forms of VEGF, come in higher doses or use sustained-delivery may help in tough AMD cases. |
Carl Regillo, MD, in practice at Wills Eye Hospital in Philadelphia, says that he starts treatment with one of the first-generation anti-VEGFs, which include bevacizumab, ranibizumab or aflibercept. “We now have more treatment choices than ever before, but the reality is that most insurance companies mandate bevacizumab first,” he says. “It’s not by choice, but we usually end up starting with that. If I’m not getting an adequate response, meaning the macula is not completely, or nearly completely, drying within the first three treatments, I’ll then switch to on-label ranibizumab or aflibercept and treat a few more times. If the macula is optimally responding, then I’ll stick with one of those two drugs. If there’s persistent, significant exudation or the patient needs a very frequent treatment regimen to have optimal disease control, I’ll think about switching to faricimab next.”
He adds that faricimab (Vabysmo, Genentech) has better durability than the first-generation drugs, and it may also achieve better drying in select patients. He is not using much brolucizumab at this time because of the ocular safety issues. “Before faricimab was FDA-approved, I did opt for brolucizumab as the next step in suboptimal responders, but the safety profile’s not as good as other anti-VEGFs,” Dr. Regillo says.
Dr. Freund agrees. “I haven’t been using brolucizumab since the safety issue of occlusive vasculitis emerged; however, during the brief period I used the drug, it seemed that eyes that couldn’t be controlled with the other agents responded more robustly to brolucizumab,” he says. “The safety issue was very unfortunate, and, in my opinion, this risk usually outweighs the drug’s potential benefit, even in patients who aren’t optimally controlled.”
Physicians will sometimes consider switching from bevacizumab or ranibizumab to aflibercept in tough cases. In one retrospective study, researchers included 282 and 359 eyes “non-switch” (i.e., staying on ranibizumab) and “switch” (switched to aflibercept) cohorts, respectively. The researchers say the cohorts were well-balanced. Though visual acuity remained stable during the observation period in both cohorts of eyes, the researchers say that optical coherence tomography images demonstrated lower prevalence of intraretinal and subretinal fluid as well as pigment epithelial detachment at 12 months in eyes subjected to switch of anti-VEGF agent compared to the non-switch eyes.1
In another study, researchers analyzed 164 eyes (101 were switched from bevacizumab to aflibercept (group 1) and 63 from ranibizumab to aflibercept (group 2). One year after the switch, there was an overall nonsignificant mean decrease of two ETDRS letters in BCVA. Three years after switching, there was an overall mean decrease of seven ETDRS letters, which was statistically significant. However, they noted a significant improvement in the mean central retinal thickness was found at one, two and three years. They say that aflibercept can be useful in the management of refractory neovascular AMD, with a good morphological response. However, in the long-term, it didn’t achieve BCVA stabilization.2
Vabysmo
Looking at relatively newer arrivals on the AMD scene, according to Karl Csaky, MD, PhD, in practice in Dallas, many retina specialists who treat tougher cases of AMD are now considering Vabysmo [faricimab-svoa, Genentech], with some saying they might even use it for initial therapy.
“There hasn’t been anything new for wet AMD since aflibercept was approved over a decade ago, until the recent introduction of Vabysmo,” Dr. Csaky says. “Many of us are considering Vabysmo now that there are more real-world data to suggest that it’s safe and that we’re not seeing anything that’s of concern. Some of my colleagues are even starting to consider Vabysmo as an initial therapy, and I think that’s completely reasonable given the clinical data. In many cases, Vabysmo may be a very good alternative to other therapies. We’re in a transition zone to fully appreciate what the full impact of Vabysmo will be on real-world utilization.”
Vabysmo is the first FDA-approved treatment designed to block both VEGF-A and Ang-2 in wet AMD. It’s been shown to improve and maintain vision with treatments from one to four months apart in the first year following four initial monthly doses. Based on positive results across four Phase III studies in wet AMD and DME, it was approved by the FDA in January 2022. The studies consistently showed that patients treated with Vabysmo given at intervals of up to four months achieved non-inferior vision gains compared to aflibercept (Eylea, Regeneron) given every two months in the first year. It was well-tolerated in all four studies, with a favorable benefit-to-risk profile. The most common adverse reaction was conjunctival hemorrhage, which was reported in 7 percent of patients.3
According to Dr. Csaky, Vabysmo is following the aflibercept model. “If we look at what happened 10 years ago when Eylea came out, we went right into using Eylea for the refractory cases and trying to understand its full impact,” he says. “We were beginning to feel comfortable that the safety profile was good, and then it was just a question of determining the full potential of the drug. We had refractory cases of patients on Lucentis who then did very well on Eylea.”
The real question with any new AMD drug is its durability. “Vabysmo was approved just over a year ago, and some practices are just starting to feel comfortable enough to use it,” Dr. Csaky explains. “I don’t think we have the full stamp of approval yet, but it’s now clearly a nice alternative to consider once you’ve gone through the typical switching and looking to try to treat and extend. There are still questions about whether it needs to be loaded, or whether we can treat and extend right away.”
Dr. Freund adds that faricimab appears to be a bit more robust in its ability to dry and possibly extend the duration between injections than the other agents, excluding brolucizumab. “I was cautious in starting to use faricimab after I saw a patient develop occlusive vasculitis with brolucizumab,” he says. “My impression of faricimab is that I’m not seeing as big of a benefit as I saw with brolucizumab compared to the other anti-VEGFs. But, it does seem to help control exudation better than the other agents in some of these refractory cases. Although I might be able to reduce or resolve fluid in some of those incomplete responders, I haven’t been able to extend the injection interval more than a week or two. I think we have to manage expectations because, in the clinical trials, there were patients who could go to these very long treatment intervals of 12 to 16 weeks. If an eye already can’t be controlled or extended with the current agents beyond a month, it’s unrealistic to think that switching to faricimab will be able to both get rid of the exudation and also extend to a very long interval. Patients who can be extended are more likely going to be treatment-naive cases, which tend to respond more robustly after the first injection.”
PCV Patients
Polypoidal choroidal vasculopathy is often considered more refractory to anti-VEGF therapy than other neovascular AMD cases, according to Dr. Freund. “That may be because there are dilated vascular elements within the neovascular lesion,” he says. “Also, these eyes often have choroidal features that overlap with CSR and indicate choroidal venous congestion that may drive fluid into the subretinal and intraretinal spaces. So, in those cases, it might be desirable to initiate treatment with one of the more potent agents, such as aflibercept or faricimab.”
He adds that high-dose aflibercept, currently under FDA review, might be an effective alternative to use in eyes that might benefit from a more aggressive therapy to get them under control. “Rarely, I also will use photodynamic therapy in PCV cases,” he says. “But, unlike some colleagues, I feel that using combination therapy at the initiation of therapy isn’t an effective long-term strategy for PCV. PCV patients typically present 10 years younger than our typical age-related macular degeneration patients of Western European ancestry. While combination therapy may seem effective for several years, recurrences occur because the treatment targets just the polypoidal lesions and not the larger neovascular complex referred to as a ‘branching vascular network.’ New polyps typically occur, and visual outcomes for eyes receiving multiple PDT treatments are often poor. I’ve learned through experience that this reactive strategy often fails due to these unpredictable recurrences.”
Dr. Regillo also occasionally uses verteporfin photodynamic therapy in these patients with PCV. “It’s the only photosensitizing drug that’s FDA-approved for photodynamic therapy,” he notes. “The chances of me needing photodynamic therapy is really rare. In fact, less than 1 percent of neovascular AMD ever gets photodynamic therapy nowadays.”
Other Treatments
Dr. Freund says that he will occasionally use off-label strategies, such as treating more than monthly if a patient is really not being controlled. “If a patient continues to have hemorrhage or is losing vision, I might give an additional injection between monthly injections,” he says. “In those situations, I often use a sample. In some patients, you just need to treat more aggressively at the initiation of therapy.”
He also occasionally uses aqueous suppressants to extend the duration of anti-VEGF injections. “Glaucoma agents reduce the production of aqueous and may slow the clearance of drugs, which may extend the duration just a little bit,” Dr. Freund explains. “In some patients, we may not be making progress because the drug may only last for say three-and-a-half weeks, and we’re only injecting monthly. By the time we give the next injection, we’re back to where we started, not building on the success of the first injection. But, if you could extend that just a few extra days, then you could potentially continue to dry the macula. In some of my patients, just adding a topical timolol-brinzolamide combination seems to help get them under control. I might try this strategy if there’s no contraindication to using those drugs, but to prove whether that’s an effective strategy would require a formal randomized trial with placebo.”
The Future
Physicians say there are therapies on the horizon, such as gene therapy and high-dose aflibercept, that hold out the hope for more effective treatments for recalcitrant cases.
Dr. Freund notes that gene therapy looks promising if the safety issues related to intraocular inflammation can be overcome. Dr. Regillo adds that other agents in the pipeline hold promise, as well. “There’s a high likelihood that high-dose aflibercept will be FDA-approved and in our hands within the next year or so,” he says. “It met its primary endpoint in the Phase III neovascular AMD study, so it’s pending FDA approval. That drug looks more durable than the older drugs we’ve been using. There is also still the possibility that KSI-301 could get FDA-approved for wet AMD.”
Other agents currently in the pipeline include OPT-302, which is a fusion protein that binds VEGF-C/D. “It’s in Phase III clinical trials, and is being used as a combination therapy with a VEGF-A blocker (ranibizumab or aflibercept),” Dr. Regillo explains. “It’s being used in combination in hopes of getting improved visual acuity outcomes. It’ll probably be another couple of years before we know the study results. Then, there are a whole host of therapeutics in the pipeline, mostly aiming at greater anti-VEGF durability, many of which are sustained release of an anti-VEGF-A or an anti-VEGF-like agent. And that includes the port-delivery system [Susvimo, Genentech], which was FDA-approved over a year ago, but implementation of the device is on hold because of an issue with the septum of the device that has to be rectified. But patients would undoubtedly benefit from highly effective sustained delivery and choose it.”
Also being examined is a class of therapeutics called tyrosine kinase inhibitors. “These are small molecules that have to be packaged in polymer-like sustained delivery platforms, injected intravitreally, or in a suspension injected suprachoroidally aiming to get an anti-VEGF-like effect for four, six or eight or so months,” he adds. “Those are all in the sustained-delivery category. It’ll provide an effect like we get now, but for more than just three or four months, which is about the limit to the drugs that we’re using. Lastly, there are several more gene therapy approaches being tested aiming for very long-lasting, potentially even indefinite, anti-VEGF therapy.”
Dr. Csaky is a consultant/advisor to Abbvie, Adverum Biotechnologies, Merck & Co, Inc, Ocular Therapeutix, Regeneron, and Ribomic. He is a consultant/advisor to and receives grant support from Genentech/Roche and Novartis Pharma AG. He is a consultant/advisor and receives equity from EyeBio. Dr. Regillo is a consultant to 4DMT, Adverum, Aldeyra, Allergan, Annexon, Apellis, Aviceda, Genentech, Iveric, Kodiak, Merck, NGM Biopharmaceuticals, Notal Vision, Novartis, Ocugen, Opthea, Ray, Regenxbio, Regeneron, Stealth Biotherapeutics, Takeda, Thea and Zeiss. Dr. Freund is a consultant to Bayer, Genentech, Novartis and Regeneron.
1. Granstam E, Aurell S, Sjovall K, Paul A. Switching anti-VEGF agent for wet AMD: Evaluation of impact on visual acuity, treatment frequency and retinal morphology in a real-world clinical setting. Graefe’s Archive for Clinical and Experimental Ophthalmology 2021;259:2085–2093.
2. Neves Cardoso P, Pinheiro AF, Meira J, et al. Switch to aflibercept in the treatment of neovascular AMD: Long-Term Results. J Ophthalmol 2017:6835782.
3. Genentech news. https://www.gene.com/media/press-releases/14943/2022-01-28/fda-approves-genentechs-vabysmo-the-firs. Accessed February 18, 2023.