 |
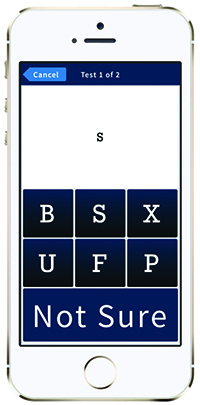
| Figure 2. The most popular test within Paxos Checkup is the visual acuity test. Pictured here, it is simple and intuitive, even for patients who are illiterate or have limited English proficiency. Patients need only match the letter in the white box to one of the letters below or select “Not Sure.” |
And it’s beginning to revolutionize health care. In 2015, approximately 5 million people were already using connected mobile health (mHealth) devices to help their doctors monitor their cardiac rhythms, blood glucose or other metrics, and that is expected to rise to 15 million by 2018 and to 36 million by 2020.1
Much of that growth will likely come from smartphone-enabled home medical monitoring. With widespread access to cellular networks and high-speed image and data processing capabilities, today’s smartphones are orders of magnitude faster than many of the medical diagnostic devices used in the 1990s. And cell phone use is becoming nearly ubiquitous, even among older adults. Americans now spend an average of 5.6 hours daily using some form of digital media, more than half of it on a smartphone or tablet (See Figure 1).2
“At the same time as this boom in smartphone usage, we were facing huge changes in vitreoretinal care, with more patients requiring frequent injections for the treatment of macular degeneration and other diseases,” says Mark S. Blumenkranz, MD, a retinal specialist, professor and former chair of ophthalmology at the Byers Eye Institute at Stanford University School of Medicine. “I was looking at my iPhone one day and thought how great it would be if there was a phone-based eye test so I could track how my patients were doing between visits.” That was the genesis of the idea for an app that he and Stanford colleague Daniel Palanker, PhD, would develop over the next several years, eventually cofounding DigiSight Technologies.
Monitoring Acuity and More
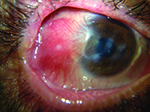
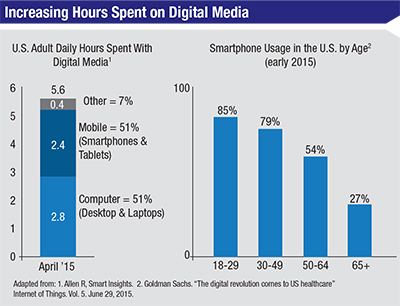 |
| Figure 1. Smartphones make up a significant portion of adults’ daily digital media use in the United States. Smartphone usage is growing across all age groups. |
To ensure that the test was well-correlated to in-office vision testing, the developers spent a lot of time making sure the on-screen letters accurately corresponded to lines of Snellen acuity. “We also had to adjust for the higher contrast of a screen compared to a standard eye chart,” says Dr. Blumenkranz. Extensive testing revealed that it didn’t matter very much whether the person tended to hold the device at 12 or 14 or 16 inches. “As long as they hold it the same way every time—and our data suggest that people naturally do this—the reproducibility is very high,” Dr. Blumenkranz says.
The test has been clinically validated3 and was recently listed with the Food and Drug Administration as part of a suite of tests called Paxos Checkup.
The other tests that patients can take from the Paxos Checkup app include contrast sensitivity and contrast acuity, inverse acuity, low-illumination contrast acuity, Amsler grid and a proprietary grid test (DigiGrid) and color discrimination. Patients can take one or more tests daily, weekly or as directed by their physician, with whom they must register prior to using the app. Test results are transmitted and stored in compliance with HIPAA privacy and security guidelines for protected health information. The physician’s office receives alerts when patients hit triggers set by physicians, such as losing two or more lines of vision, but doctors can also review all the test results for an individual patient plotted in a graph.
“It completely changes what I look at,” says Dr. Blumenkranz, who uses the app for home monitoring of his patients with age-related macular degeneration. “Instead of trying to make a decision from two data points—the visual acuity at the last two exams—I see a curve. The more often they test, the smoother the curve. At a glance, I can tell if the patient’s vision over the past month has been stable, trending up or down or fluctuating. It makes it much easier to pick up on subtle changes.”
The goal, he says, is to intervene before the patient’s vision “falls off the cliff.” He also believes having this kind of data can serve as a valuable safety net for patients, because it helps him identify which patients need to come in sooner than planned for their next injection.
“Patients love it,” Dr. Blumenkranz says. “It gives them something they can proactively do towards managing their disease, over which they otherwise have no control. I think it really reinforces the doctor-patient relationship.”
Mobile Imaging
 |
| Figure 3. The Paxos Scope device enables both anterior and posterior imaging of the eye. Its universal, spring-loaded mounting system fits and aligns with virtually any smart phone, regardless of its size and camera lens location. |
The device is lightweight and inexpensive. It was developed by two Stanford ophthalmologists, David Myung, MD, PhD, and Robert T. Chang, MD, who serve on the faculty at the Byers Eye Institute at Stanford. The two started working on the project together nearly four years ago when they saw the need for a better way for residents and physicians on call to send photos to their colleagues.
There were already a number of adapters available to connect a phone or camera to a slit lamp, but Dr. Myung said he felt that these didn’t meet the need at large. “There are many settings where there is no slit lamp available, such as a nursing home, primary-care setting or in many rural settings,” he says. “And even in the emergency department, there might not be anyone who is completely comfortable in the use of the slit lamp, or has the time to spend troubleshooting it if there are any problems.”
Ultimately, Drs. Myung and Chang—who published their original design in March of 2014— determined that they wanted a device that could be used on any phone.4,5 A variable-intensity external light source was necessary to provide light for fundus photos. That way, they wouldn’t have to rely on the phone’s internal flash (which can vary from one smartphone model to the next) and could take many photos without draining the phone battery. The intensity of the light can be adjusted for patient comfort and eye color. The mounting and lens-alignment system is also designed to adapt to nearly any size and dimension phone (See Figure 3).
 |
 |
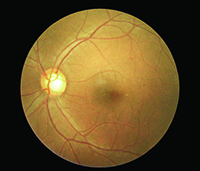
| Figure 4. A recent study found that Paxos Scope’s smartphone-acquired fundus photos demonstrated 91 percent sensitivity and 99 percent specificity to detect moderate nonproliferative and worse diabetic retinopathy, with good agreement between fixed camera and smartphone-acquired photo grades. |
Young ophthalmologists in training are already using their phones to share photos with an attending surgeon, he said, but may be doing so in ways that are not HIPAA-compliant. Paxos Scope securely transmits images to a Cloud server over WiFi or cellular signals without storing them on the phone.
A recent study that is forthcoming in the journal Retina found that the smartphone-acquired fundus photos demonstrated 91 percent sensitivity and 99 percent specificity to detect moderate or worse nonproliferative diabetic retinopathy, with good agreement between fixed-camera and smartphone-acquired photo grades (p<0.001).6 (See Figure 4)
The device is capable of capturing retinal images with up to a 56˚ static field of view. “Although the quality of the images is quite impressive given the modern smartphone camera quality, our goal was not to replace a fundus camera, but instead to obtain images quickly and easily that are good enough to aid referrals to specialists or remote recommendations,” says Dr. Chang. “In this way, we can augment communication and triage capabilities with additional photographic information.” Moreover, he said, “People were already taking photos with their smartphone but the magnification and lighting were not optimized for the eye; we wanted to improve this.”
Dr. Chang believes less-expensive, on-demand, mobile imaging holds the potential to expand access to care everywhere, particularly in underserved populations in the United States and abroad. Some examples include helping other health-care workers obtain photos in patients in nursing homes who haven’t been getting regular dilated exams, facilitating various eye disease screening camps, and even coupling photos with other parts of the eye exam that can be performed remotely. “The ultimate dream of a portable, full basic eye exam on a smartphone platform using a few small adapters is moving one step closer to reality,” he said.
Big Data
A third element of the platform that will soon launch is Paxos Analytics, which will give pharmaceutical companies real-time insights into their clinical study outcomes. In fact, it’s the data analysis part of the platform that is expected to provide much of DigiSight’s initial revenue.
| Scaling Mountains to Provide Eye Care | |||
The nonprofit Himalayan Cataract Project has been working to change that by improving eye-care training, infrastructure and the provision of high-quality care in Nepal and elsewhere. The organization supports a training center, the Tilganga Institute of Ophthalmology, that serves as a center of excellence for the developing world. It trains many teams of doctors and nurses from Asia and Africa, in an attempt to alleviate blindness by increasing local capacity and efficiency. HCP Board Director Matthew S. Oliva, MD, says the work provides a strong sense of shared values and commitment. “While I have really focused on expanding our sustainable development model, I still love sharing that moment of sight restoration with individual patients,” he says. Mobile health technology may help his organization overcome a major challenge. “It is often difficult for ophthalmic technicians and doctors in underserved areas to decide which patients would benefit from a trip to Kathmandu to receive subspecialist care,” he says. Dr. Oliva and his colleagues at HCP, including its co-founder Geoff Tabin, MD, fellow John Welling, MD, and David Chang, MD, have been collaborating closely with David Myung, MD, PhD, from Stanford and ophthalmologists at the Tilganga Institute of Ophthalmology in Kathmandu to deploy free Paxos Scope adapters in rural Nepal through a partnership between HCP, DigiSight and the American Society of Cataract & Refractive Surgery Foundation (See images, above). Given that most doctors at rural-health care centers in Nepal use cell phones and text messaging as their primary means of communication, he is convinced that a smartphone based technology can be an effective aid to telemedicine. “The Paxos Scope offers an elegant way to share patient information so that rural health providers can seek advice on patient care or facilitate a referral for follow-up care. We are optimistic this will lead to improved, comprehensive care for patients in Nepal,” Dr. Oliva says. —J.B. |
Eventually, physicians may also find the data analytics aspect extremely valuable for day-to-day patient care. “Once you aggregate a lot of data, we think there are some very compelling and interesting things that can be done with it, such as developing more sophisticated predictive capabilities,” says Mr. Foster. Analysis of the data could potentially lead to new insights about disease progression or therapeutic efficacy and allow doctors to more precisely personalize care to the individual patient.
“There is significant pressure on health-care systems in the United States to be accountable for high-quality care, while at the same time containing rising costs,” says Mr. Foster. “One way to accomplish this is to give expensive treatments like anti-VEGF injections only when patients actually need them, rather than on an arbitrary schedule that overtreats some patients, increasing costs through overutilization, while undertreating others and potentially increasing costs through higher rates of visual impairment.”
Although it seems at first blush that more information could overwhelm physicians who are already stretched to provide care to a growing senior population, Mr. Foster says more information can actually help doctors work smarter. The company’s internal analyses suggest, for example, that physicians spend only about 10 minutes per week reviewing the Paxos Checkup dashboard for all the patients doing at-home monitoring. “But in that short time, they can actually enable patients to engage more in their own care, and potentially create a more pleasant workflow experience and potentially improve outcomes,” Mr. Foster says. REVIEW
1. Fagerberg J, Kurkinen L. “mHealth and Home Monitoring,” Berg Insight Report, December, 2015. www.berginsight.com, accessed October 2015.
2. Allen R. Mobile Internet Trends Mary Meeker 2015 1. Smart Insights. Accessed December, 2015 at http://www.smartinsights.com/internet-marketing-statistics/insights-from-kpcb-us-and-global-internet-trends-2015-report/attachment/mobile-internet-trends-mary-meeker-2015-1/
3. Yu S-Y, Yang JH, Kim Y, et al. Reliability of the smartphone-based electronic visual acuity testing, ARVO, 2014.
4. Myung D, Jais A, He L, Blumenkranz MS, Chang RT. 3D Printed Smartphone Lens Adaptor for Rapid, High Quality Retinal Imaging, Journal of Mobile Technology in Medicine, 2014, Vol. 3, Issue 1: 9-15.
5. Myung D, Jais A, He L, Blumenkranz MS, Chang RT. Simple, Low-Cost Smartphone Adapter for Rapid, High Quality Ocular Anterior Segment Imaging: A Photo Diary, Journal of Mobile Technology in Medicine, 2014, Vol. 3, Issue 1: pp. 2-8.
6. Toy B, Myung D, He L, et al. Smartphone Ophthalmoscopy Adapter as an Inexpensive Screening Tool to Detect Referral-Warranted Diabetic Retinopathy. Retina 2016, In press.