Late Dislocations
Recent studies have looked at in-the-bag lens dislocations and their causative factors, and have mentioned that their incidence may be increasing.
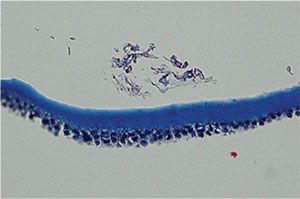 |
| Photomicrograph of the anterior capsule with exfoliative material seen anteriorly in a case of spontaneous IOL dislocation. |
Researchers in a joint U.S./German study in 2015, designed to analyze the IOL-capsular bag complexes in eyes in which the IOLs subluxated or dislocated, reported that they’ve received an increasing number of specimens related to in-the-bag subluxation or dislocation in recent years.1 They refer to a previous study they performed in 2009 that looked at the possible causes of 86 subluxations or dislocations, and note that just two of the specimens were submitted between 2000 and 2003 while 84 were submitted between 2006 and 2008.2 A recent meta-analysis from Spain that looked at dislocation studies found that late in-the-bag subluxation or dislocation has been “reported with increasing frequency, leading to concerns of a pending large increase in IOL dislocations needing surgical intervention.”3 The researchers also cite a large, retrospective, population-based study that found the cumulative risk of IOL dislocation increases slowly with time, with a 1.7-percent risk after 25 years.4 Though the rate of surgery related to late dislocations is low in the population-based study, the Spanish researchers say that the number of pseudophakes in the Western world is growing quickly as a result of improvements in phaco, longer lifespans and other factors, and that this might mean an increase in late dislocations.3
Given these studies, though, is this a problem surgeons should be worried about? Nick Mamalis, MD, director of the Ophthalmic Pathology Laboratory at the University of Utah’s Moran Eye Center, isn’t so sure. “The key question is: As we do cataract surgery on younger and younger patients, do we see them having more of a chance of spontaneous dislocation of the IOL within the capsular bag as the years go by?” he muses. “The good news is that we haven’t seen signs of that, at least in the lenses that have spontaneously dislocated that are sent to our lab. In these lenses, the most common reason is pseudoexfoliation. When we did our first major lab study on that, we found that half of the specimens had dislocated secondary to exfoliation syndrome. But then, when we worked further with our German colleagues who sent us the IOLs within the capsular bags to analyze, even though a third of the patients had diagnosed exfoliation prior to the dislocation we found that actually two-thirds of the cases had exfoliation.”
The Capsulorhexis Connection
Another factor that some surgeons point to regarding a possible increased incidence of dislocations is the capsulorhexis. In a letter published in Ophthalmology, Los Altos, Calif., surgeon David Chang reported on two patients who had late dislocations, commenting, “The incidence of this delayed complication appears to have skyrocketed after universal adoption of the capsulorhexis technique.”5
“I think one of the crucial issues in spontaneous IOL dislocation within the capsular bag is the use of a capsulorhexis,” says Dr. Mamalis. “In the past, when we were doing can-opener capsulotomies and extracapsular surgeries, we just weren’t seeing it happen. I think there’s something to the idea that a good capsulorhexis, and an implant placed completely in the bag, can somehow, over many years, possibly lead to some constriction of the bag, some phymosis and some additional stretching of the zonules which could, in theory, put the patient at risk for a spontaneous dislocation. I say ‘in theory’ because we haven’t seen any signs of this in the lab at this point.”
George O. Waring IV, MD, medical director of the Medical University of South Carolina’s Magill Vision Center and assistant professor of ophthalmology and director of refractive surgery at the MUSC’s Storm Eye Institute, was one of the first surgeons to help surgeons and patients understand the term dysfunctional lens syndrome, and notes that nothing about the capsulorhexis has been definitively shown to cause dislocations down the line. He says neither femtosecond capsulotomies nor manual capsulorhexes will put a lot of stress on the zonules. “As far as capsular contraction goes, this would be an opportunity for lens epithelial cell eradication, and to date we don’t have a way to do that,” he says.
Lessons from Younger Eyes
Dr. Waring says ophthalmologists’ experiences with the youngest of patients may help allay some fears of long-term dislocation.
“The best line of reasoning for this is pediatric cataract surgery,” Dr. Waring says. “With refractive lens exchange, you’re probably talking about someone who’s already lived 50 years with his natural lens and is getting a lens replacement. But if you look at a cohort of infants or toddlers who are having IOLs implanted, they have their implants for more than 70 or 80 years, and we don’t have any evidence that suggests that they’ll have additional zonular issues because they have an implant. I think that we feel secure that this is still basically a non-concern.”
Ultimately, Dr. Mamalis says long-term dislocations should be on the surgeon’s radar, but maybe not a source of worry. “We haven’t done cataract surgery with a capsulorhexis in people in their 40s and then followed them for 40 years because capsulorhexis hasn’t been around for 40 years,” he says. “We just don’t know the answer regarding the risk of dislocation in these patients. I can say we haven’t seen signs of it actually occurring, which is reassuring, but we just don’t know. It’s not a procedure that I would say we shouldn’t be doing, but it’s something we should keep an eye on.” REVEW
1. Liu E, Cole S, Werner L, Hengerer F, Mamalis N, Kohnen T.
Pathologic evidence of pseudoexfoliation in cases of in-the-bag intraocular lens subluxation or dislocation. J Cataract Refract Surg 2015;41:5:929-35.
2. Davis D, Brubaker J, Espandar L, Stringham J, Crandall A, Werner L, Mamalis N. Late in-the-bag spontaneous intraocular lens dislocation: Evaluation of 86 consecutive cases. Ophthalmology 2009;116:4:664-70.
3. Ascaso FJ, Huerva V, Grzybowski A. Epidemiology, etiology, and prevention of late IOL-capsular bag complex dislocation: Review of the literature. J Ophthalmol 2015;2015:805706. Published online 2015 Dec 21.
4. Pueringer S. L., Hodge D. O., Erie J. C. Risk of late intraocular lens dislocation after cataract surgery, 1980–2009: A population-based study. Amer J Ophthalmol 2011;152:4:618–623.
5. Chang D. Letter to the editor: Prevention of bag-fixated IOL dislocation in pseudoexfoliation. Ophthalmology 2002;
109:11:1951.