While search engines are useful, sometimes it’s nice to have a dedicated, doctor-vetted app to look up what you need. Here are five reference apps developed by doctors to consider downloading.
Acronym Help
“Ophthalmology uses acronyms in our documentation and notes probably more than any other field,” says OE Acronyms (Ophthalmic Edge) co-director Grayson Armstrong, MD, MPH, a comprehensive ophthalmologist and medical director of Ophthalmic Emergency Services at the Massachusetts Eye and Ear Infirmary. He presented the app at the Retina Society meeting in Chicago. He works on the program alongside Nimesh A. Patel, MD, a pediatric and adult retina specialist at Mass EE and app creator Yale L. Fisher, MD, of Vitreous Retina Macula Consultants of New York. Dr. Fisher founded Ophthalmic Edge as a 501(c)(3) non-profit.
“This app can help nurses, internal medicine doctors, technicians, medical students, patients and others who might not understand the language of what we do in our field,” he explains. “Misunderstanding certain acronyms can be dangerous. Take ICP, for example. In internal medicine and neurology, this means intracranial pressure. In ophthalmology, it’s intermediate capillary plexus for uveitis. Even within ophthalmology, not all subspecialists are familiar with the acronyms of other subspecialities. This limits our ability to provide team-oriented care.”
Dr. Grayson says the Cares Act, which gives patients access to their records and notes, has also introduced the potential for patients to misunderstand ophthalmic acronyms. “This may lead to their taking the wrong medication or the wrong dosage or thinking they need a certain treatment,” he says. On a lighter note, he points to the acronym PEE, punctate epithelial erosion. “It’s a common finding, but patients get confused, thinking we’re talking about pee in their eye.”
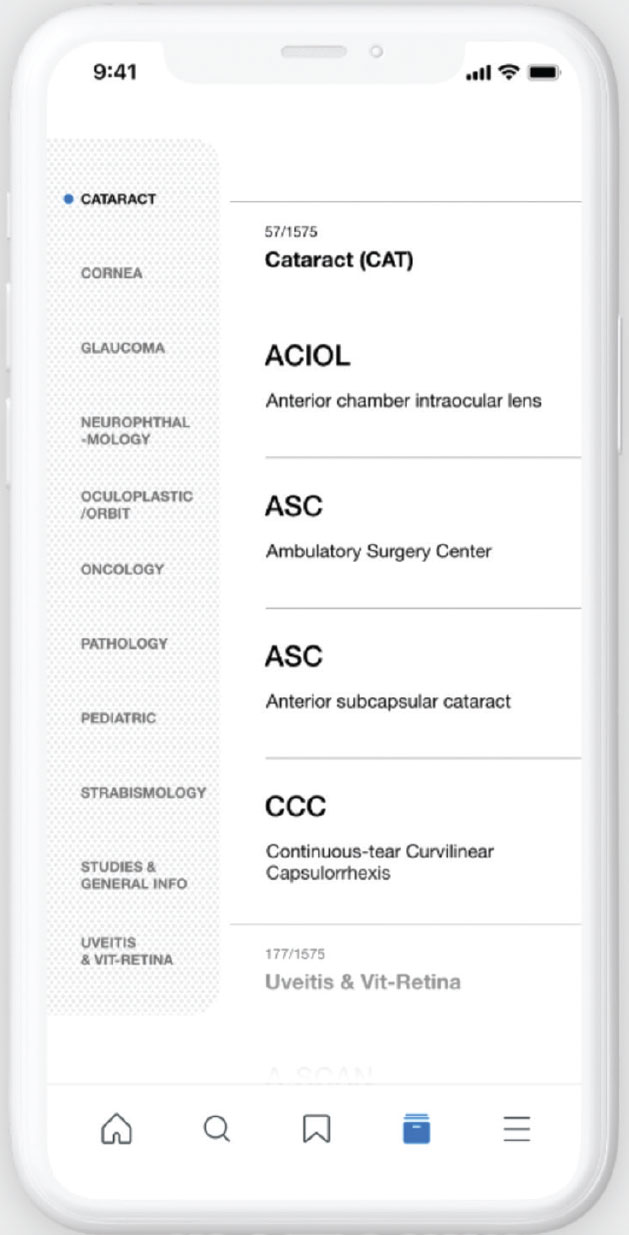 |
| OE Acronyms is a free, open-source app that currently includes more than 2,600 ophthalmic acronyms. The developers say it helps to prevent confusion among those who aren’t familiar with the many acronyms ophthalmic subspecialties use. Click image to enlarge. |
The free, open-source app covers all subspecialties of ophthalmology and currently includes more than 2,600 acronyms. It had 1,152 users as of September and more than 63 contributors. “Anyone can contribute an acronym,” says Dr. Armstrong. “In the online form, you put in the acronym, provide a short description, and then add your name as a contributor. We want to give people credit for their work, as well as ensure it’s a legitimate acronym from a legitimate individual.”
The app also includes major clinical studies’ acronyms, such as MARINA, PIVOT and HARRIER. “There’s a brief description of each trial’s key findings,” says Dr. Armstrong. “You can save favorite acronyms and trial nicknames and make flashcards to study.”
When searching for an acronym, users can search by the letters or by the clinical findings or diagnosis. Each acronym and definition are categorized by subspecialty, so users also have the option of looking only at the oculoplastics acronyms or only at the retina acronyms, for example.
Dr. Armstrong says he uses the app most often during grand rounds. “There are a lot of acronyms being thrown around by ophthalmic subspecialists,” he says. “I can look them up quickly. It’s also convenient for technicians. My techs do all the workup and intake for my patients, but I’m a comprehensive ophthalmologist, so they don’t often see a lot of things for retina, glaucoma or cornea in my notes. They can look up the acronyms on their phones to check what testing or work-up needs to be done before the patient sees me. It helps streamline the clinic.” OE Acronyms is available for Android and iPhone. For more information, visit oeacronyms.com.
Plaquenil Dosing
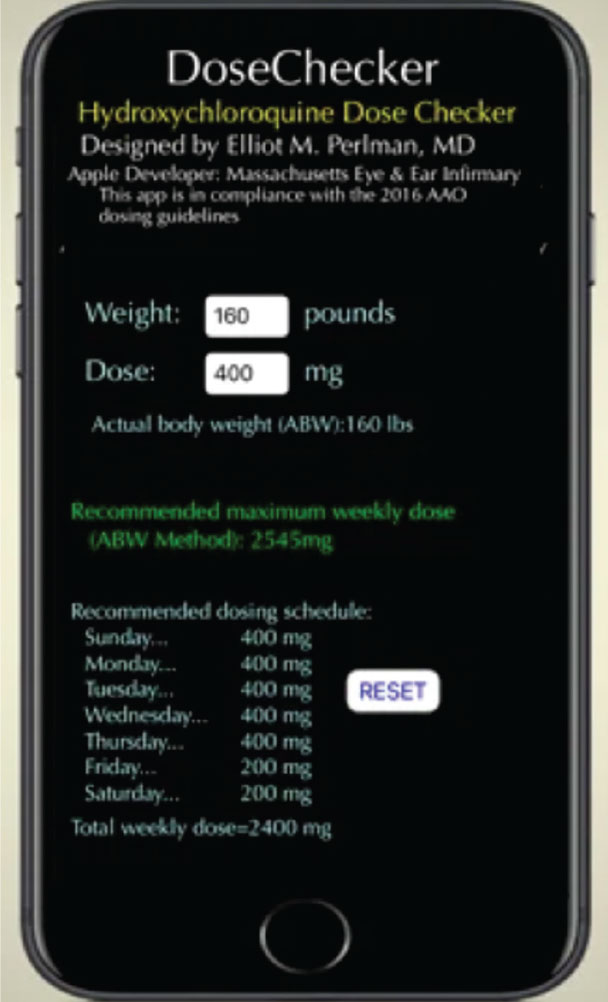 |
| DoseChecker offers hydroxychloroquine dosing recommendations in a weekly schedule using a combination of 400-mg and 200-mg daily doses because the drug is available only in 200-mg tablets. Click image to enlarge. |
DoseChecker from the Massachusetts Eye and Ear Infirmary is an app that helps clinicians determine a safe dosing regimen for hydroxychloroquine. The current version of the app uses only Absolute Body Weight to calculate dosing toxicity, in accordance with the 2016 AAO guidelines. According to this method, which assumes the drug is distributed evenly throughout muscle, skin and fat, the maximum daily dose is 5 mg/kg/day x ABW (kg).1
Long-term use of hydroxychloroquine puts patients at increased risk for developing hydroxychloroquine retinopathy. The app provides an adjustable weekly dosing schedule using a combination of 400-mg and 200-mg daily doses, since the drug is available only in 200-mg tablets. Dosing recommendations are always within the approved drug labeling and for use only by clinicians, which obviates the need for FDA regulation as a class I mobile medical device.1 In the published paper on the app, the creators say prescribing doctors should consider cumulative dose, concomitant retinal disease and presence of systemic disease, which may affect a patient’s risk for developing toxicity.1 Additionally, ophthalmologists should refer to the AAO recommendations for screening and follow-up. DoseChecker is available in the App Store.
Virtual Call Bag
You’ve probably heard of Eye Handbook (Cloud Nine Development), or maybe even have it on your phone. It’s one of the most downloaded eye-care apps, and it has a host of features, including vision-testing tools, various calculators, an atlas of eye images, a collection of educational videos, a coding tool and a new online forum.2
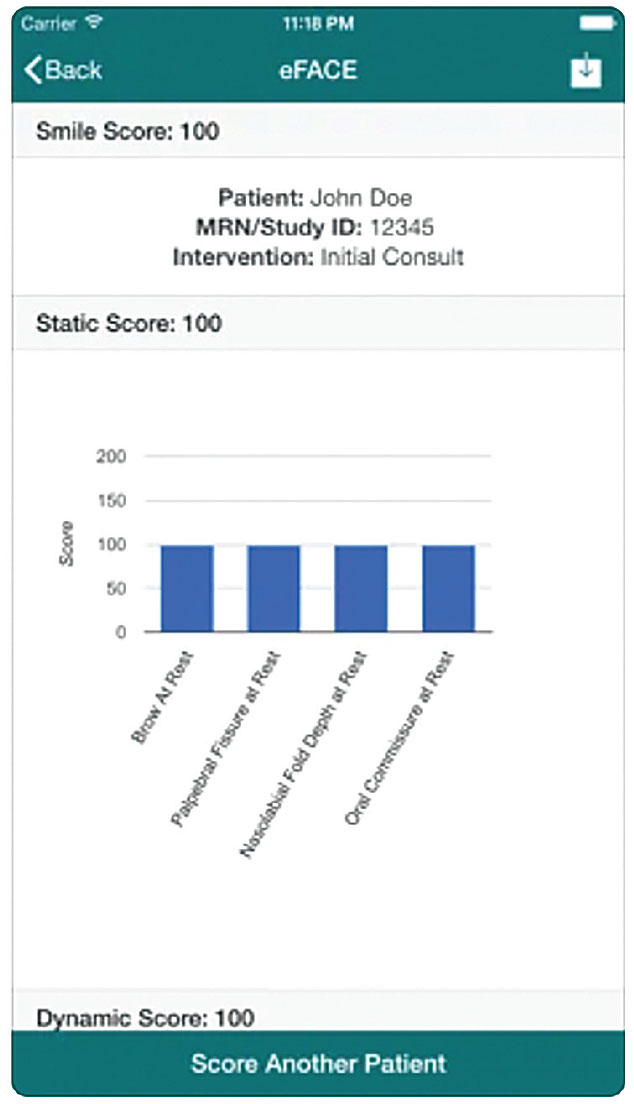 |
| The eFACE app from Massachusetts Eye and Ear Infirmary helps clinicians identify facial palsy. It performs static readings, dynamic movement readings and synkinesis scores, and can be used to obtain clinician-rated scores for 16 separate facial function features. Click image to enlarge. |
Vinay Shah, MD, a vitreoretinal specialist and clinical associate professor at Dean McGee Eye Institute, University of Oklahoma College of Medicine, created the app with Ken Lord, MD, of Retina Associates of Southern Utah, when they were residents at the University of Missouri Kansas City. Rohit Krishna, MD, director of the glaucoma service at UMKC School of Medicine, is also a partner.
“It’s kind of like a one-stop shop,” Dr. Shah says. “It’s eye-care-facing, but many emergency room doctors, primary care doctors and neurologists use the app as well.
Some patients use it to test their own vision. I use the vision-testing tools whenever I’m doing consults or seeing patients in the emergency room. I don’t have to carry around a bunch of different charts.” He also frequently refers to the BMI and Plaquenil dosing calculators, as well as the coding feature.
“We update the content once or twice a month,” he explains. “The Eye Atlas images are contributed from other doctors or from us. We also curate the educational videos mainly from YouTube, so they’re all in one place. The Forums are useful for sharing cases or getting some ideas from other doctors. There’s a built-in media consent for sharing images, but users should also check the consent requirements unique to their institutions.” Eye Handbook is available for Android and iPhone. For more information, visit eyehandbook.com/EHBweb.
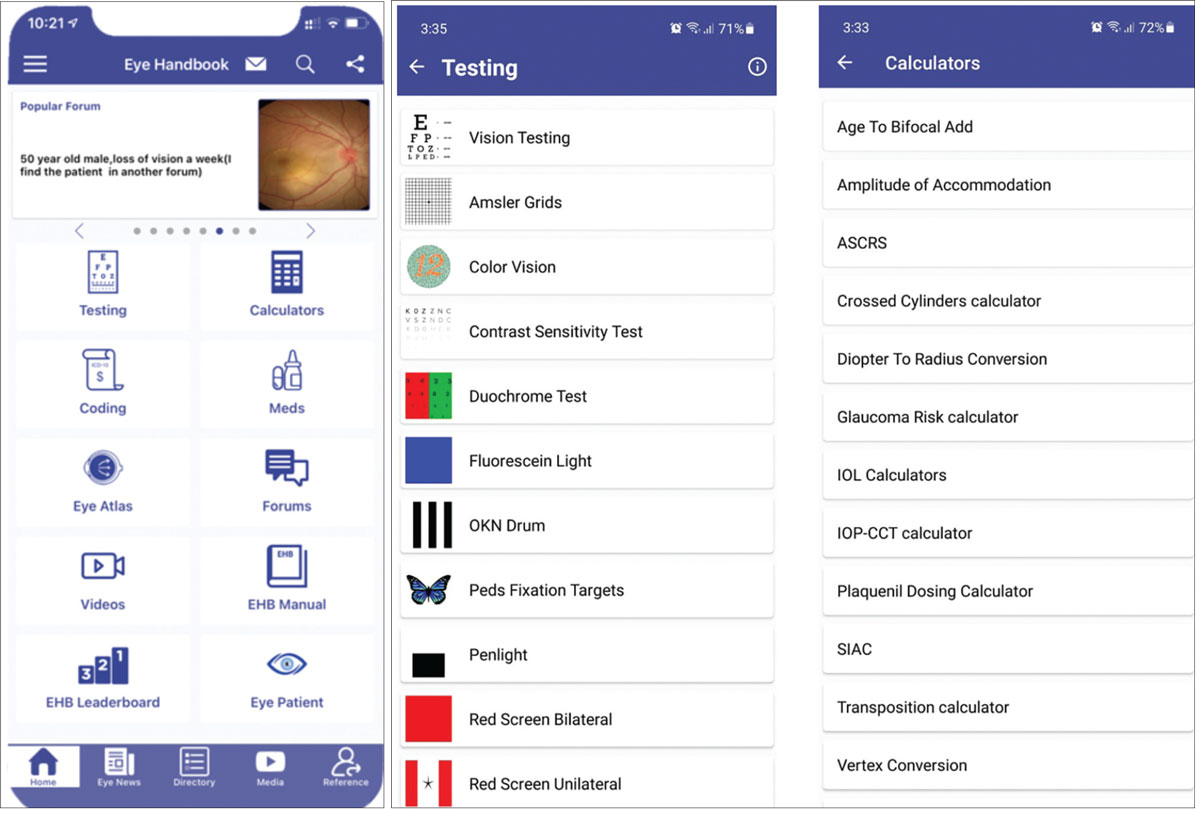 |
| Eye Handbook is a comprehensive tool that includes educational material, an online forum, an atlas of eye images and coding information. Click image to enlarge. |
Facial Palsy Detection
Two new online resources can help detect facial palsy. The eFace (Massachusetts Eye and Ear Infirmary) app is a digital, clinician-graded facial function scale that provides quantitative and graphic depictions of facial function scores in patients who suffer from unilateral facial paralysis. It performs static readings, dynamic movement readings and synkinesis (misrouting) scores, and can be used to obtain clinician-rated scores for 16 separate facial function features. In studies, it’s been well-received by facial nerve experts3 and has demonstrated reliable, reproducible and straightforward digital clinical measures for assessing facial paralysis.4 It’s available in the App Store for $9.99.
There’s currently no standardized assessment of facial palsy, however, and clinician-graded scales like the eFace are still subjective and limited by observer bias. One proposed way to move toward conformity in grading is by using artificial intelligence. Researchers at the Massachusetts Eye and Ear Infirmary and the Florida Institute of Technology’s biomedical engineering program developed a machine-learning program called auto-eFace and compared it to the eFace. They found that the auto-eFace predicted more asymmetry in normal patients and less asymmetry in patients with flaccid palsy and synkinesis, compared to clinician grading.
In the study, clinician-graded eFace assessment was performed on 160 photographs from the center’s Standard Facial Palsy Dataset, and a Python script was used to generate auto-eFace scores on these same photographs. Auto-eFace produced significantly lower scores than the eFace for normal faces (93.83 ±4.37 versus 100 ±1.58, p=0.01). The machine-learning program reported better facial symmetry in patients with flaccid paralysis (59.96 ±5.8) and severe synkinesis (62.35 ±9.35) than clinician-graded eFace (52.2 ±3.9 and 54.22 ±5.35, respectively, p=0.080 and p=0.080, respectively). The Auto-eFace software is available online for free.
Smart Coding
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
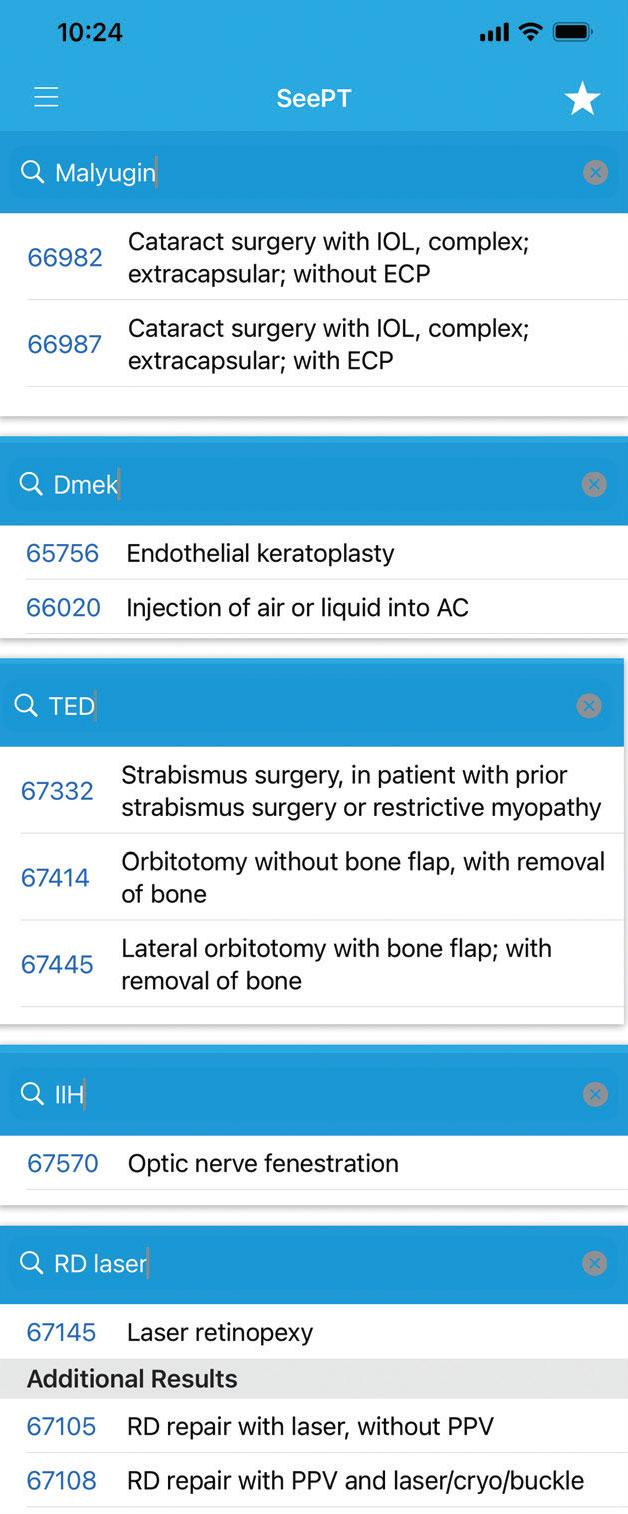
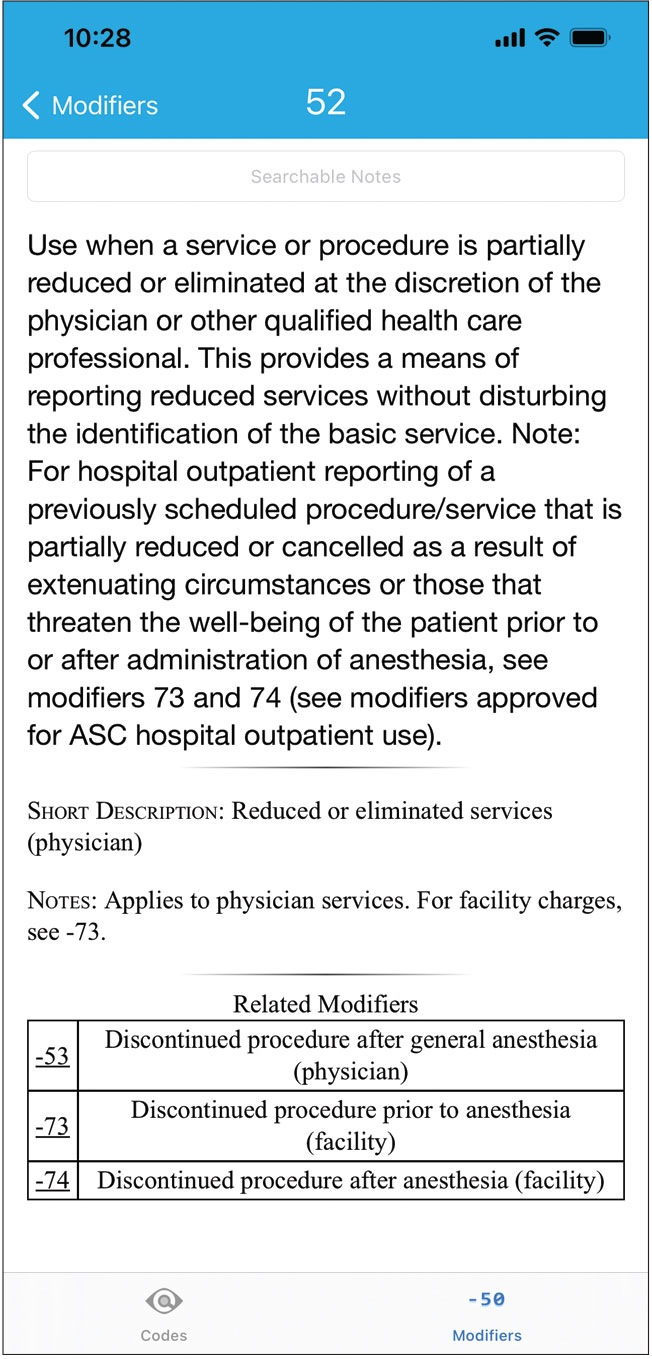
“SeePT is a licensed app that takes the CPT codes applicable to ophthalmologists and puts them in an accessible, searchable form that allows intelligent searches based on the natural language ophthalmologists use to think about procedures,” says developer Evan Schoenberg, MD, a cornea, cataract and refractive specialist in Atlanta. He and Evan Silverstein, MD, a pediatric ophthalmology specialist and an assistant professor in the department of ophthalmology at Virginia Commonwealth University, co-own a company called See Vision that develops medical apps.
What is smart coding? “It takes into account how ophthalmologists think,” says Dr. Schoenberg. “If you were to search a database for the CPT code for cataract surgery and you typed in ‘cataract,’ you would eventually find the right code, but if you don’t know the specific language used in the database, finding the right code becomes more difficult. For a simple example, say you’re looking for the code that covers the use of a Malyugin Ring during cataract surgery. The official description of a complex cataract surgery—‘requiring devices or techniques not generally used in routine cataract surgery (e.g., iris expansion device…’—doesn’t include the words ‘Malyugin Ring,’ but the app knows to cross-reference ‘Malyugin’ and turn up the right code. A less common example might be for an implant procedure. Say you’re doing a brand-name one like Dextenza. You may not realize it’s listed in the database as a ‘dexamethasone implant.’”
Dr. Schoenberg says that if you’re using abbreviations, the system automatically expands them into familiar terms. “If you type in ‘IOL’ because you’re doing an IOL exchange, you’ll get the right code instead of having to guess the specific words used in the database.”
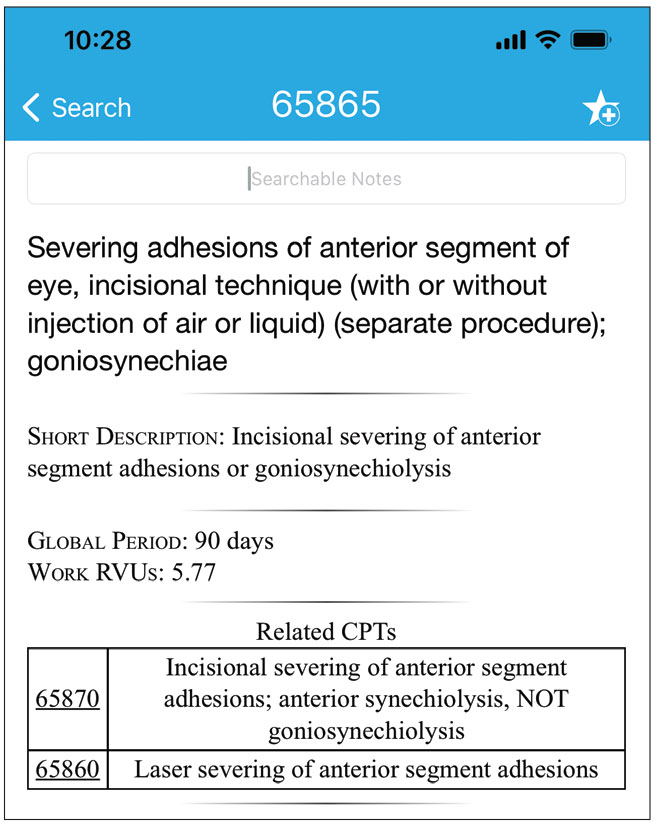 |
SeePT features smart-search technology that enables clinicians to quickly look up the codes they need using the natural language with which they think about the procedures. Click image to enlarge. |
The new CPT codes go live on the app for a seamless transition, so you’re always using the most current version of the codes, Dr. Schoenberg explains. “The AMA requires a code license on a yearly basis. There’s a free trial built into the app, which the AMA allows. Users will be notified when they need to license the new year’s codes. If you choose not to, you’ll still have access to the previous year’s codes, but upgrading is recommended.”
The yearly AMA code license is $24.99, which goes directly to the AMA. The smart search functions, RVU database and cross-referencing features of the app require a yearly subscription of $49.99. Dr. Schoenberg notes that purchasing the CPT code book, which doesn’t include intelligent search functions, costs $85. “With the app, you have more function and convenience for less money,” he says. “It pays for itself when you consider the ramifications of coding just one procedure incorrectly.” SeePT is available in the App Store. For information, visit seevisionllc.com.3
1. Perlman EM, Greenberg PB, Browning D, et al. Solving the hydroxychloroquine dosing dilemma with a smartphone app. JAMA Ophthalmol 2018;136:2:218-219.
2. Lord K, Shah VA, Krishna R. The Eye Handbook: A mobile app in ophthalmic medicine. Mo Med 2013;110:1:49-51.
3. Banks CA, Jowett N, Azizzadeh B, et al. Worldwide testing of the eFACE facial nerve clinician-graded scale. Plast Reconstr Surg 2017;139:2:491e-498e.
4. Banks CA, Bhama PK, Park J, et al. Clinician-graded electronic facial paralysis assessment: The eFace. Plast Reconstr Surg 2015;136:2:223e-230e.



