 |
Timothy G. Murray, MD, MBA, President of the American Society of Retina Surgeons, knew he was insisting on seemingly unforgiveable—but necessary—medicine for his colleagues when he participated in the creation of a now-infamous virtual “ban” on routine patient visits and all surgeries except for emergent/urgent procedures during the first month of the COVID-19 outbreak. Now that the moratorium is over—with retinal specialists and other ophthalmologists planning a phased, regional return to work under the guidance of public health experts and local government leaders—he believes retinal specialists will be able to step up and meet pent-up demand for care without undermining efforts to flatten the regional curves of the deadly pandemic.
“Many of us practice medicine in small groups, following strict infection control measures and performing outpatient procedures,” he says. “We have the needed flexibility, nimbleness and practice discipline to keep our patients and ourselves safe—and also cease operations or ramp back up up, as needed, in response to local epidemiological data and other inputs. Here, as COVID-19 continues its ever-branching and uneven penetration of the national patient population, Dr. Murray and other experts offer advice to help you resume—or prepare to resume—patient care, depending on your local circumstances.
Effects of the Recent Slowdown
 |
Many retinal surgeons cut chunks out of their schedules even before March 18, when the American Academy of Ophthalmology, representing the consensus of the American Society of Retinal Surgeons and all other major societies in ophthalmology, urged ophthalmologists to suspend routine patient visits and restrict their activities to emergent or urgent care/surgery. On April 17, however, after the release of White House guidelines on “Opening Up America Again,” David W. Parke II, the chief operating officer of the AAO, announced in an emailed letter to all AAO members that it was “time to consider the process of reopening ophthalmology care,” based on “local and state governments, on public health authorities interpreting local patterns of disease, on testing availability, on institutional policies and ultimately on individual ophthalmologists. While we closed routine practice nationally, we will open locally.” (See “Reopening Ophthalmology and America” below.)
“We needed to put those temporary restrictions in place to help get the disease somewhat more under control,” says Dr. Murray, who is also founding director and CEO of Miami Ocular Oncology & Retina. “But that first month of significantly reduced care involved a lot of sacrifice that’s left lasting effects. Some retina practices went weeks without seeing any patients. Some practices even closed. Our hope is that surgeons can get back on their feet by adapting to our new way of practicing. We hope to provide guidance targeted at returning to practice in the same way that we provided guidance regarding practicing during the earlier stages of pandemic.”
Staying Stable
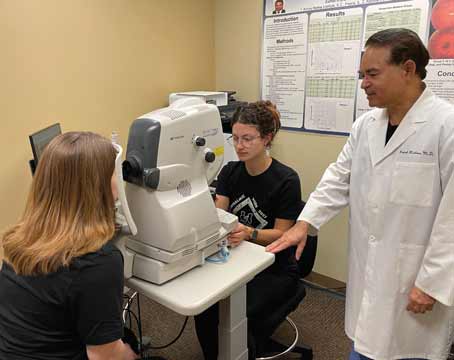
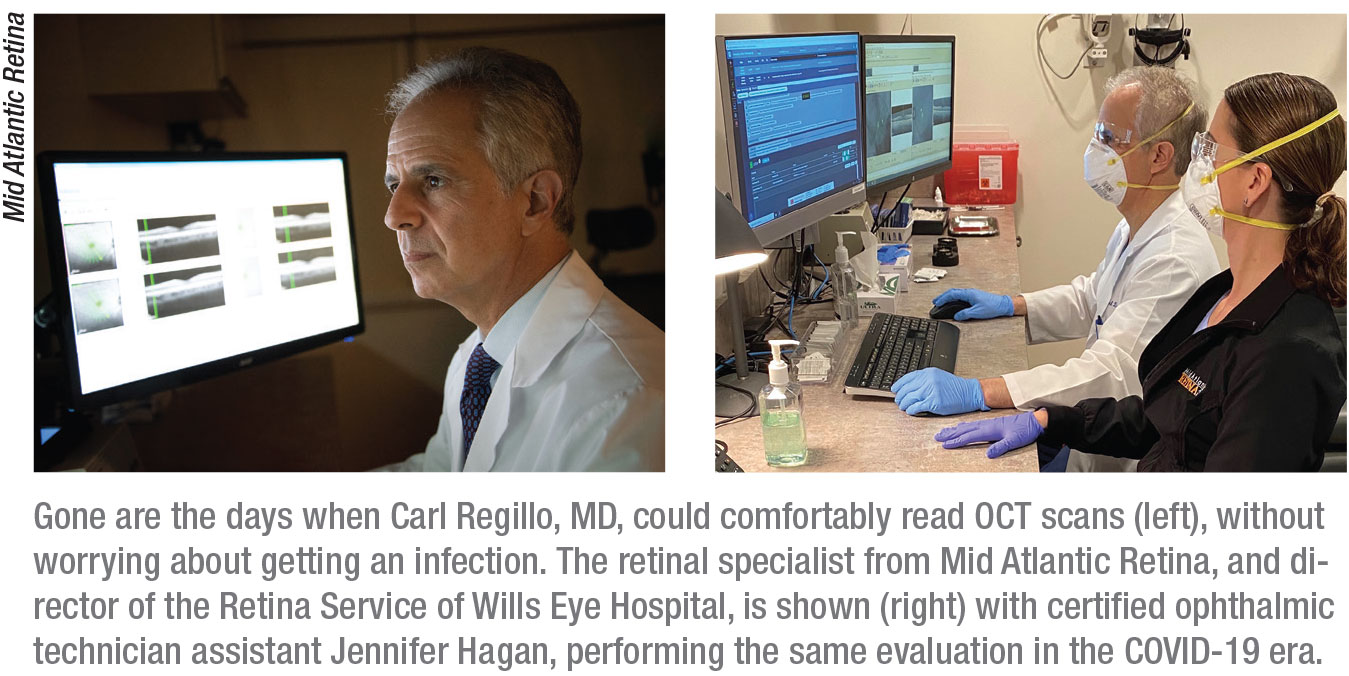
Jim Vander, MD, president of Mid Atlantic Retina, the Retina Service for Wills Eye Hospital, which has 18 locations in Pennsylvania, New Jersey and Delaware, says his independent private practice responded to the slowdown by submitting a successful application for a Paycheck Protection Program loan before the PPP’s initial $349 billion offering ran out of funds in mid-April, two weeks after the loan program was launched.
 |
The PPP is part of the $2.2 trillion Coronavirus Aid, Relief, and Economic Security Act (CARES Act), signed into law on March 27, which is designed to provide assistance to small and large businesses and displaced workers affected by the pandemic’s nationwide shutdowns in March through May. An additional $310 billion allocation was approved by Congress to replenish the PPP as part of a $484 billion coronavirus relief bill fund for distressed businesses and individuals when this issue of Review was being printed.
Mid Atlantic qualifies for the PPP loan because it remains a private practice, as opposed to being a part of a private equity firm, which would’t qualify for these loans. Mid Atlantic is categorized by the SBA as a “small business concern,” which is usually (but not always) defined as having 500 or fewer employees. Like the president of any other small business affected by the pandemic, Dr. Vander plans to apply his practice’s loan to the cost of payroll (except for employees earning more than $100,000 per year) and approved administrative expenses, paying for two month’s worth of these costs. Under the loan terms, the portion of the PPP loan that meets payroll will be forgiven by the federal government and must meet 75 percent of the total loan value. The practice will need to repay the balance of any borrowed amount at 1-percent interest, beginning within six months and ending within two years.
Dr. Murray, the ASRS president, also secured a PPP loan to stabilize his practice’s financial health. “I applied early, using my existing banking relationship,” he says. “Luckily I was able to clear many of the hurdles associated with the PPP loan process and, in fact, my practice just received its PPP funding. Importantly, we’re using a unique account for PPP funds to allow better tracking of all usages, especially focused on obtaining loan forgiveness at the conclusion of the loan term.”
Tapping Federal Funds
If you plan to tap into future PPP or other CARES Act loan funds that may available, Drs. Murray and Vander recommend using a bank that’s familiar with the needs of smaller clients, which typically include medical practices. Preferably, you should have an existing relationship with the lender. Mid Atlantic Retina benefited from the help of Bryn Mawr Trust, headquartered in Bryn Mawr, Pennsylvania, which Mid Atlantic has worked closely with for many years.
“These CARES Act programs are in Bryn Mawr Trust’s wheelhouse,” says Dr. Vander. “If you’re a large bank that deals with large corporate customers, the PPP and other loan programs coming down from the federal government through the SBA may represent a whole different world and mindset. Our previous experience with very large national banks was a struggle after the financial collapse of 2009. These enormous institutions didn’t seem to have the people and systems in place to deal with a corporate structure and size like ours.”
Easy Does it
 |
John T. Thompson, MD, one of three partners at Retina Specialists, with offices in Towson, Frederick, and Columbia, Maryland, is not endorsing or participating in a federal assistance program. His practice’s 30-member staff is working reduced hours, tackling administrative tasks. “At this point, we’ve shifted some clinical people to the front desk to help with a high volume of phone calls that are coming in from patients who need to discuss rescheduling issues and related matters,” Dr. Thompson says.
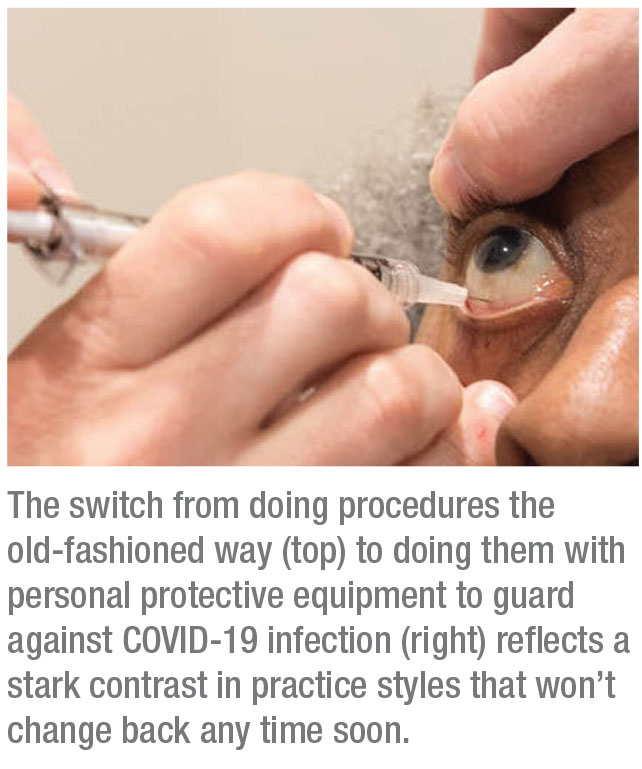
Each of the practice’s offices is also reducing costs by scheduling one physician at a time, Dr. Thompson notes. When the practice begins to get busier again, he expects the staff to be ready to help ramp up the volume of visits efficiently, having developed experience working with COVID-19 practice safeguards. “Each patient visit involves steps that require more time because of the need for screening, cleaning areas involved in the patient visit and taking other precautions,” he notes.
Dr. Thompson admits finances are a concern and recommends adjusting your practice budget so that future revenues can compensate for the lower receivables during the recent slowdown. “Because of the way our medical billing works, we’re fine right now. We’re collecting for services provided two to three months ago,” he says. “Soon, we’ll need to contend with a substantial decrease in revenue from the clinical side of our practice. You need to keep in mind that most office-based practices have overhead that’s 50 percent. So if your volume goes down by more than half, it essentially means you’re barely covering your expenses.”
One approach to avoiding cost over-runs is to furlough staff, with the intention of bringing them back when the practice gets busy again. Mid Atlantic Retina, which is preparing for a fiscally challenging second half of this year, has temporarily furloughed about 40 percent of the practice’s employees while retaining their benefits during the recent slowdown. All retinal specialists began working three-quarters of their regular daily hours. Dr. Vander, the Mid Atlantic president, said the practice was still preparing for how and when to further open its practice when this publication was being printed.
“We do all of our work in ‘outpatient facilities,’ some ambulatory-surgery-center-based, and some hospital-based,” Dr. Vander explained after the release of the White House guidelines and the Academy’s conditional lifting of restrictions. “We’re just discussing how to resume elective surgery and can’t tell you anything definitive yet.”
New Systems
Specialists recommend introducing systems and protocols that improve efficiency, safety and quality of care under the unique circumstances of the pandemic. Dr. Vander says Mid Atlantic will continue to follow three priorities. “The first one, for which there is no flexibility, is safety,” he says. “We make sure everyone is properly equipped and that our protocols are followed to protect our patients, employees, doctors and our families. Priority number two is managing the needs of our patients, and priority three is managing our finances. All three of these priorities are intertwined. We’ve established the types of patients who need to be seen for anti-VEGF injections and for new symptoms suggesting potentially acute problems, reflected by flashes and floaters, sudden pain and severe vision loss. We’ve verified that we have the materials and the protocols to see them and, based on that, determined the number of people that we need to keep employed onsite.
“We’ve also had a number of employees working from home,” he continues. “Reducing the number of the people in the office has been important. It’s not good for safety if you have too many people standing around and chatting. We’ve reduced the need for personal protective equipment by reducing the number of people involved. We’re starting to get a handle on the patient numbers—who is showing up and what those visits are like. We’ve structured the visits with the most efficiency and safety in mind. Going forward, we will have to bring some of those people back from furlough, and we hope to bring all of them back.”
Managing Surgical Flow
Like most retinal practices, Mid Atlantic has had to limit surgeries to retinal detachments, infected eyes (endophthalmitis) and miscellaneous emergent cases such as trauma. Timely surgery has also been indicated for vitreous hemorrhage related to an acute retinal tear and a posterior vitreous detachment. When elective procedures are added to the mix, Mid Atlantic will continue with innovative protocols developed for surgery in the COVID-19 era. Wills Eye Hospital in Philadelphia, where Mid Atlantic performs operations, has dedicated an operating room to cases involving COVID-19-positive or presumed-positive patients, using a negative air flow environment, according to Dr. Vander. The anesthesia department has established protocols for managing the airways of vulnerable and COVID-19-positive patients. These safeguards will remain in place indefinitely, accommodating increased procedures while the virus remains far from eradicated, according to Dr. Vander.
“We also have a COVID-19-positive treatment room, separate from the OR, at Wills,” says Dr. Vander. “So if we have to do a laser treatment or pneumatic retinopexy on a patient who is at high risk or known to be positive, we bring the patient directly into that room, wearing full protective gear during the encounter. A deep cleaning is done after the procedure. Our practice has contributed a laser and a cryotherapy unit for use in that room while we continue to deal with the virus. Only COVID-19-positive and presumed-positive patients will be treated in these rooms.”
As time passes, Dr. Vander says the doctors at Mid Atlantic Retina will need to care for more patients who fit the description of high-risk or infected. “Soon the issue we’ll have to wrestle with is how to deal with patients who were previously infected,” he notes. “When can you let them back into your office? How do you handle the patient who has been exposed because of contact with an infected loved one? For example, how should we handle a man who gets a retinal detachment the day after his wife has been very symptomatic and has tested positive?”
Managing Office Visits
During March and April, Mid Atlantic Retina conducted injection visits and allowed for the care of the acute cases listed earlier. As ophthalmology practices stir back to life, Vander expects to care for more referral patients and will consider when to resume six-month and 12-month follow-up visits that have been postponed indefinitely.
To maintain social distancing and other precautions, Mid Atlantic will continue to minimize exposure to the staff and limit access to different rooms in the office. “We screen patients as they come to the door and typically allow only one or two patients in our waiting room,” says Dr. Vander. “The patients appreciate that we’re there for them and that there are no other patients around. When they approach the front desk, they’re asked to continue walking to a room, which functions as their vision room, exam room and injection room. So there’s a minimal amount of contact, physically, with the space, equipment and staff. All surfaces touched by the patient are assumed to be contaminated and are wiped down. We don’t rely on gloves to protect against the virus because gloves are no better than your hands if you’re touching everything with your gloves on.”
Because of these approaches, patients get in and out of the practice faster than ever, says Dr. Vander. “If a back-up of patients develops, we ask the waiting patients to wait in their cars, and we send them a text message or call them on their cell and say, ‘Okay it’s your turn. Come on in.’ ”
To respond to the continuing shortage of personal protective equipment, the practice asks patients to wear their own masks, a request that’s posted on the practice website and mentioned during all calls and reminders. “We don’t feel confident in an ongoing supply to offer masks to patients routinely,” Dr. Vander explains. “The priority is to get the health-care workers the masks first. I certainly don’t want to take masks away from emergency rooms and hospitals that need them.”
Time, Finances and Volume
Besides managing increasing office and OR activity, practices will need to focus on the calendar and their adjusted budgets. “The critical date for us will be two months from the date of our Paycheck Protection loan,” says Dr. Vander.
Dr. Murray says his practice will carefully manage the cash flow from his practice’s PPP loan. “My tumor practice has high overhead for the OR,” Dr. Murray says. “If my volume went down, I’d be hurt without support. I do high-end specialty imaging, which most retina practices don’t do. If volume should drop too far, that’s when I think most people have to make the difficult decision to let their staffs go. That is, unfortunately, what I still need to tell my employees these days. I tell them that we’re not out of the woods yet.” REVIEW