With the immense popularity of corneal refractive procedures such as LASIK, implanting a phakic intraocular lens has remained pretty far down on most American surgeons' preference list. However, such lenses provide good vision for patients needing high corrections; accommodation is preserved; the procedures are reversible; corneal healing isn't a factor in the outcome; postop dry eye is not an issue; and implantation can be combined with corneal or other procedures. These patients also may require fewer postop visits, compared to laser-surgery patients who have dry eyes or visual complaints.
Phakic IOLs currently fall into three categories based on where they are positioned inside the eye: posterior chamber lenses, which are placed behind the iris (such as STAAR Surgical's Visian ICL); iris supported lenses, which enclavate tissue on the front of the iris to hold the lens in position (such as AMO's Verisyse lens, or its foldable cousin, the Veriflex); and angle-supported lenses, which are placed in the anterior chamber between the iris and the cornea (such as Alcon's AcrySof Phakic, currently in clinical trials).
Here, surgeons from several countries discuss the advantages of each design. (Note: Verisyse and Veriflex lenses are distributed in
Posterior Chamber or Iris Claw?
Erik L. Mertens, MD, FEBOphth, ophthalmic surgeon and medical director of the
"In my hands, the Visian has extremely high predictability and practically no side effects," he says. "It also has a more aesthetic appearance in the eye than the iris claw lenses that sit in the anterior chamber. I've never had any problem with zonules as a result of using it—and I've never had an infection after implanting any phakic lens. However, I'm very careful about selecting my patients. The only problem I've encountered is a refractive surprise in less than 1 percent of my ICL patients. In those cases, if there's an absolute contraindication for laser surgery I exchange the lens. Otherwise, I use laser correction."
Dr. Mertens says his success with the ICL has led him to use the Artisan lens much less often. "The Artisan requires a 6-mm incision, which needs stitching," he notes. "That induces astigmatism even if you're a very good surgeon. The foldable Artiflex isn't my favorite lens either, because it's made of silicone, and in 15 to 20 percent of cases it causes inflammation in the anterior chamber. The angle between the haptics and the optic is not as pronounced as it is with the nonfolding Artisan, so if you enclavate too much iris tissue into the claws it can rub against the optic-haptic junction, causing inflammation. This means giving the patient steroids for a longer time."
Simon P. Holland, MD, clinical professor of ophthalmology at the
Dr. Holland says he likes the ICL for several reasons, including the availability of a toric lens. "Many good candidates, such as high myopes, have a degree of astigmatism that can be addressed effectively with a toric Visian," he says. "But even without that, the lens has worked well.
"One problem we're concerned about is cataract development over the long term because the ICL is positioned so close to the crystalline lens," he notes. "However, most cataracts that have been reported were related to surgical technique, such as touching the lens during implantation. Another concern is that I need to do fairly large iridectomies when I implant this lens—and I've had one or two patients develop pupil block in spite of that. This is largely a question of surgical technique, however. Overall, I think it's an excellent lens."
Dr. Mertens says there are some situations in which he would not use the Visian ICL. "It's not good to put in an ICL when the patient is 50 years of age or older," he notes. "Those patients have a much higher incidence of cataract formation; it may be that an older crystalline lens is more compromised by the inflammatory response you trigger when you open the eye. Also, if the anterior chamber is shallower than 2.8 mm from endothelium to crystalline lens, I won't implant an ICL. Only about 20 percent of our hyperopes have a sufficiently deep anterior chamber."
David R. Hardten, MD, director of refractive surgery for Minnesota Eye Consultants and
Unlike Dr. Mertens, Dr. Hardten says he tends to choose the Visian implant in a patient of presbyopic age who is not ready for lens replacement. "There are a number of reasons for this," he explains. "First, if the patient is 25 and the lens will be in the eye for a long time, it makes sense to do a little extra work to make the larger incision and implant the Verisyse in order to have a lower risk of cataract. If a patient of presbyopic age develops a cataract, it's not as big an issue; almost everybody eventually needs cataract surgery when they get older. Second, the shorter recovery time with the Visian is better for an older patient; a younger patient can handle a slightly longer recovery time. Third, the smaller incision in the older patient pays off if you have to remove a cataract a few years later; you won't have to make a large incision to remove the IOL."
Using Angle-Supported Lenses
Jorge L. Alio, MD, PhD, professor and chairman of ophthalmology at
"My first choice is to use angle-supported lenses," says Dr. Alio. "These lenses have had problems in the past, but after 18 years I still favor them. I implanted a phakic angle-supported IOL in my own sister, who was -23 D, 18 years ago. She is still doing fine, with a normal endothelial cell count, excellent quality of vision and no complaints—which is true for most of our implanted patients. Some of the earlier angle-supported lens models were not successful because of their designs and materials. However, I have been lucky—or perhaps had the medical wisdom to choose the right ones—because I haven't had any trouble with them."
Dr. Alio offers four reasons for his current preference for angle-supported lenses. "First, there is a wider area inside the anterior chamber to implant the lens," he says. "Second, during implantation you see everything you're working with right in front of you. Third, the current models appear to be even more reliable than previous models I've used. Fourth, the examination and measurement technology we have at this moment is more accurate for the anterior chamber than for the posterior chamber."
Dr. Alio does use other lenses, however. "I use the Visian ICL when I want to simultaneously correct myopia and astigmatism, in cases where the astigmatism is more than 1.5 D," he says. "In cases of mixed astigmatism, hyperopia or hyperopic astigmatism, I use an iris-claw lens." Dr. Alio says that offering all three options allows him to cover every type of eye for which a phakic IOL is appropriate.
"Currently, I prefer the toric ICL for myopic astigmatism, simply because of the small incision," he continues. "I use the Artisan for hyperopic astigmatism, mixed astigmatism or hyperopia. The Artiflex is a very good lens for straightforward myopia; I don't use it more frequently because angle supported lenses are easier to implant. I reserve it for cases in which the anatomy is not what I consider optimal for an angle-supported lens."
Angle-Supported Lens Concerns
"The big advantage of the Acrysof phakic [compared to posterior-chamber lenses] is that it's easier to insert and remove, and farther away from the crystalline lens," says Dr. Holland. "And it has fewer issues relating to acute glaucoma or pupil block than previous angle-supported lenses. The question the current trials should answer is: What effect will it have on the endothelium? This is the big concern with any angle-supported lens."
Dr. Holland notes that angle-supported phakic IOLs have been associated with several problems in the past. "One issue is the possibility of causing synechiae—connections between the iris and the endothelium in the periphery," he says. "That can be a problem because it's associated with endothelial cell loss and possibly inflammation of the angle; it can lead to glaucoma in the long run. Some of the earlier angle-supported lenses used fixed-loop haptics made from rigid materials that got encased in the periphery, leading to these problems.
"The data from our five AcrySof investigators shows an initial endothelial cell loss of about 2.2 percent in the first six months, and 3 percent in the first year," he continues. "But after the first year the endothelial cell loss has been the same as you find with the normal aging of the eye. The caveat is that most of the other anterior chamber lens implants didn't show a problem until three to five years post-surgery; I think that's the reason this trial has been extended. But some of the previous lenses that were withdrawn had cell losses of 10 percent the first year, plus significant ongoing losses."
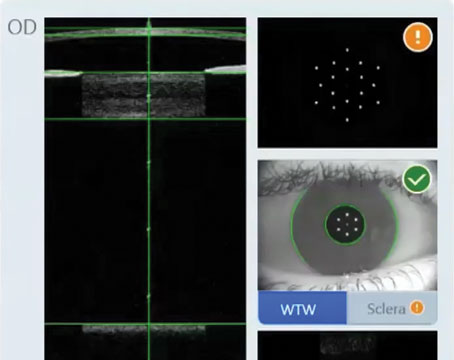
Dr. Holland notes that another concern has been ovalization of the pupil caused by the pressure of the haptics pushing out into the angle. "In the AcrySof trials, out of more than 700 eyes implanted with the lens, there have been no cases of pupil ovalization," he says. "That's unusual with such a large cohort. It may be because the haptic loops on this lens are flexible; if tissue is pressing against the loop, the loop flattens a little into an oval shape. This makes precise sizing less of an issue than it is with posterior chamber phakics; we just use white-to-white, which is inaccurate, but we haven't had any issues as a result."
There is a potential downside to this advantage, however. "Because the lens is forgiving, we're concerned that if patients rub their eyes, the lens could rotate," explains Dr. Holland. "A number of patients have presented with lens rotation, although so far it hasn't been associated with any clinical problems. Obviously, if Alcon wants to put a toric platform on this, they'll have to find a way to stop the lens from rotating."
Dr. Holland says the surgery itself is not difficult. "You have to make sure the lens isn't inside-out when you implant it," he says. "It's so flexible that it can flip. Other than that, it uses the same inserter as the standard AcrySof, which is familiar technology for most surgeons. And you make the same incision you would for cataract surgery. Generally, I use a temporal approach, although I sometimes move the incision site to act as a partial limbal-relaxing incision."
Clinical Results
Dr. Holland says patients receiving the angle-supported lens have been very happy. "The biggest problem we have is getting patients to come back for follow-up," he notes. "I'm not trying to promote this lens, but patients have been very satisfied. Most phakic lenses in myopic patients will improve best-corrected visual acuity, but we're seeing 20 to 22 percent of our patients gain two or more lines of uncorrected vision. It seems to improve the quality of their vision, too—probably because it's closer to the nodal point of the eye. We've had results like this with hyperopic patients as well."
The clinical results of the AcrySof phakic trial so far have been outstanding, he notes. "My counterparts in the
Dr. Alio notes that there appear to be a few differences between the visual outcomes associated with different phakic IOLs. "For example, night vision problems are more unusual with posterior chamber lenses," he says. However, he suspects that overall vision may be somewhat higher quality with the AcrySof phakic IOL than with the other lenses. (Dr. Alio has no financial connection to the AcrySof lens, although he is a clinical investigator for Alcon.) "I don't have data to prove this, but I believe the vision you get with the Alcon lens is crisper," he says. "I participated in the study of the AcrySof phakic IOL in
Pearls for Implanting Phakics
These strategies should help make phakic IOL implantation go more smoothly:
• When sizing a posterior chamber IOL, don't rely solely on white- to-white. "The white-to-white measurement, recommended by STAAR's software program for the Visian, will give you the best lens size about 90 percent of the time," says Dr. Mertens. "But when the sulcus-to-sulcus size is significantly smaller than the white-to-white, I choose an ICL one size smaller than the one recommended by the software program. If the UBM instrument indicates that the sulcus is larger, I go for a one-size-larger ICL. Since I began using this protocol two years ago, I haven't had any angle-closure glaucoma or cataracts relating to the size of the IOL."
• With the Visian ICL, use HPMC viscoelastic. "When implanting a Visian lens, I'd recommend using only hydroxy propyl methyl cellulose viscoelastic rather than hyaluronic acid-based viscoelastic," says Dr. Mertens. "The latter can remain trapped behind the Visian after surgery because it's difficult to remove; then its chemical composition can cause small opacities in the lens. HPMC-based viscoelastic won't cause this problem."
• Pay attention to endophthalmitis prophylaxis. "Preventing endophthalmitis is of the utmost importance," notes Dr. Mertens. "Put a few drops of povidone-iodine in the eye before the patient enters the operating room, and use it to prepare the skin around the eye. After you put in the speculum, put a few drops of it on the eye again. Be sure to let it work for at least three minutes before you make the incision. At the end of surgery, use vancomycin in the anterior chamber."
• Schedule about twice the time you'd need for cataract surgery. Dr. Hardten recommends this if you're just starting to implant phakic IOLs. "Implanting the Verisyse requires extra preop work—peripheral iridotomies and a peribulbar block, especially for the first few cases," he notes. "Implanting the Visian requires extra postop work—measuring relative position if the lens in the anterior chamber and checking intraocular pressure." He adds that you should use a peribulbar block for your first cases, especially with the Verisyse.
A Growing Trend?
Despite phakic IOLs' slow growth in the
Dr. Mertens also thinks that phakic IOLs will increase in popularity. "Phakic IOLs have been a big success in my practice," he says. "My phakic IOL results are much better than our outcomes from laser surgery, and I have fewer complaints from patients. Plus, being able to say you offer all the options is a marketing advantage."
Dr. Mertens adds that these patients are his happiest. "They never complain," he says. "They have excellent vision and they don't have dry eyes. Every surgeon wants happy patients who don't complain."
Dr. Hardten has financial interests with AMO, Alcon, Allergan, Bausch & Lomb and STAAR Surgical. Dr. Mertens receives travel support from STAAR Surgical. Dr. Alio is a consultant for Bausch & Lomb and a clinical investigator for Alcon.