Presentation
A 56-year-old woman with a macular tumor OS, diagnosed as a choroidal hemangioma with subretinal fluid, was referred to the Wills Eye Hospital Ocular Oncology Service for further evaluation. Her history dated back to an outside institution in 2012, at which time she was found to have a symptomatic macular choroidal hemangioma OS with an overlying retinal detachment. She was offered photodynamic therapy at that time, but she declined and instead elected conservative management with oral propranolol 80 mg twice daily. This therapy continued for two years with mild subjective visual improvement, but treatment was discontinued after her local ophthalmologist retired. She returned in 2018 with worsened visual acuity.
Medical History
Past medical history revealed diet-controlled diabetes mellitus and fibromyalgia. Past ocular history was only significant for myopia. She wasn’t taking any medications. Social history and family history were non-contributory.
Examination
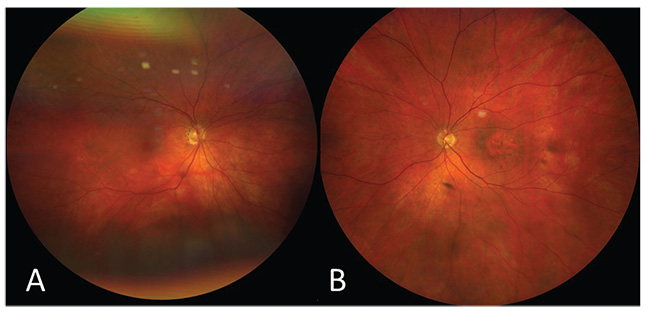
On examination, best-corrected visual acuity was 20/30 OD and 20/150 OS. Pupils, confrontation visual fields and extraocular motility were normal. Intraocular pressures were 17 and 18 mmHg in her right and left eyes, respectively. External examination was within normal limits, and slit lamp examination showed mild nuclear sclerosis bilaterally. Dilated fundus examination OD was unremarkable (Figure 1A). The left fundus revealed macular retinal pigment epithelium atrophy with focal hyperpigmentation and subtle subretinal fluid (Figure 1B).
What is your diagnosis? What further workup would you pursue?
Please click this link for diagnosis, workup, treatment and discussion.