Scientists compared the prediction accuracy of the Barrett True-K for keratoconus with standard formulas (SRK/T, Barrett Universal II and Kane) and the Kane keratoconus formula.
The multicenter retrospective case series took place at the Shaare Zedek Medical Center, Jerusalem, Israel; and University Eye Clinic, Maastricht, the Netherlands.
Eyes with stable keratoconus undergoing cataract surgery were included. Predicted refractions were calculated for SRK/T, Barrett Universal II, Barrett True-K for keratoconus (predicted and measured), Kane and Kane adjusted for keratoconus formulas. Primary outcomes were prediction error (PE), absolute error (AE), and percentage of eyes with PE ±0.25 D, ±0.50 D and ±1 D. Subgroup analyses were performed based on the severity of the keratoconus.
Fifty-seven eyes were included in the study. Here are some of the findings:
- PE wasn’t significantly different from zero for SRK/T, Barrett True-K (predicted and measured) and Kane keratoconus formulas (range: 0.09 to 0.22 D; p>0.05).
- The AE of Barrett True-K predicted (median: 0.14 D) and Barrett True-K measured (median: 0.10 D) were significantly lower than the Barrett Universal II (median: 0.47 D) and Kane (median: 0.50 D); p<0.001.
Scientists concluded that the Barrett True-K formulas for keratoconus had higher prediction accuracy than new-generation formulas and a prediction accuracy similar to the Kane keratoconus formula.
J Cataract Refract Surg 2022; Oct 28. [Epub ahead of print].
Vandevenne M, Webers V, Segers M, et al.
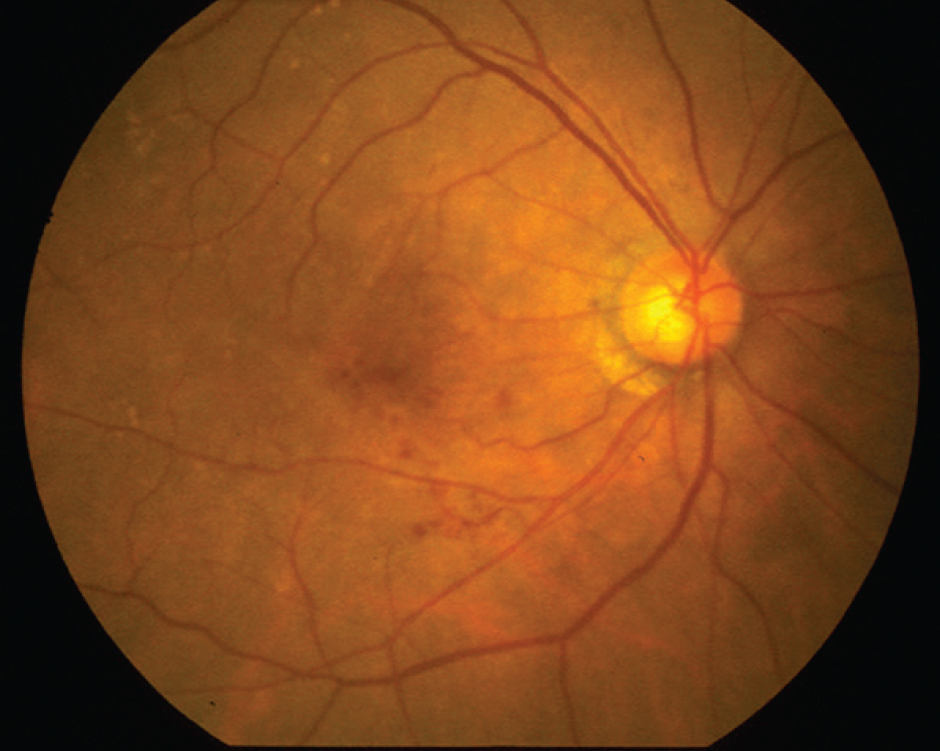 |
Prevalence of AMD in the U.S.
Researchers aimed to produce estimates of early- and late-stage age-related macular degeneration prevalence overall and by age, gender, race and ethnicity, county and state.
The study team conducted a Bayesian meta-regression analysis of relevant data sources containing information on the prevalence of AMD among different population groups in the United States.
Researchers included data from the American Community Survey (2019), the National Health and Nutrition Examination Survey (2005 to 2008), U.S. Centers for Medicare & Medicaid Services claims for fee-for-service beneficiaries (2018) and population-based studies (2004 to 2016). They included all relevant data from the U.S. Centers for Disease Control and Prevention’s Vision and Eye Health Surveillance System.
Researchers estimated the prevalence of early-stage (defined as retinal pigment epithelium abnormalities or the presence of drusen 125 or more microns in diameter in either eye) and late-stage AMD (defined as choroidal neovascularization and/or geographic atrophy in either eye) and stratified it, when possible, by the factors listed earlier. Data analysis occurred from June 2021 to April 2022.
Here are some of the findings:
- In 2019, approximately 18.34 million people ages 40 years and older (95 percent uncertainty interval [UI], 15.30 to 22.03) living with early-stage AMD, corresponding to a crude prevalence rate of 11.64 percent (UI, 9.71 to 13.98).
- Approximately 1.49 million people 40 years and older (UI, 0.97 to 2.15) living with late-stage AMD, corresponding to a crude prevalence rate of 0.94 percent (UI, 0.62 to 1.36).
- Prevalence rates of early- and late-stage AMD varied by demographic characteristics and geography.
Researchers estimated a higher prevalence of early-stage AMD and a similar prevalence of late-stage AMD compared with earlier studies. They suggested that state-level and county-level AMD estimates may help guide public health practice.
JAMA Ophthalmol 2022. Nov 3. [Epub ahead of print].
Rein DB, Wittenborn JS, Burke-Conte Z.
Microvascular Abnormalities and OAG
Researchers evaluated peripheral microvascular abnormalities associated with open angle glaucoma patients, as part of a cross-sectional study.
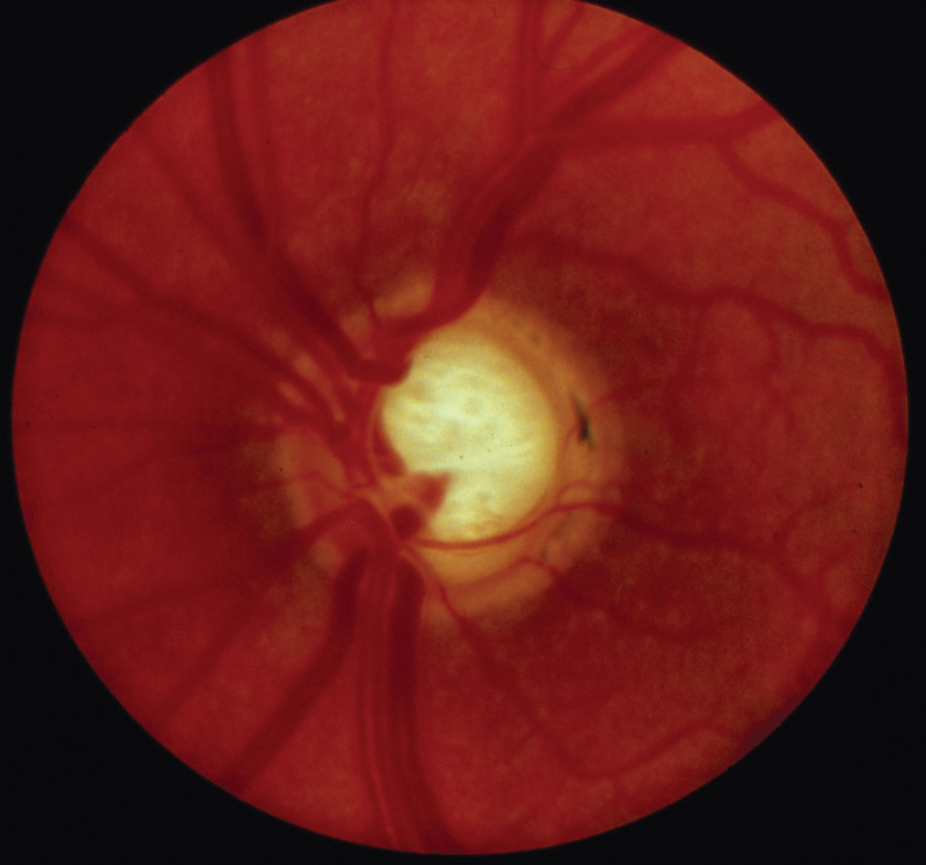 |
Patients with OAG and controls underwent a detailed ophthalmic evaluation, including Humphrey visual field tests and swept-source optical coherence tomography. Researchers performed nailfold capillaroscopy (NFC) and laser Doppler imaging (LDI) to evaluate peripheral microvascular abnormalities. Using NFC, they recorded the presence of microhemorrhages, tortuous capillaries, dilated capillaries, avascular areas and the capillary density, among other characteristics. Fingertip blood flow (FBF) was measured using LDI at different time points, before and one, 10 and 20 minutes after exposure to a cold stimulus. In addition, venous blood samples were collected to measure serum endothelin-1 (ET-1) concentrations as well as serum auto-antibodies.
Main outcome measures included presence of microhemorrhages, tortuous capillaries and dilated capillaries; FBF, ET-1 and auto-antibodies.
Here are some of the findings:
- Sixty-eight subjects (43 patients with OAG and 25 controls) were enrolled.
- Microhemorrhages were found in the nail bed of 65.1 percent of OAG patients compared to 25 percent of the controls (p=0.003).
- A significant difference was found in the mean FBF at baseline in OAG patients (293.6 ±100.2 perfusion units) vs. controls (388.8 ±52 perfusion units) (p<0.001), together with a significant decrease in the mean FBF 10 and 20 minutes after cold stimulus in OAG patients in comparison to controls (p<0.001 for all comparisons).
- A positive correlation was found between mean baseline FBF and HVF MD (r=0.27, p=0.03), and between mean baseline FBF and average retina nerve fiber layer thickness (r=0.44, p=0.001).
- Neither the analysis of ET-1 concentrations (p>0.71) nor the auto-antibodies measurements (p>0.05, for all) showed any difference between the two groups.
Researchers reported significant peripheral microvascular abnormalities were found in open-angle glaucoma patients compared to controls, suggesting that microvascular changes might play a role in the pathogenesis of the disease. In addition, they wrote, some of the abnormalities seemed to correlate with functional and structural glaucomatous damage.
Ophthalmol Glaucoma 2022. Oct 25. [Epub ahead of print].
Taniguchi EV, Almeida INF, Gracitelli CBP, et al.
A.I. and Diabetic Retinopathy
This study investigated the feasibility of using deep learning (DL) models to automatically segment retinal capillary non-perfusion and neovascularization on ultra-widefield fluorescein angiography images from patients with diabetic retinopathy.
This retrospective, cross-sectional chart review study included 951 UWFA images collected from patients with severe nonproliferative DR or proliferative DR. Each image was segmented and labeled for NP, NV, disc, background and outside areas. Using the labeled images, DL models were trained and validated (80 percent) using convolutional neural networks (CNNs) for automated segmentation and tested (20 percent) on test sets. The accuracy of each model and each label was assessed.
Here are some of the findings:
- The best accuracy from CNN models for each label was:
— 0.8208 for NP;
— 0.8338 for NV;
— 0.9801 for disc;
— 0.9253 for background; and
— 0.9766 for outside areas.
- The best intersection over union for each label was:
— 0.6806 for NP;
— 0.5675 for NV;
— 0.7107 for disc;
— 0.8551 for background; and
— 0.924 for outside areas.
- The mean boundary F1 score (BF score) was:
— 0.6702 for NP;
— 0.8742 for NV;
— 0.9092 for disc;
— 0.8103 for background; and
— 0.9006 for outside areas.
Researchers determined that DL models could detect neovascularization and non-perfusion as well as disc and outer margins on UWFA with good performance. They added that automated segmentation of important UWFA features will aid physicians in DR clinics and in overcoming grader subjectivity.
Br J Ophthalmol 2022. Oct 14. [Epub ahead of print].
Lee PK, Ra H, Baek J.
Hypertensive Drugs and Cataract
Researchers say that hypertension medications don’t increase the risk of lens opacity.
A recent study looking into the association between antihypertensive use clinically and cataract risk found that this class of drugs wasn’t associated with an increased prevalence of this ocular occurrence. Previous research was inconsistent on the matter.
The case-controlled study evaluated the Korean National Health Insurance Service-Health Screening Cohort database from a time period spanning 2002 to 2013. Cases were defined as patients prescribed antihypertensives who underwent cataract surgery between 2010 and 2013. Controls were patients prescribed antihypertensives with no history of cataract diagnosis or surgery between 2002 and 2013. Four controls were matched to each case, and adjusted odds ratios and 95% confidence intervals were estimated for cataract risk using a conditional logistic regression model after adjustment.
The analysis included 12,166 cases and 48,664 controls. The adjusted ORs for cataract were 1.18 with thiazide diuretics, 1.12 with beta-blockers, 0.94 with calcium channel blockers, 1.22 with angiotensin-converting enzyme inhibitors and 0.97 with angiotensin II receptor blockers compared with non-use of each antihypertensive.
The researchers say that given the benefits of treating hypertension, such as the reduction in further complications, they suggest it’s not necessary to change current clinical practice for antihypertensives. They add that, however, in a few sections of drug exposure, the risk of cataract increases with the duration of the use of some antihypertensives, clinicians should take into account that hypertension itself may increase the risk of cataracts rather than the use of antihypertensive drugs.
Ophthalmic Epidemiol 2022. Nov 11. [Epub ahead of print].
Yang HL, Byun SJ, Park S, et al.
Post Hoc Analysis of VISTA And VIVID Studies
In a post hoc analysis of the Regeneron-sponsored VISTA and VIVID studies of aflibercept (Eylea), investigators characterized diabetic macular edema incidence in the fellow eyes of patients treated for DME in the study eye.
The analysis evaluated the data on fellow eyes without diabetic macular edema at baseline through week 100. The presence of diabetic macular edema in the fellow eye was inferred by investigator-reported DME adverse events and use of interventions to treat the diabetic macular edema.
Here are some of the findings:
- Over 100 weeks, the following groups of fellow eyes developed DME:
— intravitreal aflibercept injection (IAI) 2 mg q4 weeks (n=245): 44.9 percent;
— IAI 2 mg q8 weeks (n=258): 44.2 percent; and
— laser control (n=252): 42.9 percent.
- Mean time to DME development in combined treatment groups was about six months.
- Multivariable regression analysis confirmed patients with shorter diabetes duration (HR per 10-year decrease: 1.16; 95 percent CI, 1.03 to 1.30; p=0.0160) and thicker baseline study eye central subfield thickness HR per 10-µm increase, 1.01; CI, 1.01 to 1.02; p=0.0002) were at higher risk of developing DME in the fellow eye.
Investigators found, among patients with diabetic macular edema in one eye at baseline, almost half developed DME in the fellow eye over two years. They added shorter duration of diabetes and thicker central subfield thickness in the study eye were predictors of diabetic macular edema development in the fellow eye.
Retina 2022. Oct 17. [Epub ahead of print].
Dhoot DS, Moini H, Reed K, et al.



