Everyone’s probably heard the phrase “work smarter, not harder” at least once in their lives. While the basic principles of phaco haven’t changed, the technology used for it has advanced over the years, providing surgeons with various options to efficiently improve their operations and work smarter. Here, cataract surgeons provide insight into the latest technology advancements and how they use them to achieve greater efficiency in their cataract procedures.
Machine Settings: Best Practices
There are many different brands and models of phaco machines on the market, but they all come with the same basic settings: power; vacuum; and aspiration flow rate. Normally, a representative from the phaco machine manufacturer will visit a physician’s office or operating room to program the machine settings. But, in most cases, the settings can be easily altered pre-, intra- and/or postoperatively.
“For each step of the procedure, you’d dial in different parameters,” says Kevin Miller, MD, the Kolokotrones Chair in Ophthalmology at UCLA. Dr. Miller received his undergraduate degree in bioengineering from John Hopkins University and consults for many companies in the phaco industry. Because of his technical background, Dr. Miller finds himself modifying his machine settings regularly. “I’m one of those people that likes to tweak things. If I’m struggling at some point in the procedure, then I’ll make little tweaks. As I finish the case, and if I like those tweaks, then I’ll save them so that they’re permanent.”
Dr. Miller understands that the factory settings on phaco machines are standardized for cataract surgery, which leads to many surgeons losing efficiency during operation. He says, “I do know that the vast majority of surgeons, once the phaco specialist comes in and sets up the machine and after the surgeon goes through their first five cases, they will never touch the settings. They’ll come back 10 years later, and it’ll have the same settings.”
To increase efficiency during cataract surgery, Dr. Miller suggests more vacuum, more phaco power and more aspiration flow rate. “That allows you to blast through the cataract, get it out of the eye and rip it out really fast,” he says. “But those very same settings that allow you to go faster actually reduce the safety of the procedure. All it takes is for one bad capsule and you could just throw away any efficiency gains that you had gotten for that day.”
 |
| Veritas’ settings are toggled via the touchscreen. Twenty setup options can be programmed onto the machine. The default settings, “Advanced Fluidics Program” and “Advanced Infusion Program,” are available on the touchscreen as well. (Courtesy Johnson & Johnson Vision) |
If increasing settings reduces safety, then what’s a good practice to adjust settings without jeopardizing a patient’s safety? Aaron Waite, MD, from Waite Vision in Utah, sets his phaco machine, Oertli’s CataRhex 3, to toggle between different settings using the foot pedal. “When you do something as precise as eye surgery you want to make sure your settings are set for all comers,” he says. “Set the settings for the densest lens you’re going to encounter, and then you have the modification of the power to use only when you want. So, if a patient comes in and they have a super dense lens, I’m all ready to go. If they’ve got a soft lens, piece of cake.
“Anytime you’re around a new machine, you have to realize you’re going to have to optimize the settings for you as a surgeon,” Dr. Waite continues. “For example, I’ve used a couple of really good machines that I wasn’t happy with because the settings weren’t optimized, but I know if I had the time to sit down and play with the machine, then I’d probably be completely satisfied with those machines.”
Dr. Miller explains why he believes surgeons are hesitant to touch the machine settings. “[A phaco machine is] a versatile tool with a lot of settings that you can adjust, but most people are afraid to touch them because [they’re afraid to break the device],” he says. “It’s like an 80-year-old who gets an iPhone who doesn’t want to break the phone by pressing on the icons. You can’t break it. You push on it and things pop up, you press on other things and more stuff pops up. You play with it and then eventually you figure out how the phone works. Same thing with a phaco machine. So, there are all these little things you can tweak to make it more comfortable for the patient, optimize your efficiency, and also balance it out with safety. But, it means overcoming the fear of breaking the machine by touching it and getting below the settings. And most of the companies—I would say all the companies—have phaco specialists who would be happy to come back and help you optimize your settings based on how they see the cases that you’re doing.”
Some surgeons find the default settings to be comfortable and familiar to their practice. Vestavia, Alabama’s Jack Parker, MD, believes adjusting the settings can cause issues cognitively when using the machine. “Usually, I don’t do very much adjustment intraoperatively,” he says. “The reason is that once you start fiddling around with things a little bit, you sort of just lose your sense of predictability about what’s happening and then you become a little less familiar of what’s going on at what speed. So, typically I’m more comfortable just leaving everything alone during the case.”
Dr. Miller says that, though the phaco settings are important, they’re not the end-all be-all when it comes to total efficiency. “The 30,000-foot-view issue is that for most surgeons, the nucleus removal only takes about a minute, so it’s pretty quick no matter how you do it,” he says. “No matter how unsophisticated you are, or how geeky you are, you’re talking about a minute, plus or minus a little bit, for most people to get through the nucleus removal. So, if you’re really trying to eke out efficiency, how much additional time can you shave off of that minute, and do those few seconds really make a difference in terms of the number of cases you’re going to do on a given day? Probably not. I would say most efficiency gains in surgery will have nothing to do with phaco settings. Even though we obsess about it, and there are things you can do to get through the phaco part faster, in the grand scheme of things, they probably don’t amount to a hill of beans.”
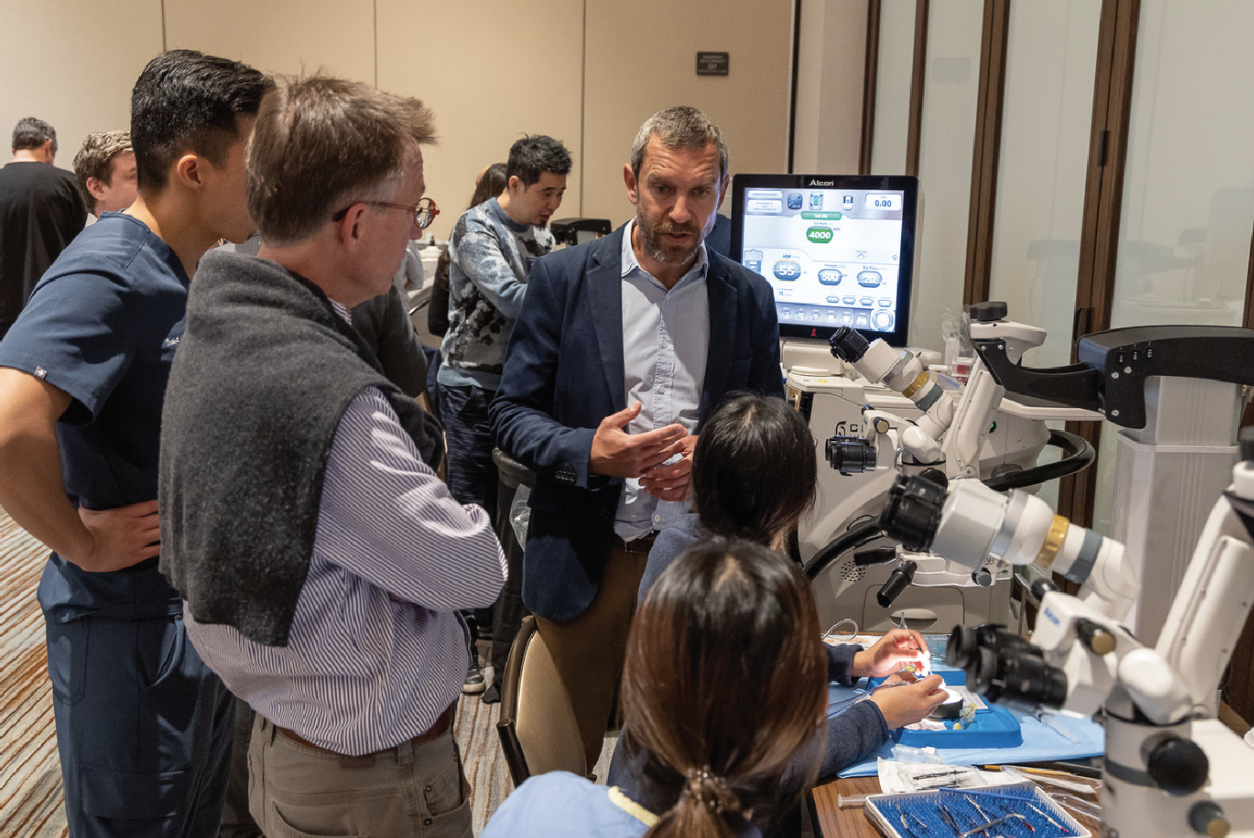 |
| In April, during an Alcon Advanced Cataract Surgery Course in Irvine, Calif., surgical residents learned about the technology for the Centurion system. Residents could test the settings and functions of the machine. (Courtesy Kevin Miller, MD) |
Longitudinal, Torsional and Transversal
Years ago, phaco companies altered the movement of the phaco probe in an effort to gain more efficiency and safety. Most phaco machines use longitudinal ultrasound to breakdown the nucleus in the lens. Other platforms like Alcon’s Centurion and Johnson & Johnson Vision’s Veritas use different forms of ultrasound to reduce thermal energy during surgery. Here’s a review of these alterations and what they bring to the table.
Transversal ultrasound, found in the Veritas system, minimizes chatter from the nuclear fragments that are being emulsified. This type of modulation results in the ability of a “side-to-side” movement that may reduce the frictional heat commonly generated by longitudinal movement, according to the company.1 Alcon says the torsional oscillation effect found in the Centurion system reduces the amount of energy and increases the efficiency required to remove the nucleus by fragmenting the cataract via shearing, in place of the conventional jackhammer effect from longitudinal ultrasound.1
“There’s an efficiency advantage of having pure torsional over pure longitudinal,” says Dr. Miller. “In pure longitudinal, the phaco needle basically pistons forward and backward at about 40 kHz. The tip, virtually at full throttle, pistons at about 3.5 mL/min at 40 kHz. With torsional, it’s different. For the exact same amount of energy applied into the eye, there’s twice as much cutting. So, that’s obviously more efficient.” Although the frequency of torsional phaco is lower than longitudinal phaco at 32 kHz to 40 kHz, at least one study found that the reduction of the repulsive effect and cutting in the lateral direction by torsional phaco make it efficient.2
J&J’s Veritas doesn’t use pure transversal ultrasound, but rather a combination of longitudinal and transversal movements.3 In a 2023 study, researchers compared the grooving efficiency between longitudinal and transversal ultrasound handpieces. They didn’t observe a significant difference in grooving time between the two phaco probes. Transversal ultrasound had a statistically significant decrease in time as the power settings were increased from 25 to 75 percent (5.22 ±0.758 and 4.63 ±0.69 seconds).4 However, researchers speculated that transversal can be more efficient than longitudinal phaco due to increased chatter from longitudinal movements.4
Phaco Machines
No two phaco machines are exactly the same, and various models provide features that can increase efficiency when performing phacoemulsification.
• Bausch + Lomb Stellaris Elite. Bausch + Lomb’s Stellaris Elite Microsurgical System offers both cataract and retina capability in a single platform. The machine features B+L’s Adaptive Fluidics with dynamic infusion compensation, which the company says monitors and compensates fluid flow in the eye. B+L says that efficiency gains in fluidics stem from the rotary vane pump that features a low start-up torque and high-flow capability. Furthermore, instead of traditional longitudinal, the Stellaris uses “Attune” energy. B+L says that this form of energy uses longitudinal ultrasound but combines it with acoustic cavitation technology. Acoustic cavitation is the growth and collapse of preexisting microbubbles under the influence of an ultrasonic field in liquids.8
 |
| Surgical residents in Southern California test the settings of Bausch + Lomb’s Stellaris Elite. These are not recommended settings, but rather an example of the settings and features presented on the machine. (Courtesy Kevin Miller, MD) |
The Stellaris uses a touchscreen display to control machine parameters. Here, surgeons can access phaco power, aspiration flow rate, vacuum and more. Phacoemulsification frequency runs at up to 28.5 kHz with a pulse mode range of 1 to 250 pulses per second. Irrigation can be manipulated using either gravity, pressurized air or both. Air pressure maxes out at 100 mmHg and the vacuum can fluctuate between 0 and 600 mmHg.
The Stellaris is equipped with vitreous removal. B+L’s Bi-Blade vitrectomy cutter is a dual-edge blade that effectively cuts at 15,000 CPM. Another retina feature specific for the Stellaris is the Vitesse hypersonic vitrectomy system. This system produces high-frequency longitudinal vibrations that aim to liquify vitreous, as opposed to a traditional guillotine vitrectomy system that cuts vitreous at a high rate.9
• Alcon Centurion. The Centurion Vision System is similar to the Alcon Infiniti Vision System. The Centurion is equipped with torsional phaco, and features the “Active Sentry” handpiece. According to Alcon’s website, this handpiece has a built-in pressure sensor that regulates IOP and chamber stability.
“With the Centurion, I have a sculpt that’s on continuous, a chop which is on burst, and a quad which is on pulse,” says Dr. Waite. “The other thing is that it has torsional and longitudinal phaco. So, the phaco tip has sort of a bend to it so if you twist it, [it phacoemulsifies the cataract], where if you have a straight tip and twist it, it does nothing. So, the torsional phaco can only work with a certain type of phaco tip, but the Alcon machine uses what the company calls ‘intelligent phaco,’ which is predominately torsional, but then it kicks into longitudinal once you have occlusion.”
The Centurion begins to become more efficient when torsional power reaches 60 percent.5 This occurs when the machine’s vacuum is set at 550 mmHg, aspiration at 50ml/min, and IOP at 50 mmHg.5 During a 2016 study, researchers found no efficiency gains after increasing the torsional power above 60 percent. They reported that chatter was highest at 10-percent power and decreased linearly as power was increased up to 60 percent, and chatter didn’t improve above this power level.5
• Johnson & Johnson Vision Veritas. The Veritas features a dual pump fluidics system, which J&J says increases phaco efficiency by allowing surgeons the ability to switch between peristaltic and Venturi pumps and adapt to clinical needs.
In order to optimize the Veritas system for surgery, researchers determined the most efficient settings for both available pump types. During an in vitro laboratory study, researchers hardened porcine lens nuclei with formalin to simulate a human cataract lens.6 Using a Venturi pump, researchers concluded that the phaco system became most efficient when the bottle height was set at 100 cm, the vacuum was set to 600 mmHg, and the power was set to 80 percent.6 Aspiration flow rate wasn’t measured during the study.
In a separate study using porcine lens nuclei, researchers determined the most efficient settings with a peristaltic pump attached to the Veritas. They concluded that setting the bottle height at 100 cm, vacuum at 600 mmHg, aspiration rate of 50 or 60 mL/min, and power at 90 percent provided the most efficient parameters.7
 |
| Oertli offers optional accessories such as a carrying case, a sterile touching device and an infusion pole to make the CataRhex 3 simpler to transport, set up and operate in most clinics. (Courtesy Oertli) |
• Oertli CataRhex 3. “There isn’t a traditional software operating system on the CataRhex. It’s a direct push of a button to function, like a handheld calculator. This means there are no software glitches, problems, or updates, and due to this approach, the CataRhex is remarkably low maintenance,” says Dr. Waite. Oertli describes its phaco machine, the CataRhex 3, as compact and portable. The device itself weighs 11 lbs., and all connections and features can be accessed on the front of the device. Also, the CataRhex is equipped with Oertli’s Speep pump, which is a peristaltic-Venturi pump hybrid. The pump allows for surgeons to independently control both the flow and vacuum.
The CataRhex 3 allows surgeons to toggle between what it calls Phaco 1, 2 and 3. Dr. Waite worked closely with an Oertli representative to choose specific parameters that fit his needs for each phaco settings. “What I use for my Phaco 1, we’re going to call that one ‘sculpt,’ is continuous phaco at 60 percent, flow at 18mL/min and the vacuum set to 100 mmHg. Phaco 2, which is ‘chop,’ is in a burst mode. The burst’s power is at 70 percent, the flow is at 40mL/min and the vacuum is at 475 mmHg. Phaco 3 is the ‘quad’ setting. That’s in a pulse mode. Pulse is at 55 percent, flow is at 40 mL/min and the vacuum is at 565 mmHg,” he says.
Dr. Parker is also a CataRhex 3 user. “We use a low vacuum usually between 60 and 100 mmHg and a higher phaco power: about 80 percent. Flow is usually about 10 mL/min,” he says. “The settings that I quoted aren’t particularly aggressive; they’re the default settings recommended by the company.”
• DORC EVA System. Dutch Ophthalmic Research Center offers the EVA Nexus, an ophthalmic surgical system, with the upgraded phaco-vitrectomy system. The integrated footswitch comes with six programmable buttons that allow surgeons the ability to switch between phaco and vitrectomy surgeries. The company offers customizable inlays to allow for alternative foot positions and comfort. Surgeons can control the device’s vacuum and flow using Vacuflow VTi technology. This eliminates the risk of unwanted pulses or flow. The vacuum runs between 0 to 680 mmHg and the flow runs between 0 to 90 mL/min.
The EVA platform is meant for both phacoemulsification and vitrectomy. The vitrectomy handpiece cuts at a max speed of 16,000 CPM, but surgeons can opt for a different device. DORC’s TDC cutter has a cut speed of up to 8,000 CPM and is designed to facilitate cutting tissue on the return of each stroke of the vitrectome. For phacoemulsification, phaco pulse mode runs at a maximum 250 PPS at 40 kHz. In the EVA EquipPhaco platform, DORC provides disposable and reusable phaco tips in four sizes: 1.8 mm; 2.2 mm; 2.4 mm; and 2.8 mm.
• Zeiss Quatera 700. The latest phacoemulsification machine from Zeiss features a brand-new pump system to streamline cataract surgery. According to the company, the Quattro pump is a synchronized fluid exchange system that directly measures and simultaneously controls both infusion and aspiration volumes in real-time.
“This new Quattro pump allows the surgeon to use higher levels of vacuum without sacrificing chamber stability or safety of surgery,” says Ralph Chu, MD, ophthalmologist at Chu Vision Institute in Minnesota. “The higher levels of vacuum are what allows more efficient removal of the cataract. It’s not only the cataract, but also the cortical material. With all these premium lens technologies, having cortical cleanup is critical.”
Having a complete Zeiss suite allows for more efficient phacoemulsification when using the Quatera 700. “When you have all the Zeiss products aligned with it it’s more efficient,” says Dr. Chu. “What I’m talking about is digital workflow – having Zeiss’ diagnostic equipment, the Callisto intraoperative alignment system, as well as the forum can help surgeons.” The Callisto eye system from Zeiss eliminates manual markings for aligning toric IOLs by using a digital interface to examine the eye and precisely measure for markerless alignment. This can be controlled by the foot pedal or hand grips.
Dr. Chu uses three different settings for phacoemulsification: irrigation and aspiration (I/A); supracapsular; and sculpt. On his machine, irrigation is set to 45 cmH2O and vacuum is controlled between 0 and 600 mmHg for I/A. Irrigation is set to 48 cmH2O, vacuum is controlled between 300 and 600 mmHg, and ultrasound is set between 20 and 65 percent for supracapsular. Lastly, irrigation is set to 50 cmH2O, vacuum is set between 0 and 100 mmHg, ultrasound is set between 10 and 100 percent, and flow is set between 0 and 24 cc/min. This can all be controlled on the Quatera 700 interface or the foot pedal. However, Zeiss offers Power on Demand, which automatically modulates ultrasound without pressing or releasing the foot pedal.
The latest phacoemulsification technology is continuously being advanced through the numerous phaco platforms on the market. “I think the phaco machines of the future will have a little bit of AI, or smart programming, in it to figure out if you’re struggling. It’ll learn how to auto adjust for you so that it happens intuitively. I think things like that will happen down the road,” Dr. Miller speculates. “Things like that smart software that will be running in the background will make novice surgeons look like more experienced surgeons because it’s going to help optimize the technology portion of what they’re doing. But the technology isn’t there, yet. We’re still in the phase where you have to set the things yourself.
Dr. Miller consults for Alcon and Johnson & Johnson Vision. Drs. Waite and Parker have no financial interests in the products discussed. Dr. Chu is a consultant for Carl Zeiss Meditec.
(8/18/23: Article modified to include the Quatera device.)
1. Assil KK, Harris L, Cecka J. Transverse vs torsional ultrasound: Prospective randomized contralaterally controlled study comparing two phacoemulsification-system handpieces. Clin Ophthalmol 2015;9:1405-11.
2. Kim DH, Wee WR, Lee JH, Kim MK. The comparison between torsional and conventional mode phacoemulsification in moderate and hard cataracts. Korean J Ophthalmol 2010;24:6:336-40.
3. Quesada G, Chang DH, Waltz KL, Kao AA, Quesada R, Wang Y, Ji L, Parizadeh D, Atiles L. Clinical performance and surgeon acceptability of a new dual mode phacoemulsification system. Clin Ophthalmol 2022;16:2441-2451.
4. Wilkinson SW, Ungricht EL, West WB, Harris JT, Zaugg B, Olson RJ, Pettey JH. Comparison of phacoemulsification grooving efficiency in longitudinal vs transversal handpieces. Clin Ophthalmology 2023;17:191-195.
5. Jensen JD, Shi DS, Robinson MS, Kramer GD, Zaugg B, Stagg BC, Pettery JH, Barlow WR Jr, Olson RJ. Torsional power study using Centurion phacoemulsification technology. Clin Exp Ophthalmol 2016;44:8:710–713.
6. Wright AJ, Thomson RS, Bohner AD, Bernhisel AA, Zaugg B, Barlow WR, Pettey JH, Olson RJ. Optimization of venturi mode phacoemulsification settings of the Abbott Medical Optics WhiteStar Signature Pro in a porcine lens model. Int J Ophthalmol Clin Res 2017;4:077.
7. Wright DD, Wright AJ, Boulter TD, Bernhisel AA, Stagg BC, Zaugg B, Pettey JH, Ha L, Ta BT, Olsen RJ. Optimization of transversal phacoemulsification settings in peristaltic mode using a new transversal ultrasound machine. JCRS 2017;43:9:P1202-1206.
8. Ashokkumar M. The characterization of acoustic cavitation bubbles - an overview. Ultrasonic Sonochemisty 2011;18:4:P864-872.
9. Stocchino A, Nepita I, Repetto R, Dodero A, Castellano M, Ferrara M, Romano MR. Fluid dynamic assessment of hypersonic and guillotine vitrectomy probes in viscoelastic vitreous substitutes. Trans Vis Sci Tech 2020;9:6:9.