The Rationale for the Measurement
If you use an AMO Tecnis Z9000 or an Alcon SN60WF lens in an attempt to counteract the spherical aberration in the cornea, surgeons say measuring the cornea's spherical aberration preop would be a good idea in order to select the lens that cancels out the most corneal spherical aberration. The measurement strategy may not be as applicable, however, for the Bausch & Lomb SofPort AO since that lens isn't designed to counteract whatever amount of spherical aberration is in the cornea. Instead, the SofPort AO strives to not induce any spherical aberrations on its own, leaving whatever spherical aberration exists in the cornea untouched.
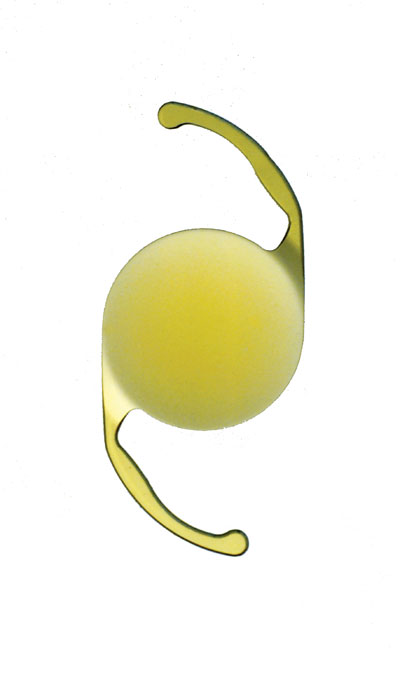
 |
| The AMO Tecnis. |
The Tecnis has -0.27 µm of spherical aberration, while the Alcon has
-0.15 µm. Knowing this, some surgeons say, you could use certain corneal topographers to measure the patient's corneal spherical aberration, then select the lens that best counteracts that number in order to bring the entire visual system's spherical aberration to zero, or as close to zero as possible. According to Houston surgeon Jack Holladay, zero was selected as a target based on studies analyzing the human visual system.1-3
"A number of studies show that, at 19 to 20 years of age, the spherical aberration of the eye is zero, meaning that the cornea and the crystalline lens are a matched system in which the positive spherical aberration of the cornea is just about equal and opposite to that of the crystalline lens," says Dr. Holladay. "The point is that the visual system of the human hits its peak at about 19 years of age. At that age, all visual function is at its best—color, contrast sensitivity and visual acuity."
San Diego surgeon Stephen Schallhorn has done studies analyzing the higher-order aberrations of naval aviators, and made the interesting finding that some aviators with excellent vision had a little spherical aberration. However, he says that, even though it's possible for some aberrations to be compatible with good vision, zero higher-order aberrations is probably the best endpoint for most patients.
"It's possible that having certain combinations of lower and higher-order aberrations could give you better apparent vision," says Dr. Schallhorn. "For instance, obviously you'd want zero astigmatism in a patient to get the best vision. However, consider a patient who can't accommodate and has +0.5 D of sphere. If that patient had -1 D of cylinder, his spherical equivalent would be plano. Therefore, the patient would have better vision with -1 D of cylinder than without it. So, with that analogy, it's possible that some combination of a little spherical aberration with some other aberration might leave a patient with better vision than if he had no spherical aberration. But, in general, I think we ought to be targeting zero spherical aberration."
 |
| Alcon's SN60WF. |
In studies by AMO, by counteracting the cornea's spherical aberration the Tecnis was able to improve patients' contrast sensitivity by 40 percent and improve their reaction time during night driving by 0.5 seconds, allowing them to stop 45 feet sooner at 55 m.p.h. than someone with a non-aspheric IOL.4
Measuring the Cornea
To nail down the amount of spherical aberration contributed by a patient's cornea, Dr. Holladay performs topography and measures the spherical aberration over a 6-mm zone. "Unfortunately, only a few of the existing topographers will do a Zernike transformation from data over a 6-mm zone, and it's critical that the calculations are done over a 6-mm zone, in order to be comparable," he says. The Carl Zeiss Meditec Humphrey Atlas, the Nidek-OPD scan and the Oculus Pentacam can do the measurement. "Many manufacturers will probably have to add it, but they haven't done it yet," Dr. Holladay says, though there is a way everyone can do it now.
Illinois vision and optics researcher Ed Sarver, PhD, has developed a software program called VOL-CT (formerly CTView) that can take topography analysis files and tease out Zernike terms, including spherical aberration. It is available at sarverandassociates.com.
"So, you can export your topography file to Dr. Sarver's program and find out what the patient's spherical aberration is," says Dr. Holladay. "If it comes out to be +0.27 µm, then you know the Tecnis IOL with its -0.27 µm will be perfect. If it's +0.15 µm, then the Alcon lens would be best. And, if it comes out to be zero, as might happen after a hyperopic LASIK, then the Bausch & Lomb lens would be the preferred option."
A traditional wavefront analyzer won't yield the corneal spherical aberration unless it's able to separate corneal aberrations from those of the lens. Most wavefront systems just give the entire eye's spherical aberration value, which isn't what the surgeon needs to plan the aspheric lens implantation.
Dr. Holladay also warns against using an eye's keratometry reading and q-value (an asphericity measurement) to derive the spherical aberration. "This is because the model of an ellipse, which uses the q-value and a central corneal radius, doesn't accurately match the shape of the real cornea," he explains. "So, if you were to take a -0.26 q-value, which is the average in the population, and a K-reading of 44, also the average in the population, you'd come up with +0.18 µm as the cornea's spherical aberration, which doesn't match the true population average of +0.27 µm, underestimating it by 35 percent."
Farrell Tyson, MD, of Cape Coral, Fla., has had success using the OPD Scan to measure corneal spherical aberration before aspheric IOL implantation. "I'm getting very good results, and the patients are pleased," he says. "The ones you really notice the effect in are the post-myopic-refractive-surgery patients. They have the most spherical aberration in their corneas to begin with, and they notice they're not seeing as much starbursting or halos post-implantation."
Naturally, not every patient will fall into the +0.27-µm or +0.15-µm categories. For those who are around these values but not exactly on them, Dr. Holladay recommends leaving the patient with a little negative spherical aberration, rather than positive.
"It's better to err on the minus side of spherical aberration, because the optical system with a little minus spherical aberration will have a little bit stronger power in the center and less in the periphery," he explains. "For example, say you had two identical patients, one with +0.1 µm of spherical aberration and one with -0.1 µm. The halo on the retina will be identical for them, with the same diameter. The difference is, when they look at something up close, the pupil constricts and the patient with negative spherical aberration will have stronger power in the center, allowing him to read a little better. With positive spherical aberration, on the other hand, as the pupil comes down the center gets weaker and the near vision gets worse. Refractive surgeons have known this for years. When comparing hyperopic and myopic LASIK patients that have equal distance vision, the near vision in the hyperopic patient is always better because the hyperopic ablation induces negative spherical aberration, whereas the myopic ablation induces positive."
 |
| B&L's SofPort AO. |
1. Wang L, Santaella RM, Booth M, Koch DD. Higher-order aberrations from the internal optics of the eye. J Cataract Refract Surg 2005;31:8:1512-9.
2. Holzer MP. Data presented at the 19th Congress of German Ophthalmic Surgeons (DOC), Nuremburg.
3. Artal P, Ferro M, Miranda I, Navarro R. Effects of aging in retinal image quality. J Opt Soc Am A 1993;10:7:1656-62.
4. AMO FDA study results granting New Technology IOL Status.




