WITH THE RECENT INTRODUCtion of 25-ga. vitrectomy (25gPPV) systems, vitreoretinal surgeons are working to explore and fully realize all possible benefits that this "minimally invasive" technique may offer in managing patients with surgical posterior segment disease. These 25gPPV techniques may allow us to achieve desired surgical anatomical goals with reduced surgical trauma, less postoperative inflammation, more rapid recovery times, and less patient discomfort. As we gain surgical experience, we continue to add new techniques and push the capabilities of the small incision approach farther.
Until now, a major limitation of the 25gPPV approach has been the inability to place a silicone oil (SO) endotamponade. Placing SO has previously mandated at least one traditional 20-ga. sclerotomy. In this article, I"ll describe my technique for placing SO quickly and effectively using the 25gPPV system, and how it developed.
Ramping Up
My partners at the Cincinnati Eye Institute and I had been dabbling with 25gPPV for several years but began consistently expanding our utilization of this approach in mid-2004 when the 25gPPV system became available for the Alcon Accurus. Initially, we were impressed with the system"s potential but expected to use it for a minority of cases. With increasing experience, improved illumination capabilities, and a continually improving array of available intraocular 25-ga. instrumentation, we found ourselves doing an increasing percentage of surgeries, and more technically challenging surgeries with the 25-ga. system. Patients with epiretinal membrane, macular hole, primary retinal detachment, posteriorly luxed intraocular lens, and even advanced diabetic retinopathy were successfully operated. These eyes did well postoperatively, and anecdotally seemed to recover faster with less discomfort and inflammation. For example, one patient with 20/40 cataract and 20/80 epiretinal membrane underwent combined phacoemulsification with PCIOL placement and 25gPPV with membrane peeling. Visual acuity was 20/40 on postop day one, 20/20 at postop day seven.
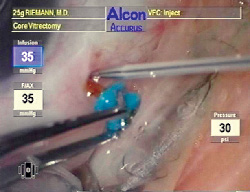
The tip of a 24-ga. Angiocath is slid down the shaft of the 25gPPV trocar until the sclerotomy is engaged.
First Case for SO Placement
In June 2004, I met a patient who had undergone combined scleral buckling and conventional 20-ga. PPV with intraocular gas tamponade two weeks previously to repair a rhegmatogenous retinal detachment. The repair failed and the patient was referred to me with a recurrent, now total, retinal detachment. The eye had not tolerated the previous surgery well at all, with 1+ corneal edema, 2+ anterior chamber cell/flare, extensive posterior inflammatory debris with fibrin strands, early proliferative vitreoretinopathy, and significant choroidal effusions. I felt that this eye would benefit from a minimally invasive 25gPPV and intraocular tamponade of the retina with silicone oil. The challenge was how to get the SO into the eye without enlarging a sclerotomy.
Injecting SO through a 25-ga. needle is unacceptably slow due to the oil"s high viscosity and the narrow internal diameter of the needle (254 µm). Poiseuille"s equation tells us that resistance to fluid flow though a cylindrical pipe is directly proportional to the viscosity of the fluid, directly proportional to the length of the pipe, and inversely proportional to the fourth power of the radius of the pipe. I chose Silikon 1000 (Alcon Labs) over Adato Sil-Ol 5000 (Bausch & Lomb) due to its fivefold lower viscosity.
To maximize the radius of the injection device, I chose a standard 24 ga. intravenous catheter (Angiocath, Becton, Dickinson and Co.). This is readily available in all operating rooms and comes with its own rigid 25-ga. stylette needle which, when removed, leaves an internal diameter of 440 to 520 µm. Due to the fourth-power relationship between radius and resistance to flow, this increased radius (from the 254 µm of the 25-ga. needle) results in a 9.0 to 17.6-fold increase in flow rate.
25gPPV trocars are actually 23.5 ga. in outer diameter to facilitate entrance and egress of 25-ga. instruments. I easily exchanged the 24-ga. Angiocath for one of the vitrectomy trocars, thereby obviating the need for a further sclerotomy. I achieved a 95-percent posterior SO fill in less than a minute by connecting the viscous fluid injector and SO syringe to the Angiocath. The patient did quite well and recovered 20/80 visual acuity.
My success with this patient led me to use this technique to operate on patients with primary retinal detachments and macular holes who were unable to maintain postop positioning with a gas endotamponade. I also used this technique on patients with combined macular staphyloma, vitreomacular traction syndrome and macular hole. All patients have done quite well.
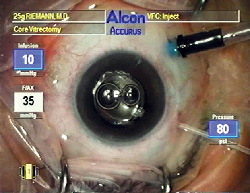
With the Angiocath exchanged for the vitrectomy trocar and connected to the silicone oil syringe, oil is injected at 80 psi.
Technique
The technique for placing SO though a 25gPPV sclerotomy is straightforward. After all intraocular work has been completed and the air/fluid exchange accomplished, the eye is ready to receive SO. Either the superotemporal or superonasal trocar is pulled out halfway so approximately 2 mm of the trocar"s shaft shows. The Angiocath and its stylette are left together as if starting an IV line. Place the bevel of the needle right against the shaft of the trocar, and slide the needle tip down the shaft of the trocar, through the opening in the conjunctiva, until the sclerotomy opening is engaged. The trocar is pulled out and the stylette and Angiocath are simultaneously pushed in so as to exchange the trocar for the Angiocath. The stylette and Angiocath are then carefully advanced into the anterior vitreous cavity until they are visualized through the pupil. The stylette is then removed and the Angiocath connected to the oil syringe, which is filled with Silikon 1000. The SO is then injected through the Angiocath using the viscous fluid injector and an injection pressure of 80 psi until the desired fill is achieved. The Angiocath and remaining trocars are then removed and routine postop meds administered.
Pearls
Use the shortest 24-ga. Angiocath available to minimize resistance to oil flow (which is directly proportional to the length of the catheter). The catheter may be trimmed on an angle to 5-6mm, which significantly speeds SO injection time. However, the factory bevel on the catheter tip that tapers away from the stylette is then lost, making insertion of the catheter into the eye less predictable.
There are two chances to accomplish the Angiocath/trocar exchange: the superonasal and superotemporal trocars. If the exchange is not achieved at either site, a fourth sclerotomy can be created by placing the Angiocath directly through pars plana using its stylette. Great care must be exercised when the Angiocath and stylette are in the eye to avoid contacting the posterior pole of the eye with these long instruments. Alcon is developing a 25-ga. SO injection cannula of appropriate length. This may allow for injection of both 1,000 and 5,000 centistoke SO.
After the SO is injected and all trocars and cannulas are removed from the eye, one or two drops of oil usually leak through the sclerotomy and migrate out through the conjunctival opening. The oil leak stops spontaneously within a few minutes, and no subconjunctival oil is visible postoperatively.
Exercise great care when injecting the SO at 80 psi. Once the SO has begun to reflux into the infusion cannula, the intraocular pressure rises VERY rapidly. Recall that 80 psi is approximately 5.3 atmospheres or 4,053 mmHg. Vigilance is essential to avoid excessive eye pressure.
Removal of SO requires one 20-ga. sclerotomy in phakic patients, although a 25-ga. vitrectomy trocar may be used for the infusion cannula. In pseudophakic patients, an inferior peripheral iridotomy is created at the time the SO is placed. To remove Silikon 1000 in these patients, a 25-ga. vitrectomy trocar is placed for the infusion cannula. A 22-ga. Angiocath is trimmed to 5 mm and connected to the viscous fluid extractor. The Angiocath is placed into the anterior vitreous cavity through an inferior corneal paracentesis and the peripheral iridotomy and the SO removed. To remove 5,000 centistoke SO, use the same technique, but with a 20-ga. Angiocath. The corneal paracentesis is then closed with a 100 nylon suture.
Better Healing, Not Speed
The benefit of 25gPPV techniques—with or without SO—is not speed. Turnover time between cases may be a bit faster with the 25 ga. system, but operative time is usually comparable to a 20-ga. surgery. Time saved starting and finishing the case is lost while performing intraocular manipulations, which may take quite a bit more time due to the narrow caliber of 25-ga. instrumentation. The key is that selected eyes operated with 25gPPV techniques may heal faster, regain vision faster, and generally do better postop than if operated with standard 20-ga. techniques. As we broaden our experience with 25gPPV systems, prospective comparative trials will be needed to validate the initial very favorable but anecdotal impressions. The ability to safely and easily place silicone oil during 25gPPV may significantly expand the range of patients for whom this technique may be considered and will hopefully prove a great advantage for retinal surgeons and our patients.
Dr. Riemann practices at the Cincinnati Eye Institute. He has no financial interest in the instruments or technology discussed.