The past few years have seen an evolution in dry-eye guidelines from several organizations. In 2006, the International Task Force Delphi Panel on Dry Eye made recommendations on the diagnosis and treatment of dry eye.1 In 2007, the International Dry Eye Workshop refined the Delphi Panel's guidelines,2 and a year later, the American Academy of Opthhalmology revised its Preferred Practice Pattern for dry eye, which is a distillation of the literature and practical points from a variety of guidelines.3
These guidelines are widely used and provide a formalized, stepwise approach to treating dry eye. They have also been helpful in educating comprehensive ophthalmologists and patients about the range of dry-eye treatments available, and they have helped justify dry-eye treatments to third-party payers.
Guideline Use
Although the AAO Preferred Practice Pattern for dry eye is widely used, a recent study has found that conformance to specific elements of the guidelines varies significantly. Researchers at
Education
While the stepwise approach outlined in the guidelines may not be anything new for dry-eye specialists, it is helpful for other doctors. "Many doctors basically would treat with artificial tears and ointments, and that was pretty much it," says Christopher J. Rapuano, MD, director of the Cornea Service at Will's Eye Institute and professor of ophthalmology at Jefferson Medical College of Thomas
Dr. Rapuano notes that the guidelines have also helped to educate patients and encourage them to seek treatment. "Patients are more aware, too," he says. "There has been a lot of media play on dry eyes and different treatments for dry eyes. There are now websites for dry eyes, and these patient-oriented websites have popularized the fact that there are many different steps in the management of dry eyes. Patients are now coming in much more knowledgeable about the different steps of dry-eye treatment. Now, they not only know about tears, but they know about Restasis, plugs and autologous serum."
This is time-saving for the doctor. "We don't have to introduce a whole new topic to the patient. We have to explain the pros and cons certainly, but part of the job is already done," Dr. Rapuano adds.
According to Stephen C. Pflugfelder, MD, the guidelines have also been helpful for educating third-party payers about dry-eye treatments. "They may help in convincing managed care or other third-party payers that a patient needs a particular medicine based on this evidence in the literature. There is a consensus that these treatments should be used," says Dr. Pflugfelder, who is director of the
Room for Improvement
Although the guidelines are long and very detailed, there is still room for improvement and further clarification. For example, while the guidelines are helpful in initiating treatment, the stepwise approach may not be best for every patient. "They have a fairly rigid, stepwise approach, and not every patient follows that," Dr. Rapuano says.
"Sometimes, I'll try things in the third box before things in the second box in certain patients. They do say that it is just a general outline and format and that not every patient goes through each of the steps. Treatment needs to be individualized for each patient, and some people may respond differently to certain regimens."
Dr. Pflugfelder agrees. "I think the problem is that the guidelines are a little rigid," he says. "Dry eye is a very heterogeneous disease. Not everyone who presents would fit into the box. They do tend to compartmentalize patients when, in reality, they aren't always that compartmentalized."
He notes that most specialists are already customizing treatment for particular patients. "However, the semi-naïve doctor may just strictly adhere to the guidelines, and he or she might be missing out on some other therapies that might be beneficial," he explains. For instance, the Delphi Panel recommends the use of oral tetracycline in level 3. For some patients, it might be better to initiate treatment in level 2. Punctal occlusion is also level 3, but there may be certain level 2 patients in whom it may be effective."
However, he adds that the guidelines are valuable for physicians in general practice who may not have as much understanding about when to initiate any given therapy. "Now, they have recommendations for where to start," Dr. Pflugfelder says. "I do see a trend in initiating anti-inflammatory therapy at an earlier stage. Previously, doctors may have waited until patients had the disease for years and were beyond help because their disease had resulted in permanent changes. Now, doctors are starting therapy at an earlier stage, where the results may be better."
Michael Lemp, MD, believes that the severity scale may need some tweaking as well. "The
For this reason, a recent Canadian consensus panel has combined grades 1 and 2, resulting in three severity grades (mild, moderate and severe).5
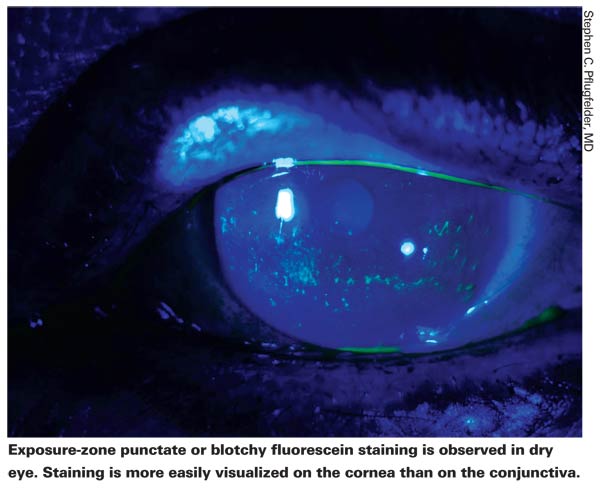
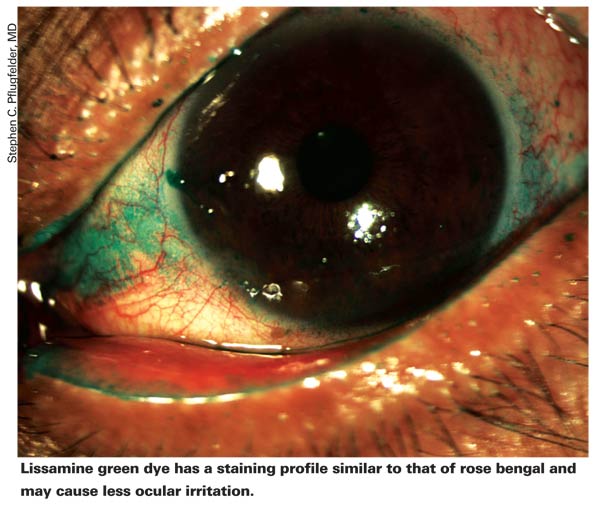
Dr. Lemp notes that most of the tests used to diagnose dry eye are not in concordance with each other because they measure different manifestations of disease. For example, a patient may have a normal Schirmer test, and yet have some staining of the ocular surface. Or, a patient may have a very low Schirmer score and no staining of the ocular surface. "They are both valuable tests, but they don't always support each other," says Dr. Lemp. "Cytokines don't go up evenly. They remain quite low in grades 1 and 2 and then all of a sudden take off in grades 3 and 4. Tear osmolarity is a marker for dry eye, and in early mild disease, tear osmolarity goes up in a more linear fashion than other tests."
Dr. Lemp also explains that there are two types of dry-eye disease: aqueous tear deficient dry eye and evaporative dry eye. In comparison to aqueous tear deficient dry eye, evaporative dry eye is actually much more common, and meibomian gland dysfunction is the most prevalent form of evaporative dry eye. In fact, a recent study concluded that "the margin of the eyelid is an important but currently underestimated structure in the maintenance of the preocular tear film and of the utmost importance for the preservation of ocular surface integrity and in the development of dry eye disease."6
"Some of the tests included in the guidelines don't evaluate meibomian gland dysfunction at all," Dr. Lemp says. "They only evaluate how the lacrimal gland is producing tears. If you have primarily meibomian gland dysfunction, it will not show up on the Schirmer test. Most people with dry eye have a mixed form of the disease, and you will get very variable results in a Schirmer test."
Drs. Lemp and Pflugfelder believe that it may be worth re-visiting the guidelines in the future. Dr. Lemp notes that future guidelines need to specifically address meibomian gland dysfunction. "The guidelines are still treating lacrimal gland dysfunction and meibomian gland dysfunction as two separate diseases. You have to change that mindset," he says.
1. Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: A Delphi approach to treatment recommendations. Cornea 2006;25:900-907.
2. Management and therapy of dry eye disease: Report of the Management and Therapy Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf 2007;5(2):163-178.
3. AAO Preferred Practice Pattern for Dry Eye. http://one.aao.org/CE/PracticeGuidelines/PPP_Content.aspx?cid=65b04ca6-a26d-4454-b27b-46aed841334d, September 2008.
4. Lin IC,
5.
6. Knop E,




