A 59-year-old Caucasian woman presented with a one-month history of increased floaters and decreased vision in her left eye. She stated that her vision was previously equal in both eyes. She was initially evaluated for the floaters four months prior to presentation and found to have a posterior vitreous detachment without evidence of retinal tears or detachments at that time. She denied any history of trauma, pain, headache or neurologic symptoms.
Medical History
|
With regard to her history of multiple myeloma, she was first diagnosed six months prior to presentation and had completed five months of chemotherapy. She had since been in remission and was in the process of preparing for stem cell collection and autologous implantation.
Examination
The patient’s vital signs were stable and within normal limits. Her visual acuity was 20/30 with improvement to 20/25 pinhole in the right eye and 20/60 in the left eye without improvement on pinhole. External examination showed moderate ptosis in both eyes with the right slightly greater than the left. There was no proptosis in either eye. Pupils were equal and reactive without afferent pupillary defect. Confrontational visual fields were full to finger counting in both eyes. Extraocular motility was full in both eyes. Intraocular pressure was 13 mmHg in the right eye and 15 mmHg in the left eye.
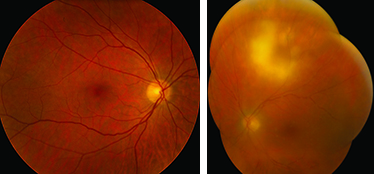
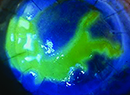
Anterior slit-lamp examination of the right eye was normal. The left eye showed multiple keratic precipitates and 2+ cell and flare present in the anterior chamber. Funduscopic examination of the right eye was normal. Funduscopic examination of the left eye showed significant vitreous haze, mildly attenuated vessels along with perivascular cuffing along the veins, and an intraretinal lesion measuring 6 x 6 mm approximately 5 mm superiotemporal to the nerve (See Figure 1). An old 2 x 1 mm chorioretinal scar was also present.
Please click this link for diagnosis, workup, treatment and discussion.