Any eye-care professional or patient will tell you that the treatment of dry eye has changed and evolved drastically over the years. Not only have treatments advanced, but research has uncovered more potential causes and triggers of dry eye and ocular inflammation. While the common condition can be overwhelming to treat with its many variables and management options, identifying a cause is always the first step, followed by the trial-and-error of different treatment methods.
Here, we’ll hear from the experts about the various ways to approach dry-eye treatment and the methods and interventions they’ve found to be the most effective for their patients.
Approaching the Options
There are three things to consider before deciding on a treatment plan for your dry eye patient, according to Esen Akpek, MD, a professor of ophthalmology and rheumatology at Johns Hopkins University School of Medicine, and director of the Ocular Surface Disease and Dry Eye Clinic at the Wilmer Eye Institute in Baltimore. Dr. Akpek says the three considerations include patient-reported symptoms and concerns, clinical signs and disease severity.
“First of all, we need to recognize that dry eye is a symptomatic disease, in that we have to address the patient’s concerns. Patient-reported outcomes are very important,” Dr. Akpek notes. “The second thing that we have to address is the clinical signs because they have implications. Clinical signs might have to do with blurring of vision or fluctuating vision, especially cellular erosion and short breakup time. Both the patient concern and clinician-measured clinical signs need to be addressed at the same time.
“The next thing is to determine the severity of the disease,” she adds. “All the treatment guidelines or suggestions are based on the severity, but usually, there’s a discordance between the patient-reported and clinician-measured severity. So, you have to start by determining which one to address and how.”
Robert Latkany, MD, a corneal specialist and refractive surgeon at the Dry Eye Center of New York City, agrees with Dr. Akpek that some patients may need to be treated based on clinically measured disease severity, while others may find even mild symptoms intolerable or disruptive to daily life and be more eager to find a solution for immediate relief.
“If someone is miserable but their eyes don’t even look bad, I would call that something that needs urgency, but is that a severe case? Not necessarily,” Dr. Latkany explains. “That’s the problem with this condition. You’ve got three subgroups: You have the one that looks terrible but doesn’t feel too bad, just a little bit dry. I’m still going to treat that person kind of aggressively. Next, you have the patient who doesn’t look that bad, but feels terrible. In the interest of keeping the patient, I’m going to try to make this person happy and treat their symptoms, otherwise they’re going to bail and go to someone else. But, I’m not in as much of a rush to treat that patient, because they don’t really look that bad. Lastly, you have the patient who both looks and feels terrible. For that person, you’ve got to get going with treatment quickly, because that’s truly the most severe.”
 |
 |
Address the Underlying Causes
For many patients, dry-eye symptoms may be improved or relieved by simply identifying and removing the factors that are exacerbating inflammation or abnormal tear production. Encourage anyone with sudden-onset dry eye to review any new products they’ve used or been exposed to lately to help identify a possible allergy or irritant.
“The natural stuff is huge, but often neglected,” explains Dr. Latkany. “I’ll get someone who says their eyes are burning, so I ask them, ‘Have you used any new moisturizers or a new sunblock or makeup product?’ and they answer, ‘Oh, well yeah, I’ve been using this product…’ So, I ask them to do me a favor and do nothing except stop using that one product. Two weeks later, they’ll come back and say, ‘Doc, I’m all better,’ whereas this person could have been plugged, put on Restasis or Xiidra, had LipiFlow or intense pulsed light treatment, you name it. Sometimes, you just have to say, ‘Hey, just stop that, and let’s see what happens.’”
Finding the cause of dry eye to determine the best treatment options requires consistent questioning of the patient about their symptoms, lifestyle and habits. “It’s so critical to get the information out of the patient,” says Dr. Latkany. “Sometimes, you won’t get it from a technician, and sometimes, I don’t get it my own questioning the first exam. I might get it the second exam, or the third exam. But don’t neglect the history-—that’s huge.”
One suggestion Dr. Latkany gives for patients with allergies that may be contributing to or causing dry eye is to invest in an air purifier for their home or bedroom. If the person sleeps with their eyes open, suggest a humidifier to increase the moisture in the room, or tell the person to wear an eye mask or goggles while sleeping and see if their symptoms improve. “For the patient with lagophthalmos who has dryness and scratches caused from that, I’m going to say ‘Hey, try this Refresh P.M. ointment for the next three nights and see how you feel in the morning.’ Maybe I’ll try two things, and suggest the eye mask and the ointment,” says Dr. Latkany. He recommends, however, not to try manual therapies and medicated drops all at the same time to be able to gauge individual effectiveness and avoid unnecessary intervention.
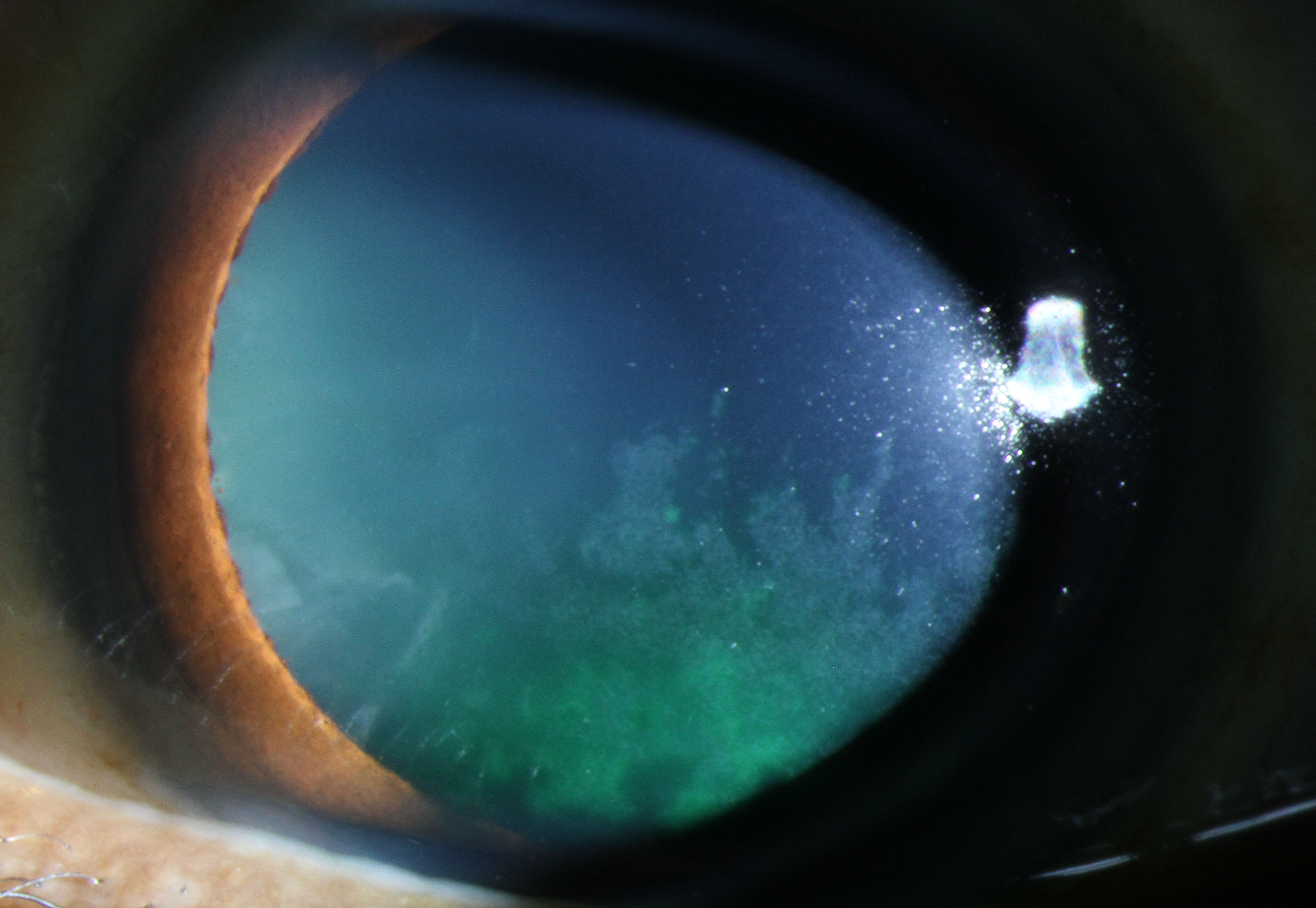
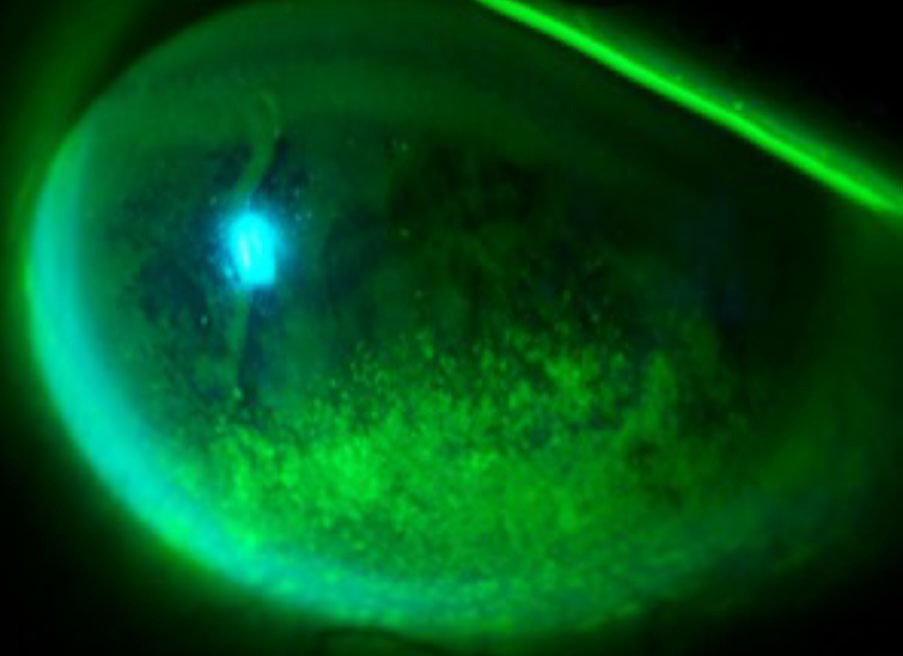 |
| Confluent inferior corneal fluoroscein staining in patient with dry eye and lagophthalmos due to Bells’ palsy. (Image courtesy of Esen Akpek, MD.) |
Other underlying conditions contributing to dryness that may be worth testing for include neurotrophic keratitis (NK), which Dr. Akpek notes could even be caused by the continuous inflammation of the eye. “One thing I recently started doing for my dry eye patients is routinely checking corneal sensation. I’ve actually found that decreased corneal sensation isn’t very uncommon among patients with severe dry central cornea, and especially if they say they aren’t in pain, my mind goes to NK. If I test them and they do have decreased corneal sensation, I’ll prescribe the appropriate treatment, which is a recombinant nerve growth factor,” says Dr. Akpek. Oxervate is the newest FDA-approved recombinant nerve growth factor therapy to treat NK.
Vatinee Bunya, MD, an associate professor of ophthalmology at Penn Medicine and co-director of the Penn Dry Eye and Ocular Surface Center, urges ophthalmologists to screen patients for another potential underlying cause of eye dryness and irritation: Sjogren’s Syndrome. “Sjogren’s is very underdiagnosed,” Dr. Bunya warns. “The majority of Sjogren’s patients have dryeye symptoms, and as eye care providers, we’re the first ones to see them. Just asking about the presence of symptoms such as dry mouth or fatigue could help you detect underlying Sjogren’s Syndrome.”
Whether it be environmental, underlying or systemic, aqueous deficiency or meibomian gland dysfunction, pinpointing the cause of dry eye will help you narrow down treatment options and guide you and your patient’s next steps.
Topical Therapy
When avoidance of environmental triggers falls short, here’s the latest thinking on topical options.
• Artificial tears. Tried-and-true artificial tears still hold up as the first thing to prescribe a patient complaining of dry-eye symptoms in almost every mild to moderate case (though if symptoms are mild and recurring, also continue to investigate the potential role of environmental factors).
It’s important to recommend preservative-free drops to patients who will be using them on a daily basis to prevent adverse reactions. Eye drops with preservatives are only safe for occasional patient use; in other words, for people who don’t have frequent eye dryness and probably aren’t in your office.
Dr. Bunya says that she always advises patients to start the treatment process by using preservative-free drops consistently but notes that patient compliance may be an issue for some.
“For patients with mild dry eye, usually I’ll recommend preservative-free artificial tears that come in individual vials,” Dr. Bunya says. “It’s important that they’re preservative-free because bottled tears have preservatives in them, and they can actually cause dry eyes if you use them frequently. Usually, I’ll start treatment by telling patients to use the drops two to four times each day to start, even if their eyes feel okay. Often, patients will only use the drops if their eyes are bothering them, but then it’s hard to get the eyes to start feeling better once they are already irritated. So, a lot of times, even just starting with twice a day, every day for a few weeks is a helpful first step.”
Dr. Akpek adds that in cases where preserved drops must be used, non-benzalkonium chloride (BAK) drops are the safer option to help prevent vision damage or worsening of symptoms.
• Prescription drops. For the patients who need more relief than artificial tears can provide, physicians will often turn to a prescription medication targeting inflammation. Restasis (cyclosporine ophthalmic emulsion) 0.05%, Xiidra (lifitegrast ophthalmic solution) and Cequa (cyclosporine ophthalmic solution) 0.09% are the three non-steroidal anti-inflammatory drops for dry eye. The most recent FDA-approved drop, Eysuvis (loteprednol etabonate ophthalmic suspension) 0.25%, is an ocular corticosteroid approved for short-term treatment of dry eye.
Though most ophthalmologists are familiar with the effectiveness of Restasis and Xiidra, in terms of the drugs that arrived in recent years, Cequa, when compared to vehicle at almost three months in two randomized, prospective studies, induced a statistically significantly higher percentage of eyes with increases of at least 10 mm from baseline in Schirmer’s wetting.1 For Eysuvis’ part, in prospective, randomized trials, it reduced ocular discomfort throughout the trial period, with a statistically significant improvement reduction of discomfort in the treatment group at day 15.2
 |
| If corneal staining persists after treatment, clinicians will intensify the therapy. (Image courtesy of Vatinee Bunya, MD.) |
Dr. Latkany notes that there are some adverse events to be aware of. “None of these prescription drugs is a home run,” he says. “All have side effects that prevent a significant percentage of patients from successfully using them. From burning, pain and blurry vision for Restasis, Xiidra and Cequa, to elevated eye pressure and cataracts for Eysuvis, they have to be monitored carefully. That said, they do offer relief for some patients, whether used individually or in combination with each other.” If used in combination, experts advise that patients wait at least 10 to 15 minutes between each product’s instillation. Dr. Latkany says he avoids prescribing the three non-steroidal drops to patients with ocular rosacea and dry eye, as they tend to have higher failure rates due to negative side effects.
Though drops offer short-term relief for many, relying on any of them to treat symptoms long-term is unrealistic and could even make eyes worse, Dr. Akpek explains. “Treating dry eye with only topical medication is counterintuitive. Every time you put topical eye drops on the ocular surface, you disrupt the homeostasis of the actual tear film and dilute the good tears that patients might produce. So, I think systemic or local treatments work better in the long run.”
Punctal Plugs
For patients who aren’t responding well enough to drops and are experiencing excess tear duct drainage, punctal plugs are still one of the more effective and least invasive treatment options available for chronic dry-eye cases. Punctal occlusion is usually done fairly early in treatment for patients with moderate dry eye who don’t find sufficient relief from topical medications alone.
“If you have solid evidence in the office that the patient has low tear production (for example, a decreased tear lake or a low Shirmer’s test), then I would have a low threshold for trying punctal occlusion,” says Dr. Bunya. “Contact lens wearers especially tend to respond well to it.”
Dr. Latkany says that he’ll put punctal plugs in quicker for some patients than others, but that each case has to be handled based on a patient’s symptom severity and comorbidities. “For that purely aqueous deficient patient, I’ll start off with two lower plugs,” he says. “If the two lower plugs aren’t enough, I’ll do two upper plugs. But in my grand pool of patients, that is not the most common patient, for sure. Even though I only see dry-eye patients, it’s a mixed-bag; for example, someone who’s aqueous deficient who also has allergies or rosacea, I’ll treat that patient differently (address the allergy and treat inflammation to see if symptoms improve before considering plugs). But, I will only ever treat with one thing at a time to understand what is working and what’s not.”
Christopher J. Rapuano, MD, Chief of Wills Eye Hospital’s Cornea Service, says that although he’s usually not hesitant to plug lower tear ducts, he’s apprehensive about plugging upper tear ducts because he’s found that they aren’t as comfortable for the patient.
Meibomian Gland Dysfunction
Inflammation in patients with anterior blepharitis and meibomian gland dysfunction must be addressed first and foremost, as it’s the root cause of MGD and ocular discomfort.
The initial approach to addressing mild dry eye due to meibomian gland dysfunction is by instructing the patient to clean their eyelids, especially if they haven’t been doing so already. Dr. Latkany believes this is a crucial part of a patient’s personal eye health and that a consistent cleaning regime could have a large impact on the frequency and severity of dry-eye symptoms.
“I often use the analogy of cleaning your gums and your teeth,” Dr. Latkany says. “You have to floss, and you have to brush teeth every day. Then, when you go to the dentist, they do a little better or a job than you are doing at home. But, you can’t come to me every six months and have me clean your eyelids if you haven’t been doing it at home and keeping up with the maintenance.” He recommends setting aside 10 minutes to instruct your patients on how to clean their eyelids at home and increase the chance that they might comply if they know how to do it properly.
Dr. Bunya also emphasizes the importance of lid cleaning for dry eye patients of all severities, which she suggests can be done using diluted baby shampoo or over-the-counter cleansers. In addition, she recommends treating mild to moderate dryness by advising patients to apply warm compresses over their eyes twice a day for five minutes at a time.
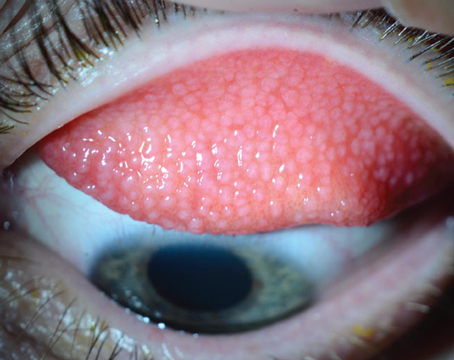
 |
| This dry-eye patient has a moderate amount of lissamine green dye staining nasally and temporally. Note the silicone punctal plug in the left lower tear duct. (Image courtesy of Christopher Rapuano, MD.) |
Dr. Rapuano says that patients with mild to moderate dry eye can be prescribed erythromycin antibiotic ointment to apply to lids at bedtime as the next step when drops and regular lid cleanings aren’t sufficient. “Erythromycin kills two birds with one stone; it lubricates the eyes overnight to help address any aqueous deficiency contributing to the dry eye, and secondly, it functions to kill any kind of bacterial overgrowth on the eyelids,” Dr. Rapuano explains. “It’s also a mild anti-inflammatory, and it decreases the lipid composition in the oil glands so they work a little better.”
Dr. Rapuano does note that “azithromycin works better than erythromycin, but logistically, it’s harder to get: it’s more expensive, insurance doesn’t want to cover it and it’s only FDA-approved for a two-week course.”
It could be helpful to screen MGD patients for new or existing rosacea, a skin condition that can clog up the oil glands in the eyelids (ocular rosacea). Daily eyelid cleanings or using topical antibiotics can be useful in mild to moderate cases, and devices like LipiFlow may be necessary for more severe ones.
“Certainly, if they have a lot of blepharitis or rosacea, consider oral doxycycline or oral azithromycin,” says Dr. Bunya.
Dr. Rapuano also says doxycycline is a solid next step once the MGD patient has tried both erythromycin and azithromycin. “I’m not a huge fan of systemic antibiotics long-term for a relatively limited problem, but for some people, doxycycline is very helpful,” he says. “I’ll do a medium dose for two weeks and then cut that dose in half for another four or six weeks and see how they do.” He notes that sometimes people will find symptom relief after a six- or eight-week course of doxycycline, while others may need to stay on it for months or even years to achieve desired relief.
LipiFlow and TearCare are two thermal eyelid procedures that can be considered for those with severe dry eye caused by MGD. “They work through a combination of a heating of the eyelids to soften up the oils and then a massaging of the lens to clean out the oil glands and remove blockages,” explains Dr. Rapuano. “I’ve done both of those with great success in some patients, medium success in most patients and zero success in some patients.”
Intense pulsed light therapy is a relatively new treatment for MGD. “It uses bright light to treat abnormal blood vessels in the superficial skin to decrease the inflammation of the eyelids,” explains Dr. Rapuano. However, most of these therapeutic procedures aren’t covered by insurance and can be costly. Dr. Bunya says she “[tends] to try a lot of the other treatments before recommending LipiFlow or intense pulsed light, just because those are usually an out-of-pocket expense for the patient.”
THE DREAM Study: Omega-3 Called into Question Though the results were striking, the study received pushback for a couple of reasons, one being that most participants were simultaneously continuing other treatment interventions throughout its duration. The DREAM research team aimed to conduct a study that was considered “real-world,” meaning that outside factors could’ve snuck in and swayed results; however, this is just speculation at this point. One argument against the validity of the findings has already been debunked: Namely, that the placebo in the study, refined olive oil, could have a therapeutic effect on dry eye. The researchers say that the low dosage given to participants and the oil refinement process exclude it from offering sufficient health-promoting benefits, so it’s unlikely that’s the explanation for the similar results between the omega-3 pills and the olive-oil placebo. Clearly, as the DREAM Study has shown, the question of whether omega-3 supplements are effective in improving dry eye is a topic requiring further research. However, there’s no denying that a diet rich in fruits, vegetables and plant-based foods could benefit all patients, especially those dealing with dry eye. A 2020 study linked higher consumption of vegetables and vegetarian protein alternatives with lower severity of dry eye.2 1. Hussain M, Shtein RM, Pistilli M, et al. The dry eye assessment and management (dream) extension study - a randomized clinical trial of withdrawal of supplementation with omega-3 fatty acid in patients with dry eye disease. Ocul Surf. 2020;18:1:47-55. 2. Flanagan J, Huang B, Tavakoli S, et al. Is dry eye related to diet? Invest Ophthalmol Vis Sci 2020;61:7:330. |
Severe Dry Eye
There are many therapies currently available for severe dry eye, but success rates depend on the cause and severity of symptoms and a person’s eye anatomy. Some popular techniques to treat severe cases include autologous serum eye drops (ASEDs), scleral lenses and various procedures, such as the few mentioned above (LipiFlow, TearCare and intense pulsed light therapy).
Autologous serum eye drops contain ingredients found in natural tears that can’t be replicated by artificial ones including antibodies, albumin, Vitamin A and epidermal growth factors. The serum eye drops are made using a very small amount of the patient’s blood drawn during a brief appointment.
“Especially in the last couple of years, you can see that patients are responding well to the serum,” Dr. Bunya observes. “They tend not to have a lot of side effects because it’s made from their own blood. I’ve started to prescribe autologous serum drops sooner, even in patients with moderate dry eye, and have had great success with that.” A downside to serum drops, however, is that they’re another treatment not often covered by insurance.
Scleral or bandage contact lenses are both options to consider for moderate to severe dry-eye patients. Scleral lenses, such as the PROSE lens, “are filled with tears, and then the patient puts it in, and it bathes the eye with tears all day long,” Dr. Rapuano explains. Typically more affordable for patients, soft bandage contact lenses reinforce damaged tissues and protect the nerve endings from abrasion caused by eyelids.
Dr. Rapuano adds that steroid drops could be helpful in short-term cases of severe dry eye but may do more harm than good when used to treat chronic conditions such as aqueous deficiency.
Lateral tarsorrhaphy is an advanced treatment option available for certain patients with severe evaporative dry eye. “If you have a patient whose eyes are really open, you can do a permanent tarsorrhaphy where you actually stitch the eyes partly close, so that there’s not as much evaporation,” explains Dr. Rapuano. “We typically do that for some older or rheumatoid arthritis patients, but it’s a pretty dramatic treatment choice.”
To find the most success treating today’s large population of dry eye patients, physicians advise moving in a stepwise fashion, trying one method at a time and then supplementing with others in cases of unimproved symptoms or higher severity.
Dr. Rapuano is a consultant for Bio-Tissue, Dompé, Glaukos, Kala, Oyster Point, Sun Ophthalmics, Tarsus and TearLab. Dr. Akpek is a consultant for Novalique and an investigator for Ocular Therapeutix. Dr. Bunya and Dr. Latkany report no financial interest in any of the products mentioned.
1. Goldberg DF, Malhotra RP, Schechter BA, et al. A Phase 3, randomized, double-masked study of OTX-101 ophthalmic solution 0.09% in the treatment of dry eye disease. Ophthalmology 2019;126:9:1230-7.
2. Holland E, Nichols K, Foulks G, et al. Safety and efficacy of KPI-121 ophthalmic suspension 0.25% for dry eye disease in four randomized controlled trials. Presented at: AAO 2020: November 13-15, 2020; virtual meeting.