| Richard S. Hoffman, MD Eugene, Ore. |
Because cataract surgeons are using advances in technology to address higher-order optical aberrations, the measurement of functional vision is becoming increasingly important. Contrast sensitivity testing is assuming a prominent place in our evaluation of surgical modalities, because it reflects functional vision and correlates with visual performance.
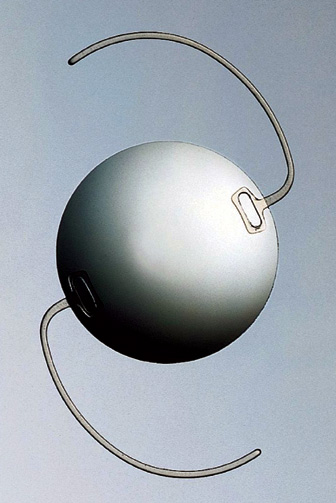
The development of the Tecnis Z9000 intraocular lens (Pfizer, New York) is the first step in integrating wavefront technology and cataract surgery. The Tecnis is the first foldable IOL designed to correct higher-order optical aberrations.
This lens has been designed with a modified prolate anterior surface to compensate for the spherical aberration of the cornea, which will eliminate total ocular spherical aberration.
 |
Additionally, clinical data shows that the modified prolate IOL provides superior functional vision and improved visual performance when compared with conventional spherical IOLs.
Contrast Sensitivity
Contrast sensitivity declines with age, even in patients without ocular pathology. When people are young, the crystalline lens has negative spherical aberration, and the cornea has positive spherical aberration. In youth, the two neutralize each other out. As people age, however, while the cornea maintains its positive spherical aberration, the lens has less negative spherical aberration. Now, the two not only don't neutralize each other out, but there is an additive effect so that people have increasing positive spherical aberration as they age.
All IOLs available today except the Tecnis have positive spherical aberration, so the lower-order aberrations are eliminated, but the higher-order aberrations are not addressed.
Compensating for Aberration
Cataract surgeons cannot look at IOLs as isolated lenses. They work in coordination with the cornea. The Tecnis lens was designed to compensate for the average spherical aberration of the cornea and to improve the ocular optical quality of pseudophakic patients. Its design is based on the average human cornea. The amount of negative spherical aberration incorporated into this IOL was based on the average positive spherical aberration of 71 cataract patients. Subsequently, independent investigators have confirmed the mean corneal spherical aberration value in 228 eyes of 134 patients.1
The Tecnis is a unique IOL with a modified prolate anterior surface with negative spherical aberration, which is designed to approximate the optical system of the youthful eye. Researchers believe that it will produce higher quality retinal images.
The Tecnis has a biconvex design, a refractive index of 1.46, and an optic diameter of 6 mm. It has a posterior and anterior sharp-edge design.
Studies have shown that using a modified prolate IOL during cataract surgery can provide superior contrast sensitivity under both mesopic and photopic conditions. Additionally, researchers have found that the spherical aberration of the eye after cataract surgery can be eliminated by modifying the anterior surface of the IOL.
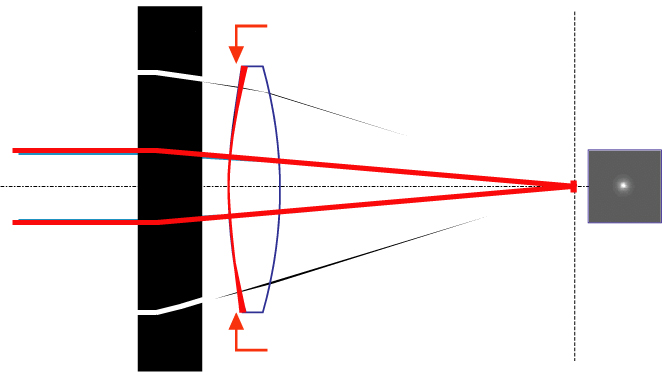 |
| Z-SHARP optic Technology: Spherical intraocular lenses have positive spherical aberration, resulting in significant positive spherical aberration in the pseudophakic eye after cataract surgery. The Tecnis lens reduces the peripheral power of the IOL by making the front surface a modified prolate, causing the lens to have a negative spherical aberration. The result is an eye with very little remaining spherical aberration in the entire optical system. |
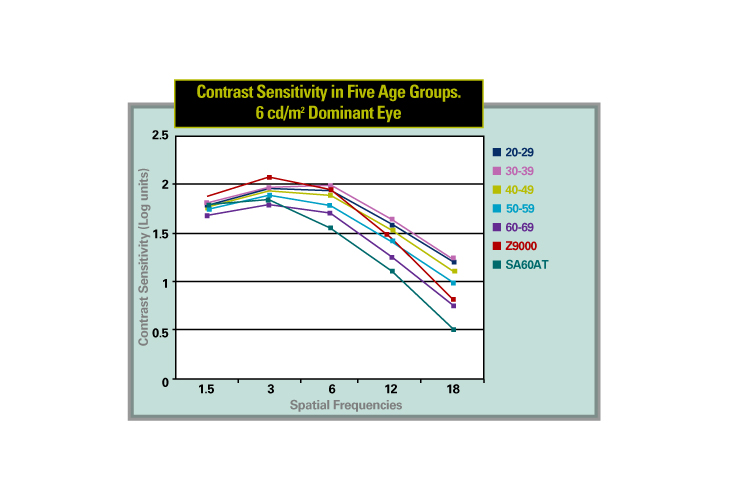
We conducted a prospective randomized trial comparing the contrast sensitivity obtained with the Tecnis Z9000 IOL with the contrast sensitivity obtained with the AR40e Opti-Edge IOL (AMO).2 When we assessed peak mesopic contrast sensitivity, we found that the Tecnis IOL provided a 0.27 log unit (77.9 percent) gain in peak contrast sensitivity at three cycles per degree compared to the AR40e. We found no statistically significant difference between the Tecnis mesopic contrast sensitivity and the AR40e photopic contrast sensitivity. This means that patients implanted with the Tecnis see as well in dim light as patients with the AR40e see in bright light.
We then compared patients in this study with healthy patients between the ages of 20 and 50 years, and we found that contrast sensitivity was better in the patients implanted with a Tecnis IOL than it was in healthy patients aged 20 to 30 years.3
Other researchers recently conducted a randomized study comparing the Tecnis IOL with the SI-40 IOL (AMO) in 45 patients with bilateral cataract.4 Thirty-seven of the 45 patients were examined at all follow-up visits up to three months after surgery. At three months postoperatively, the eyes with the Tecnis IOL had significantly better best-corrected visual acuity; however, the improved quality of vision was more apparent when assessing low-contrast visual acuity and contrast sensitivity. Wavefront measurements revealed no significant spherical aberration in eyes with a Tecnis Z9000 IOL, but significantly positive spherical aberration in eyes with an SI-40 IOL.
 |
| Eyes implanted in the Technis foldable lens have shown statistically significant differences inphotopic and low-light contrast sensitivity. |
A prospective study comparing the Tecnis IOL with the spherical SA60AT from Alcon also showed improvements in contrast sensitivity with the Tecnis IOL.5 This study included 30 patients with senile cataract but no other eye pathology who were scheduled for sequential bilateral surgery. Eyes implanted with the Tecnis foldable lens had statistically significant differences in photopic and low light contrast sensitivity.
Image Contrast, Contrast Sensitivity
A prospective, randomized study compared the Tecnis Z9000 modified prolate IOL with conventional spherical silicone and acrylic IOLs in terms of effect on retinal image contrast and functional visual performance.6 The study included 221 eyes in 156 patients that were randomly assigned to receive one of three IOLs with six months of follow-up. Researchers measured visual acuity, fundus photographic retinal image contrast, and functional acuity contrast testing.
In the first month after surgery, uncorrected visual acuity was best in the aspheric IOL group. Patients in this group experienced up to a 47-percent increase in contrast for photopic, 38-percent increase in photopic with glare, 50-percent increase in mesopic, and 50-percent increase in mesopic with glare.
Patients implanted with spherical silicone IOLs had no increase in contrast testing when compared to cataract. Digital analysis of retinal imaging demonstrated increased threshold luminance levels in the aspheric group and a four-fold increase in image contrast compared to the silicone and acrylic groups.
Patients implanted with the Tecnis IOL had significant improvement in objective retinal image contrast and in visual performance as measured by visual acuity and functional acuity contrast testing. This improvement was most pronounced in night vision and night vision with glare contrast testing when compared with conventional spherical silicone and acrylic IOLs.
Night Driving
Researchers conducted a large, prospective, randomized, double-masked, multicenter trial that included 77 patients who were implanted with the Tecnis Z9000 IOL in one eye and the SA60AT IOL in the other eye.7 This study found a statistically significant difference in best-corrected ETDRS visual acuity with the Tecnis IOL at 90 days after surgery. Using wavefront aberrometry, spherical aberrations were eliminated in eyes implanted with the Tecnis IOL but were still observed in control eyes.
In 29 of these patients, double-masked night driving simulator tests were conducted. Patients implanted with the Tecnis IOL had improved detection and identification distances for almost all targets. Examples of targets used include road signs or pedestrians, under a variety of different conditions, city or rural.
The study found that the Tecnis IOL is better than the SA60AT for allowing patients to detect most of the targets under various conditions. The greatest advantage seen was for a hazard target such as a pedestrian under rural or lower light conditions.
The study also found that those eyes implanted with the Tecnis IOL under the effect of glare performed as well as the control eyes without glare. Additionally, the driving test performance of patients correlated significantly with their residual spherical aberration. This may suggest that correcting spherical aberration may improve a driver's ability to recognize targets earlier while operating under reduced visibility conditions.
The Future
In the future, there is the potential for customization of the Tecnis. We are beginning to measure patients preoperatively using corneal topography and software that converts the corneal elevation data from the topography into Zernike polynomial expansion to determine the corneal spherical aberration. If we can prove that there is an advantage to selecting the IOL based on corneal spherical aberration, then there will be a rationale for creating lenses that correct small, medium, or large amounts of spherical aberration. Patients who have had myopic LASIK, for example, may have increased amounts of corneal spherical aberration.
The development of a prolate multifocal IOL offers further potential in the field of refractive optics. The multifocal implant will have diffractive optics for multifocality and the modified prolate anterior surface. Clinical studies on the Tecnis multifocal IOL are about to begin in this country.
Additionally, the Light Adjustable Lens (Calhoun Vision) uses wavefront sensing to correct optical aberrations. This silicone IOL with photosensitive material can be adjusted after implantation to correct myopia, hyperopia, astigmatism and possibly coma or spherical aberration.
The lens is implanted based on normal IOL calculations. A few weeks later, after the lens is seated in the eye, the total wavefront of the eye is measured. These errors are programmed into the ultraviolet light source (a digital light delivery device designed by Carl Zeiss Meditec). This will actually remodel the lens in such a way that it corrects for any residual spherical equivalent error or astigmatism, and also higher-order aberrations. The only drawback is that patients must stay out of the sun for three or four weeks until the lens is adjusted. This lens has not yet begun clinical investigation in the United States.
Wavefront technology will continue to be important in cataract surgery. In fact, wavefront-designed IOLs may be the answer to refractive surgery. Today, children with refractive errors get glasses, teenagers get contact lenses, young adults get refractive surgery, middle-aged adults get bifocals or reading glasses, and senior citizens get cataract surgery. In the future, when people reach early adulthood, they will get refractive lens exchange. It will address all of their refractive errors, and it will allow them to accommodate well so they will never become presbyopic or develop cataracts. They won't have to experience degradation of vision as they age.
Dr. Fine is clinical professor, Dr. Hoffman is clinical associate professor, and Dr. Packer is clinical assistant professor at Oregon Health & Science University. They are also in private practice together at Drs. Fine, Hoffman, & Packer in Eugene, Ore. Contact them at (541) 687-2110, fax (541) 484-3883, or by e-mail at mpacker@finemd.com.
1. Wang L, Dai E, Koch DD, Nathoo A. Optical aberrations of the human anterior cornea. J Cataract Refract Surg 2003;29:1514-1521.
2. Packer M, Fine IH, Hoffman RS, Piers PA. Prospective randomized trial of an anterior surface modified prolate intraocular lens. J Refract Surg 2002;18(6):692-696.
3. Packer M, Fine IH, Hoffman RS. Functional vision, wavefront sensing, and cataract surgery. Int Ophthalmol Clin 2003;43:79-91.
4. Mester U, Dillinger P, Anterist N. Impact of a modified optic design on visual function: clinical comparative study. J Cataract Refract Surg 2003;29: 652-660.
5. Bellucci R, Morselli S, et al. Contrast sensitivity with Tecnis IOL with negative spherical aberration and with conventional IOL. J Glaucoma (in press).
6. Kershner RM. Prospective evaluation of aspheric, silicone and acrylic IOLs on visual performance (Abstract 801). Symposium on Cataract, IOL, and Refractive Surgery, American Society of Cataract and Refractive Surgery. San Francisco, April 12-16, 2003.
7. Packer M. Evaluation of a modified prolate surface IOL with the WASCA Analyzer. Publication No: 000000-1276-350, Carl Zeiss Meditec, Jena, Germany, 2003.



