Although laser refractive surgery is only approved by the Food and Drug Administration for people 18 years and older, there are some instances in which refractive surgery is appropriate for children. For example, in children with bilateral high refractive error or unilateral severe anisometropia with amblyopia who cannot wear glasses or contact lenses, refractive surgery can be used as a last resort.
Not Ideal for Children
Refractive surgeons agree that refractive surgery should typically be reserved for patients who are 18 or older, except in special cases. "I have never performed refractive surgery on anyone under 18, and I personally don't like to do refractive procedures on people under the age of 21 for a couple of reasons," says Richard Lindstrom, MD, who is in practice in
He also notes that it's difficult to obtain high-quality informed consent in very young patients. "They usually haven't experienced any of life's hard knocks, and it's hard for them to imagine that they are not invincible and that everything won't be perfect," he says.
However, there are groups of children who can benefit from undergoing refractive surgery if traditional therapy is not working. "One group is patients with high anisometropia," says Evelyn Paysse, MD, who is in practice in
She says there is a third group that only includes a few patients. This is a smorgasbord group of children with high refractive error and either craniofacial abnormalities that make spectacle or contact lens wear impractical (e.g., Goldenhar's with microtia and/or limbal dermoids) and those with severe neck weakness (e.g., some children with cerebral palsy) whose spectacles fall down their nose.
For children who require refractive surgery, most surgeons prefer surface ablation over LASIK. "We made a conscious decision not to do LASIK because we didn't want to cut the cornea," says William Astle, MD, who is in practice in
He recently conducted a study and found that PRK and LASEK are effective and stable surgical alternative treatments in children with refractive errors who failed conventional methods of treatment.1
This study included 56 eyes of 39 patients who underwent PRK or LASEK under general anesthesia. Patients' mean age at the time of surgery was 6.5 years, with a range of 1.0 to 17.4 years. At the final postoperative examination, the mean spherical equivalent was -1.73 D in all patients, -3.2 D in PRK patients, and -1.37 D in LASEK patients. All eyes had a stable refraction and corneal clarity long-term. In the 28 eyes that were measurable preoperatively, visual acuity improved by a mean of 1.6 lines, with a range of zero to seven lines. Seven patients had measurable stereopsis before surgery and 19 after PRK or LASEK. No patient had reduced BCVA or loss of binocular fusion postoperatively.
Anisometropic Amblyopia
Pediatric patients with anisometropia are at high risk of developing amblyopia. These patients can be very difficult to treat, and some won't or can't wear glasses or a contact lens. "If you can eliminate the anisometropia with an excimer laser, then they have a much better chance of getting good binocular function," Dr. Lindstrom says. "Most research suggests that if the two eyes are more than 3 D apart, you basically end up with a monofixation syndrome. You can't really get full development of stereopsis, and in many cases you end up with relatively dense amblyopia. We see these anisometropic amblyopes all the time."
Dr. Paysse conducted a study to evaluate the long-term visual acuity and refractive error responses to PRK for the treatment of anisometropic amblyopia in children.2 The study included 11 children between the ages of 2 and 11 years who were noncompliant with conventional therapy with glasses or contact lenses and occlusion therapy and who underwent PRK. Mean preoperative refractive errors were -13.70 D (±3.77 D) for the myopic patients and +4.75 D (±0.50 D) for the hyperopic patients. At last follow-up, mean postoperative refractive errors were -3.55 D (±2.25) for the myopic group and +1.41 D (±1.07) for the hyperopic group. Additionally, cycloplegic refractions in four of the eight myopes and all hyperopes were within 3 D of the fellow eye. Seven children underwent visual acuity testing preoperatively and postoperatively, and five had uncorrected visual acuity improvement of at least two lines.
LASEK has also shown promising results in children with anisometropia who are unable to tolerate conventional methods of treatment or in whom these methods fail.3 A study conducted by Dr. Astle included 53 children with anisometropia who underwent LASEK under general anesthesia. Patients were divided into three groups: myopic difference greater than 3 D, astigmatic difference greater than 1.5 D, and hyperopic difference greater than 3.5 D. Children were followed for at least one year. Patients' mean age at treatment was 8.4 years, with a range of 10 months to 16 years. The mean preoperative anisometropic difference was 6.98 D in the entire group, 9.48 D in the myopic group, 3.13 D in the astigmatic group, and 5.5 in the hyperopic group. One year after LASEK, the mean anisometropic difference decreased to 1.81 D in the entire group, 2.43 D in the myopic group, 0.74 D in the astigmatic group, and 2.33 D in the hyperopic group, and 54 percent of all eyes were within 1 D of the fellow eye, 68 percent were within 2 D of the fellow eye, and 80 percent were within 3 D of the fellow eye. Preoperative visual acuity could be measured in 33 children. Postoperatively, 63.6 percent of children had an improvement in best-corrected visual acuity, and the others had no noted change.
Another study found that LASEK improved visual acuity in pediatric hyperopia with or without associated hyperopic anisometropic amblyopia.4 The study included 72 hyperopic eyes in 47 patients. Patients' mean spherical equivalent was +3.42 D (range: 0.00 to +12.5 D) preoperatively and +0.59 D (r: -1.25 to +2 D) one year postoperatively. After LASEK, 41.7 percent of eyes had improved corrected distance visual acuity. No patient had reduced corrected distance visual acuity or loss of fusional ability. There was a 25-percent improvement in stereopsis at one year. The hyperopic anisometropic amblyopia subgroup included 18 eyes in 10 patients. Patients' mean anisometropic difference was 4.39 D (r: +1.75 to +7.75 D) preoperatively and +0.51 D (r: 0 to +0.875 D) at one year. One year postoperatively, 83 percent of anisometropic eyes were within ±1 D of the fellow eye, and 94 percent were within ±3 D. Postoperatively, 64.7 percent of eyes had improved corrected distance visual acuity with no reduced corrected distance visual acuity or loss of fusional ability. At one year, there was a 22-percent improvement in stereopsis.
According to Dr. Paysse, for refractive error that is outside the limits of PRK and LASEK (more than 10 to 12 D), phakic intraocular lenses and refractive lensectomy may be shown in the near future to be viable alternative surgical options.
Challenges and Concerns
Although surface ablation has shown promising results in children who have failed traditional therapy, these cases have some unique challenges and concerns.
For example, a minimum age has not been established. In the
"My opinion is that there is a huge change in refractive error in children during the first two years of life and the cornea is softer than after 2 years of age, so, with excimer laser, the response to treatment may be unpredictable in this younger age group," Dr. Paysse says.
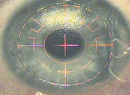
She notes that patients with thin corneas are not good candidates for refractive surgery. It is important to do pachymetry measurements centrally and peripherally to make sure patients have normal corneal thickness. The cornea should be thicker in the periphery than in the center, she explains. Topography is also very helpful if it can be obtained.
She treats patients with myopia, hyperopia and some astigmatism. "However, I'm not as thrilled about treating astigmatism because most of my children are done under general anesthesia, and it's harder to ensure that you are treating right on axis," she says.
Another issue is determining when a patient has failed traditional therapy, according to Erin Stahl, MD, a pediatric ophthalmologist in
Dr. Stahl is currently working to set up a pediatric refractive surgery program. The program will include excimer laser, phakic IOLs and refractive lens exchange. All procedures will be done at the local children's hospital. "The most difficult thing is the logistics of getting pediatric anesthesia and an excimer laser in the same place. Once the child is anesthetized, he or she is not fixating, so you have to be a lot more aware of having everything on-plane and making sure the eye is pointing straight up the whole time," she says.
Success Stories
Dr. Astle and Dr. Paysse have been performing refractive surgery in children for more than a decade, and they note that the patient benefits are much more far-reaching than visual acuity. "These are life-changing procedures," Dr. Paysse explains. "It is so much more than just giving them vision. It really changes their personalities because the children who are bilaterally affected and are not wearing correction are really isolated from the world. When we see them, they are combative, fearful and extremely hard to deal with. Their families report that this behavior is typical at home, too."
She notes that, postoperatively, parents tell her almost uniformly that the procedure has changed not only the patient's life, but that of the family as well. "The children become more social and interested in things. They become more friendly and easy to manage in our office," she adds.
Her first bilateral pediatric patient was a 5-year-old girl with refractive error in both eyes of approximately -14 D who was wheelchair-bound, and Dr. Paysse would have to put her to sleep to perform an exam because she was so combative. "At her three-month postop visit, she came in walking with a walker and hugged me. She had never walked before. At her six-month exam, she came in walking unassisted," Dr. Paysse says.
Dr. Astle has seen similar results in his patients. His most extreme patient was an infant who was -25 D. "We lasered for -19.5, and we actually got a -23 effect," he says. "That might be the type of kid that you would worry that we're changing the cornea so much that we might get ectasia. He is 12 years old and was treated 12 years ago. Unfortunately, we don't have his pachymetry readings pre-laser, but we just did them, and his pachymetry readings are 383 µm. There are no signs of ectasia, and he's wearing glasses that are -6 D now. He went from being labeled extremely developmentally delayed at 6 months of age to functioning like a normal kid."
1. Astle WF, Fawcett SL, Huang PT, Alewenah O, et al. Long-term outcomes of photorefractive keratectomy and laser-assisted subepithelial keratectomy in children. J Cataract Refract Surg 2008;34:411-416.
2. Paysse EA, Coats DK, Hussein MA, Hamill MB, Koch DD. Long-term outcomes of photorefractive keratectomy for anisometropic amblyopia in children. Ophthalmology 2006;113:169-176.
3. Astle WF, Rahmat J, Ingram AD, Huang PT. Laser-assisted subepithelial keratectomy for anisometropic amblyopia in children: Outcomes at 1 year. J Cataract Refract Surg 2007;33:2028-2034.
4. Astle WF, Huang PT, Ereifej I, Paszuk A. Laser-assisted subepithelial keratectomy for bilateral hyperopia and hyperopic anisometropic amblyopia in children: One-year outcomes. J Cataract Refract Surg 2010;36:260-267.