To get the best outcome with a toric lens, surgeons say it’s important to do three things well: measure the astigmatic axis accurately; have an effective way to visualize the target meridian when the patient is on the table; and position the lens inside the eye during surgery so the lens is aligned with that target meridian and remains there postoperatively. Here, three surgeons with extensive experience implanting these lenses share their advice on how to achieve all of these goals, whether you’re using relatively low-tech instruments or the latest in advanced measuring and marking systems.
Measuring: The Basics
While advanced technology can increase the precision of lens alignment, the basic equipment found in most practices can still do a good job. [For more on this, see “Toric Lenses: What’s Holding You Back?” on p. 28.] If you don’t have access to the latest advanced instrumentation, Robert H. Osher, MD, a professor in the department of ophthalmology at the University of Cincinnati College of Medicine and medical director emeritus at the Cincinnati Eye Institute in Ohio, recommends relying on three basic instruments. “Everyone can do manual keratometry,” he notes. “Today, the majority of cataract surgeons also have an automated keratometer—either IOLMaster or LenStar. Everybody should also have a topography unit. That’s important because you need to see what kind of cylinder you’re dealing with, so you can differentiate keratoconus or some irregular contact lens problem from regular cylinder. Of course, the presence of an unusual finding doesn’t mean you’re not going to offer a toric lens, but it certainly means that you have to explain the situation to the patient.”
 |
| The Verion’s toric IOL guidance overlay, with the target axis set at 95 degrees. The toric IOL would be rotated to align with this 95- degree guide, with no need for ink marks. |
Stephen S. Lane, MD, medical director at Associated Eye Care and adjunct clinical professor of ophthalmology at the University of Minnesota in Minneapolis, says your axis determination should be reasonably accurate if you use an automated keratometer and topography. “Primarily, you have to begin with good preoperative keratometry readings,” he says. “A number of devices can give you that; even manual keratometry can give you good, reproducible data if you have someone who is very good at performing it. But today, I think most doctors are using an IOLMaster or LenStar to determine these measurements.” Topcon’s Aladdin and Movu’s Argos are other options surgeons can use for biometry.
“Topography is probably the best technology we have today to measure the axis,” Dr. Lane adds. “The axis of astigmatism should correlate quite nicely with the automated keratometry readings that you would get with an IOLMaster or LenStar, assuming that you’re measuring a relatively normal, healthy cornea. They won’t necessarily agree exactly, but they should be very close. Then, you can use all of the various readings to hone in on what is the most likely—or at least the average—keratometry reading. The more readings you have, the better your result. In most cases I rely on automated keratometry for magnitude; I believe topography is probably the most accurate and sensitive in terms of the axis.”
 |
More Data = Greater Accuracy
Dr. Osher explains that measuring with multiple technologies helps to eliminate outlier measurements. “All of the machines measure slightly differently,” he notes. “A study we published looked at the question of how much your accuracy improves if you measure with more than one instrument and ‘meld,’ or average, the numbers.1 After testing 87 eyes of 54 patients we found that if you only measure with one technology, the number you end up with will be an outlier about 20 percent of the time. If you measure with two technologies, that drops to 8 to 10 percent. But if you use three technologies, only about 2 percent of the numbers you end up with are outliers. Everyone does manual keratometry, and everyone should do an automated K. In addition, you should get topography, because you need to understand what the astigmatism pattern looks like.”
Although the basic gear found in most practices today can do a good job of determining the target meridian and amount of astigmatism, there’s no question that having additional advanced technology can increase your accuracy. Dr. Osher has access to multiple technologies and takes full advantage of them.
“Because I’m somewhat of an academician and I love technology, I collect additional measurements with other devices,” says Dr. Osher. “I measure with the iTrace because I want to see the aberrometry and those Ks. I use the Pentacam because I want to measure the posterior cornea. And I have the luxury of using both the IOLMaster and the LenStar, so I end up with six sets of Ks for every patient. Of course, I would never recommend that every ophthalmologist do this, because the extra work and expense would convince many surgeons not to offer toric lenses. But I want to see all of those measurements because I think they’re important. They improve my understanding and increase my confidence.
“When I average all of these measurements together, it’s amazing how consistent the numbers are,” he says. “If one measurement is an outlier, I throw it out, but I usually get very good consistency on both the meridian and the amount of cylinder. Furthermore, if more than one reading is an outlier, then I check the topography for warpage or tear-film integrity, or search for some other problem. The patient may not be an ideal candidate for a toric lens, and needs to be told.”
Marking, from Ink to High-tech
Once you’ve decided on the target meridian, you have to use some form of guidance that will allow you to align the IOL along that meridian. The least expensive and most common (and arguably least accurate) method is to place ink marks on the cornea. “We all know that ink diffuses, and in the worst-case scenario it disappears completely,” says Dr. Osher. “Even with accurate marking, ink marks are often 5 or 10 degrees off, and every degree away from the target meridian eliminates about 3.3 percent of the effect of the toric lens. That’s why I developed the Thermodot device, which will finally be released this year by Beaver-Visitec International [Waltham, Mass.]. It makes a tiny pinpoint cautery mark that eliminates the need for ink. The mark is so small it isn’t even felt by the patient, and it’s gone in a day or two. To become even more accurate, I’d suggest iris fingerprinting, which is very inexpensive compared to aberrometry or the sophisticated registration methods. You use a camera to take a picture and then very inexpensive software tells you at which degree each iris landmark is located.”
Dr. Lane notes that you’re likely to achieve the greatest accuracy of alignment with toric IOLs when using a guidance system such as Verion, Callisto or the TrueVision system. “With those technologies, you’re trying to align the lens inside the eye relative to a fine line, as opposed to an ink mark. [Despite its drawbacks,] an ink mark can be fairly accurate—that’s what we used in the initial [toric IOL] clinical trial, producing pretty good results. But since we’re trying to get as close as we possibly can to the correct axis, there’s no question that guidance technologies can give us greater accuracy.”
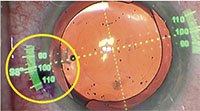
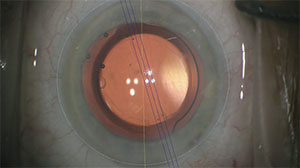
In addition to using Thermodots, Dr. Osher currently favors Zeiss’s Callisto Eye System for aligning his toric lenses. “It stores the original IOLMaster biometry measurements and memorizes the anatomy,” he explains. “When you’re in the OR, you turn on the Callisto Eye System monitor and it registers and links up the preoperative and live images. Then, you press a button and the axis appears in your ocular. It looks like a two-lane highway, making it very easy to align the lens. It’s simple, quick and accurate.” [See example on p. 32.]
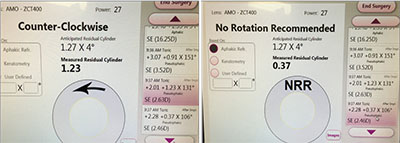 |
| An example of ORA intraoperative aberrometry screenshots during the alignment of a toric IOL. (The column on the right side of the screen shows the refractive cylinder with different alignments.) Left: With 1.23 D of measured residual astigmatism, the software recommends counterclockwise rotation of the toric IOL. Right: Slight counterclockwise rotation has resulted in a reduction of the astigmatism to 0.37 D and a determination of “no rotation recommended.” |
Intraoperative Aberrometry
Dr. Chang likes to use intraoperative wavefront aberrometry in addition to digital intraoperative axis alignment. “I use an aphakic reading with the ORA system (Alcon) to confirm the spherical and cylindrical IOL power and a pseudophakic reading to confirm the optimal toric IOL axis alignment,” he explains. “The latter is more accurate when the intraocular pressure is elevated with enough OVD to minimize speculum artifact, and with the accuracy of the Callisto system alignment, the confirmation is usually very quick if the preoperatively selected axis is correct.
“However, sometimes ORA directs me to rotate the toric axis either clockwise or counterclockwise until the intraoperatively measured astigmatism is minimized,” he notes. “I then use Callisto to re-mark the new optimal axis. After removing the OVD, Callisto then allows me to reset the toric IOL to the exact alignment that was confirmed by ORA to be optimal.
“Often,” he adds, “there is some disagreement between different preoperative diagnostic exams with respect to cylindrical power and axis. ORA serves as my tie-breaker in that case.”
Dr. Lane has also noted that using intraoperative aberrometry on the table when the patient is aphakic may produce a different axis reading than you’ll get preoperatively using a keratometer or even topography. “The question then becomes, what is the true axis?” he says. “To remove the lens, you’ve made some incisions in the cornea, and that could possibly alter the axis of astigmatism. Whether you should assume that the intraoperative aberrometry reading is more accurate depends, in part, on how much incision distortion you’ve created and how much you’ve hydrated the wound. If you’ve made large incisions and hydrated them a lot, you might get a better result by going with what the aberrometry tells you.
“In general,” he says, “I’ll go with the aberrometry reading if it disagrees with my preoperative K-readings. But again, there’s a little bit of an art to this; it’s not pure science.”
Of course, these advanced technologies, whatever their advantages, come at a significant cost. Dr. Chang, however, believes that the cost of the additional equipment is worth it, especially if multiple surgeons can use it. “Add up all the patients who will have their astigmatism managed at your ASC over the next 10 years,” he says. “It’s easy to justify the capital cost because of the surgical workflow efficiency you gain and the refractive premiums that patients pay to get the best outcomes.”
Aligning the Lens
Once you’ve settled on a method to display the target meridian, the last step is to align the lens and get it to remain in the position you’ve placed it. Dr. Osher says a big part of that process is managing your OVD removal correctly. “Once I put the lens in, I’ll rotate it clockwise until it’s a little short of the target meridian,” he says. “Then I go behind the optic with the I/A tip and I remove my Healon5, which I like to use because it’s so cohesive; I can easily remove it from behind the lens without affecting the Healon in front of the lens. I always take out the OVD behind the lens before the final alignment, because if I take it out afterwards it can cause the lens to move.
 |
| An example of a Callisto overlay during implantation of a toric IOL. The single yellow line marks the 180-degree axis; the three parallel blue lines show the 15-degree target meridian. |
“Next, I inject more OVD into the bag in front of the lens,” he says. “That expands the bag so the lens will rotate more easily; you don’t want the bag to be loose and have the chamber shallowing. Now the lens will be pressed against the posterior capsule, with no OVD left behind it.
“Next I turn on my Callisto Eye system,” he continues. “I rotate the lens to my Thermodots, the two little cautery marks, and the Callisto Eye system confirms that the alignment is dead-on. Because of the expanded bag, the lens rotates very easily with the silicone tip of the I/A hand piece placed in the optic-haptic junction. It’s easy and atraumatic.”
Dr. Osher says that before removing the last OVD, he makes sure the lens is centered and perfectly coaxial. (He notes that the stereo coaxial illumination provided by his Lumera microscope makes it easy to confirm the centration.) “I hydrate the incision before removing the final bit of OVD—something most surgeons don’t do—to ensure that the chamber won’t shallow, which would allow the lens to rotate,” he says. “Then I take out the OVD that’s in front of the optic. As I come out, I always have a second cannula in the stab incision through which I’m injecting fluid to keep the chamber deep. Between hydrating the incision ahead of time and having that second cannula, the chamber stays nice and deep, and the lens alignment doesn’t change. Once the OVD is out, I hydrate again and make sure the incision is watertight. Then I check my alignment one more time, adjust the pressure, and I’m done.”
Dr. Osher notes that some surgeons like to put in a little Miochol near the end of the procedure. “Doing that makes the enlarged pupil smaller and lets you be sure the lens is centered,” he says. “However, with a toric lens I wait until the very, very end because I don’t want the pupil to come down and obscure my view of where the guiding dots are, so I maintain maximum pupil dilation until the surgery is over. At that point I may put in a little Miochol to confirm that I’m perfectly centered as the pupil comes down. This is particularly important with multifocal torics, which we now have in the United States.”
Dr. Lane adds that surgeons shouldn’t be put off by concerns about postoperative rotation. “Today’s toric lenses are quite stable, with low rates of rotation and movement,” he says.
Measurement Pearls
These strategies can help ensure that you get the best possible outcomes:
• Watch out for simple, avoidable errors. “A number of potential errors can lead to incorrect toric IOL axis alignment,” notes Dr. Chang. “The first—and least apparent to the surgeon—is the staff failing to carefully level the patient’s head during the keratometry and topography measurements. The second potential problem is a transcription error made when going from the diagnostic machine to the operating room, such as writing 10 degrees as the operative axis instead of 110 degrees. The third potential error is mis-identifying the 180-degree axis when the patient is supine with ocular cyclotorsion; preventing this requires marking the patient while sitting upright in the preoperative area. The fourth potential source of error is during the marking of the intended toric IOL axis using a degree gauge and an ink pen, given the propensity for the ink mark to bleed, fade or smudge.
“Some of these errors are additive,” he points out. “For example, the 180 axis may be a bit off while marking the upright patient, and then the ink pen mark may be 5 degrees wide. This can lead to a 10-degree misalignment on the operating table.”
• Make sure that experienced technicians are taking the measurements. “Your results will only be as good as the talent of the individuals who take the measurements,” says Dr. Osher. “Experienced technicians will make sure the head isn’t tilted and the cornea isn’t bone-dry, among other things.”
• Disregard subjective measurements of the axis. “The axis you get from a refraction isn’t reliable,” notes Dr. Osher. “Also, disregard any cylinder in the patient’s glasses, unless the patient has high cylinder. For example, if the patient has 3 D of cylinder in her glasses, I would use that as an extra measurement. However, if the patient has 1 D, it means nothing; it could be the crystalline lens that’s creating that cylinder.”
High-tech Pearls
If you’re able to access some of the more advanced technologies, these strategies are worth keeping in mind:
• If possible, measure the posterior corneal surface. Dr. Osher points out that a truly accurate determination of the toric meridian must take into account the astigmatism caused by the posterior cornea. “There are four technologies that can measure that,” he says. “Douglas Koch, MD, who first pointed out the importance of this factor, did his pioneering work on Ziemer’s Gallilei. A lot of us have used the Pentacam; the Cassini and Opto-Vue also measure the posterior cornea.
“Rather than measuring it, many surgeons who want to take this into account simply use an average of 0.3 D of posterior against-the-rule astigmatism,” he continues. “This is the correct average, but after Dr. Koch alerted us to the importance of this factor, I spent several years measuring the posterior cornea on every patient. I found that the astigmatism caused by the posterior surface ranges from 0 to 0.8 D. That’s a whole step on a toric lens.”
Dr. Osher says taking posterior corneal astigmatism into account isn’t difficult. “The posterior axis is always against-the-rule,” he says. “So, if the patient has against-the-rule cylinder on the front of the cornea, with the steep axis at 180 degrees, you add the posterior corneal astigmatism. For example, if the patient has 1 D of cylinder at 180 degrees, and the posterior cornea has 0.5 D of cylinder, then you need to correct 1.5 D of cylinder overall. On the other hand, if the patient has with-the-rule cylinder, you subtract it. For example, if the patient has 1 D of with-the-rule cylinder at 90 degrees, and the posterior cornea measures 0.5 D, you would subtract the 0.5 D, meaning the patient actually has 0.5 D of astigmatism overall. This patient is not even a toric candidate. Finally, if the anterior astigmatism is oblique, it’s a vector case, and I pay attention to the IOL recommended by the Barrett toric calculator.
“Some might say that this is a minor point—like worrying about your luggage when you’re on the Titanic,” he continues. “But the way I look at it, we should always do the very best we can for each of our patients. To accomplish that, we should always measure both the anterior and posterior cornea.”
• If possible, measure the entire optical system to see where the astigmatism is located. Dr. Osher uses the iTrace for this purpose. “I always look at the two possible sources of the astigmatism—the cornea and the lens,” he says. “There are three possible scenarios. Usually the astigmatism is in the cornea. Rarely—but it does happen—the astigmatism originates in the lens. The patient may have been wearing astigmatic correction and been referred in for a toric lens, but in this case you may be able to tell the patient she doesn’t need a toric lens. Once the cataract is removed the astigmatism will be gone. Patients love that. I show them the iTrace readout, and they can see the corneal and lenticular astigmatism.
“The third scenario is the most interesting,” he continues. “That’s a person who has never worn glasses. This individual may have with-the-rule cylinder in the cornea that’s been neutralized by against-the-rule cylinder in the lens. I tell them, ‘After we take out your cataract you’re going to have a lot of astigmatism, so you’re a good candidate for a toric lens.’ They say, ‘Wait a minute, why are you trying to sell me a toric lens when I’ve never worn glasses?’ I show them the iTrace measurements so they understand that once we take away the lens, they’ll suddenly have a problem with residual astigmatism. This situation isn’t common, but it definitely does happen.”
Dr. Osher notes that this supports the value of taking multiple measurements. “Multiple measurements help you eliminate outliers, but they also provide additional information,” he says. “Even though the amount of testing I do sounds excessive, the tests all help me gain greater understanding about my refractive cataract patient.”
• Even if you use advanced technology to align the lens, consider also marking the cornea. “I think it’s important to use a belt-and-suspenders approach,” says Dr. Osher. “The more approaches you use, the better, because something can always go wrong. If lightning hits the surgery center or the technology breaks down, you still have something to go by.”
Dr. Osher explains how he uses the Thermodot with iris fingerprinting. “I take a picture of the eye while the patient is at the slit lamp and I’m doing my dilated exam,” he says. “Inexpensive software identifies the location of key landmarks on that iris. In the OR I can put my cursor on whatever landmark I want and the software tells me what degree it’s at, so I always know exactly where I am. Then, if all of my sophisticated technology stops working—either because the machinery is temperamental, or something bleeds and I lose registration, or fluid from I/A gets under the conjunctiva causing it to balloon up—I have a simple iris fingerprint that tells me exactly where to put my Thermodots, and the IOL will be accurately aligned.”
Dr. Lane says he no longer makes an ink mark, now that he uses the more advanced alignment tools, although he agrees that there’s nothing wrong with doing so as a failsafe. “To me, not having to do that is one of the advantages of using a guidance system,” he says. “If the power went out, I could always sit the patient up, mark the eye and lay the patient back down, but that hasn’t happened to me since I’ve had these instruments.”
The Wave of the Future?
“There’s no question that implanting toric lenses adds surgical time, and some pre-surgical discussion has to take place to ensure that patients have realistic expectations,” Dr. Lane admits. “But current toric lenses are excellent, regardless of which manufacturer’s lens you use. Meanwhile, the advanced alignment technology that’s available will improve your results. I think the investment is worthwhile, especially in groups that have multiple surgeons doing cataract surgery, so that the surgeons can share in the expense of these instruments up front. The bottom line is that surgeons who are willing to do toric lenses will be very satisfied with the results, and they’ll have a much larger group of happy patients.”
Dr. Osher agrees. “I’m convinced that one day toric lenses will be the standard of care,” he says. REVIEW
Dr. Osher is a consultant to Zeiss, Alcon, BVI and Clarity. Dr. Chang is a consultant for Clarity and Zeiss; he has no financial interest in Alcon or ORA. Dr. Lane is a consultant for Alcon.
1. Browne AW, Osher RH. Optimizing precision in toric lens selection by combining keratometry techniques. J Refract Surg 2014;30:1:67-72.



