FDA Indications
Phase III studies have found cyclosporine A to be both safe and effective in the treatment of moderate to severe dry-eye disease.
One Phase III study compared the efficacy and safety of cyclosporine A 0.05% and 0.1% ophthalmic emulsions to vehicle in patients with moderate to severe dry-eye disease.1 This randomized, multicenter, double-masked study included 877 patients with moderate to severe dry-eye disease. Patients were treated twice daily with either cyclosporine A 0.05% or 0.1% or vehicle. Treatment with both concentrations of cyclosporine provided significant improvement compared to vehicle in corneal staining and categorized Schirmer values. Additionally, cyclosporine 0.05% treatment also provided significantly greater improvements in three subjective measures of dry-eye disease compared to vehicle: blurred vision, need for concomitant artificial tears, and the physician's evaluation of global response to treatment. There was no dose-response effect, and both cyclosporine A treatments exhibited an excellent safety profile, with no significant topical or systemic adverse safety findings.
 |
| Figure 1. Fungal infection in a corneal transplant patient. |
A separate Phase III study evaluated the safety of cyclosporine 0.1% ophthalmic emulsion over a one- to three-year period in moderate to severe dry-eye patients.2 This was a nonrandomized, multicenter, open-label clinical trial that included 412 patients who were previously dosed for six to 12 months with cyclosporine 0.05% or 0.1% in prior Phase III trials. Patients instilled ophthalmic cyclosporine 0.1% twice daily into both eyes for up to three consecutive 12-month periods. The study found that cyclosporine 0.1% ophthalmic emulsion taken for one to three years was safe and well-tolerated and was not associated with systemic side effects.
"These results supplement the safety record of the commercially available cyclosporine 0.05% ophthalmic emulsion," says Stephen C. Pflugfelder, MD, one of the study's authors. Dr. Pflugfelder is a professor of ophthalmology at Baylor College of Medicine in Houston.
Adds Eric D. Donnenfeld, MD, an associate professor of ophthalmology at New York University Medical Center, New York City, "The FDA studies have shown that this is an extraordinarily effective drug for treating patients who don't make enough quality tears. These studies showed that 15 percent of patients who were given Restasis had a tripling of their Schirmer scores."
Moreover, a study conducted by Karl Stonecipher, MD, and colleagues found that it is an effective treatment for patients suffering from severe dry eye.3 The study included 4,504 ophthalmologists, optometrists and primary care physicians from across the United States. Data were obtained from patient surveys that included questions related to patients' experiences using topical cyclosporine A 0.05% ophthalmic emulsion. A total of 5,884 patients completed the study, and the vast majority of patients were women. Patients who completed the study achieved significant reductions of 30 percent in symptom severity and 31- to 36-percent reductions in activity impairments relative to baseline. Onset of relief was noted within one week by 32 percent of patients and within three weeks by 73 percent.
"These were mild to severe dry-eye patients who typically presented with dry-eye-related complaints," says Dr. Stonecipher, who is in private practice at the TLC Eye Center in Greensboro, N.C. "The most notable difference between this study and the FDA studies is the rapidity of response. I attribute that to the fact that those patients who were initially enrolled in the FDA studies were the severe dry-eye patients in whom nothing else worked, as opposed to the general dry-eye patient seen in day-to-day practice."
Non-FDA Indications
One of the main off-label uses of Restasis is for the prevention and treatment of post-LASIK dry eye, according to Dr. Donnenfeld. He pretreats all patients with mild to moderate dry eye before LASIK. Restasis not only improves the symptoms of dry eye after LASIK, but it can also improve visual acuity results after LASIK. "The ocular surface is more regular, and patients achieve better quality of vision with reduced glare and halo," he says.
 |
| Figure 2. Various cases of meibomian gland dysfunction. |
A recent masked study included 42 eyes of 21 myopic dry-eye patients who were considered poor candidates for LASIK.4 They were randomly divided into two treatment groups. One group received unpreserved artificial tears, and the other group received Restasis. The drop was discontinued for 48 hours postoperatively and was then resumed for three additional months. The eyes that received Restasis had significantly better postoperative uncorrected visual acuity at one month and in many cases at one year. Additionally, the one-week best-corrected visual acuity was better in the Restasis group, and it appeared that these eyes were recovering faster.
Dr. Stonecipher also recently reported that Restasis in LASIK patients with chronic dry eye produced improvement in patient symptoms post-LASIK and decreased the impact of dry-eye symptoms on patients' daily activities. (Stonecipher KG, McMackin N. Onset of symptom relief in chronic dry-eye patients after treatment with cyclosporine 0.05% ophthalmic emulsion. Presented at the 2005 American Society of Cataract and Refractive Surgery Annual Meeting.) In this study, the majority of patients noted relief of their symptoms within three weeks and a reduction in concomitant artificial tear use.
According to Dr. Pflugfelder, one of the most effective off-label uses of Restasis is for the treatment of allergic-type conditions. "Patients with eczema or atopic dermatitis can get very severe conjunctival and corneal inflammation. Restasis works extremely well for these patients," he says.
A recent study found that topical cyclosporine A 0.05% is safe and effective in alleviating signs and symptoms of severe atopic keratoconjunctivitis refractory to topical steroid treatment.5 In this study, 22 patients with atopic keratoconjunctivitis were randomly assigned to receive topical 0.05% cyclosporine A eyedrops or placebo for a period of 28 days six times daily during the first two weeks and then four times daily during the last two weeks. The study found that cyclosporine A had some effect in alleviating the signs and symptoms of severe atopic keratoconjunctivitis.
 |
| Figure 3. Restatis use may help a patient with Thygeson"s keratitis avoid corticosteriods and their attendant risk of cataract. |
Dr. Pflugfelder noted that Restasis is also effective in treating vernal keratoconjunctivitis. "This type of allergic and inflammatory-mediated keratoconjunctivitis typically occurs in young males. It can be severe and blinding," he says.
He noted that Restasis is a better choice than steroids for treating both atopic keratoconjunctivitis and vernal keratoconjunctivitis because the conditions are chronic and may last for years. "These patients would require very frequent steroid drops, sometimes four times a day, to control the disease, so they are prone to developing steroid complications, such as cataract, glaucoma or infections. Restasis is an extremely safe medication that can be used chronically," he says.
Another off-label use is the prevention of corneal transplant rejection. In these cases, Restasis is used as a steroid-sparing agent or as a supplement to steroids. "Transplant rejection is mediated in large part by T-lymphocytes, which are the master immune-regulating cells in the body. Cyclosporine is a potent inhibitor of T-lymphocytes, and it prevents their activation," Dr. Pflugfelder explains.
It is also effective for managing post-corneal transplant glaucoma, according to Dr. Donnenfeld, who published a paper on this topic.6 Many times, the glaucoma is induced by corticosteroids. "In patients who have glaucoma after a corneal transplant, if we take them off their steroid and put them on Restasis, they have a significant reduction in pressure," he says. In fact, these patients have a mean intraocular pressure decrease of 8.2 mmHg.
According to Henry D. Perry, MD, Restasis can also prevent a phakic corneal transplant recipient from developing cataracts. "This is especially useful in patients who are young and who have keratoconus, says Dr. Perry, an associate clinical professor at Weill Medical College. "Restasis protects their corneas and prevents the problems that can occur with long-term use of corticosteroids, in terms of cataracts and secondary glaucoma."
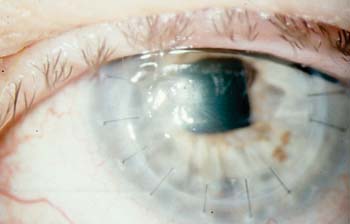
Drs. Donnenfeld and Perry have also found Restasis to be helpful in the treatment of fungal infections in keratoplasty patients (See Figure 1). (Perry HD, Donnenfeld ED, Kornstein H, Kanellopoulos AJ. Topical cyclosporine A in the management of therapeutic keratoplasty for mycotic keratitis. Presented at the 1999 American Academy of Ophthalmology Annual Meeting.)
"We use it in conjunction with nonsteroidals in an effort to avoid corticosteroids postoperatively," Dr. Perry says. "This is important because steroids postoperatively potentiate fungal overgrowth and may enhance the likelihood of a fungal recurrence. Therefore, by avoiding corticosteroids, we improve the prognosis for our patients that the keratoplasty will be successful, both in terms of clarity and, most importantly, eradicating the fungal infection."
In addition to aqueous-deficient dry eye, Restasis also effectively treats meibomian gland dysfunction (See Figure 2).7 In a prospective study, 33 patients with meibomian gland dysfunction were randomized to receive either Restasis or placebo twice daily for three months. They were evaluated at baseline and at the end of each month for subjective symptoms and objective signs, including meibomian gland inclusions, lid margin vascular injection, tarsal telangiectasis, fluorescein staining, tear breakup time, and Schirmer scores.
The study found that, at the three-month visit, several objective examination findings were statistically significantly improved in the Restasis group compared to placebo. These differences included lid margin vascular injection, tarsal telangiectasis, and fluorescein staining. The most significant finding was the greater decrease in the number of meibomian gland inclusions in the Restasis group, Dr. Donnenfeld says.
He notes that Restasis is also effective for the treatment of inflammatory corneal ulceration, rheumatoid corneal ulcers, pauciarticular juvenile rheumatoid arthritis, iridocyclitis, and ligneous conjunctivitis.
According to Dr. Pflugfelder, Restasis is also effective for certain types of superficial keratitis that typically occur after conjunctivitis. He says that superficial keratitis can occur as early as two weeks after the conjunctivitis and can last for months or years. Because it can be chronic, Restasis can be a better treatment choice than steroids.
Thygeson's superficial punctate keratitis has a similar appearance, and its cause is unknown (See Figure 3). Restasis is a good choice for these patients because many are very young, and corticosteroids can cause a cataract if they are used often enough. Children are more at risk for cataracts just because of their age and their life expectancy.
Drs. Donnenfeld and Perry also published a study showing that Restasis is helpful as primary or adjunctive therapy for superior limbic keratoconjunctivitis.8 "We use it as a treatment for these patients and also to help maintain them in a state of relative quiescence. In this way, we avoid the use of long-term corticosteroids," Dr. Perry says.
Their study included five patients diagnosed with Theodore's superior limbic keratoconjunctivitis. Topical cyclosporine A 0.5% drops were used four times daily in both eyes. All five patients had long-term improvement of irritation and foreign body sensation, as well as improvement of injection and filamentary keratitis. Except for burning on instillation, there were no complications related to this therapy.
Dr. Pflugfelder also uses Restasis in patients with herpetic stromal keratitis.
"I also use it prophylactically in patients with Hashimoto's thyroiditis," Dr. Perry says. "These patients have a 20- to 45-percent chance of developing keratoconjunctivitis sicca. With this high likelihood, using Restasis in a prophylactic way is beneficial and justifiable," he says.
The Future of Restasis
Because Restasis is a T-cell modulator, any patient with a T-cell-mediated disease will benefit from its use, and Restasis has several benefits over steroids:
• It inhibits T-lymphocytes.
• It causes no increase in IOP.
• It causes no decrease in wound healing.
• It does not inhibit the phagocytic system.
• It does not cause cataracts.
• It has no effect on viral replication.
• It improves tear function.
"There are opportunities for its use that we haven't even explored yet," Dr. Donnenfeld says. "As our comfort with cyclosporine increases, new indications for its use will be elucidated. Its unique combination of a high therapeutic efficacy and specific T-cell modulation without affecting the inflammatory pathways makes it a very low-risk drug for the treatment of these different diseases."
1. Sall K, Stevenson OD, Mundorf TK, Reis BL. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. CsA Phase 3 Study Group. Ophthalmology 2000;107:1220.
2. Barber LD, Pflugfelder SC, Tauber J, Foulks GN. Phase III safety evaluation of cyclosporine 0.1% ophthalmic emulsion administered twice daily to dry eye disease patients for up to 3 years. Ophthalmology 2005;112:1790-1794.
3. Stonecipher K, Perry HD, Gross RH, Kerney DL. The impact of topical cyclosporine A emulsion 0.05% on the outcomes of patients with keratoconjunctivitis sicca. Curr Med Res Opin 2005;21:1057-1063.
4. Salib G, McDonald M, Smolek M. Safety and efficacy of cyclosporine 0.05% drops vs. unpreserved artificial tears in dry eye LASIK patients. J Cataract Refract Surg In press.
5. Akpek EK, Dart JK, Watson S, et al. A randomized trial of topical cyclosporine 0.05% in topical steroid-resistant atopic keratoconjunctivitis. Ophthalmology 2004;111:476-482.
6. Perry HD, Donnenfeld ED, Kanellopoulos AJ, Grossman GA. Topical cyclosporine A in the management of post-keratoplasty glaucoma. Cornea 1997;16:284-288.
7. Perry HD, Doshi-Carnevale S, Donnenfeld ED, Solomon R, Biser SA, Bloom AH. Efficacy of commercially available topical cyclosporine A 0.05% in the treatment of meibomian gland dysfunction. Cornea In press.
8. Perry HD, Doshi-Carnevale S, Donnenfeld ED, Kornstein HS. Topical cyclosporine A 0.5% as a possible new treatment for superior limbic keratoconjunctivitis. Ophthalmology 2003;110:1578-1581.



