Gene Therapy
Identification of specific disease-associated genes using next-generation sequencing has made personalized medicine a reality for patients who suffer from congenital disorders. This year at ARVO, presentations focusing on personalized medicine were dominated by application of CRISPR/Cas9 technology. CRISPR, an acronym for “clustered regularly interspaced short palindromic repeats,” is a mechanism that allows for directed, specific splicing of a disease-associated gene, thereby removing the genetic identity of a particular condition.1 While the methodology holds great promise, technical hurdles remain, such as splicing the wrong gene, a problem that can be significant in some applications. Despite this, the promise of CRISPR was clearly seen in the explosion of presentations at this year’s ARVO.
| Meet David. A Hollander, MD |
| We wish to welcome David A. Hollander, MD, to the Therapeutic Topics family as a co-author of many upcoming columns. Dr. Hollander was recently appointed chief medical officer and senior vice-president of the pharmaceutical consulting firm Ora, which was founded by Dr. Abelson and whose writers help compose Therapeutic Topics each month. Prior to this new appointment, he oversaw therapeutics and served as vice president of clinical development at Allergan and was responsible for global strategy and clinical development programs in anterior segment ophthalmology and consumer eye care. In addition to his position at Ora, Dr. Hollander is on the faculty of the Jules Stein Eye Institute at the University of California, Los Angeles. His training and experience, as well as his ophthalmic and pharmaceutical acumen, represent a great addition to Ora and to Therapeutic Topics. Welcome, Dr. Hollander. —MBA |
One group investigated the use of CRISPR-based genomic editing for the treatment of CEP290-associated Leber congenital amaurosis. This study demonstrated that CRISPR-based genome editing deleted the most common human mutation in CEP290, suggesting a clinically meaningful way to restore CEP290 function without the risk of overexpression toxicity. (Stone E, et al. ARVO E-Abstract 1838) The use of CRISPR in the treatment of retinal degenerative diseases, such as retinitis pigmentosa, was also investigated. Researchers at the University of California, San Diego, developed genetically modified, human, induced pluripotent stem cell (hiPSC) retinal cell-reporters using CRISPR technology. Using this approach, the authors identified novel mechanisms of retinal development that potentially could increase the efficiency and pace of photoreceptor generation. (Wahlin K, et al. ARVO E-Abstract 2820) Look for an upcoming Therapeutic Topics to provide an in-depth look at CRISPR/Cas9 technology and its future in ophthalmology.
Many presentations focused on more traditional gene therapy using nonpathogenic viruses as delivery/vector systems (e.g., adeno-associated viruses or lentiviruses). Although this technique is technically challenging, a decade of research and development has yielded significant progress. A clinical study of RetinoStat (Oxford BioMedica), a lentiviral vector expressing endostatin and angiostatin, was one of this year’s many applications of viral-based gene therapy. (Lauer A, et al. ARVO E-Abstract 4719) The study was conducted by consultants and researchers from Oxford BioMedica. RetinoStat was administered subretinally to 21 patients with poor anti-VEGF response as a possible treatment for advanced neovascular AMD. The vector safely delivered the two transgenes and led to visual acuity stabilization and reduction of vascular leakage. In another presentation, intravitreal delivery of AAV-mediated expression of Stannicocalcin-1 (STC-1, Applied Genetics Technologies) delayed photoreceptor degeneration in two rodent models of retinitis pigmentosa; the researchers identified genes to investigate in future studies, mechanisms of action and the therapeutic potential of the approach. (One of the study’s researchers holds a patent on the therapy and consults for AGT.) (Roddy G, et al. ARVO E-Abstract 2737)
Stem Cell Biology
Stem cell technologies and applications were once again a popular topic at ARVO, with more than 150 posters and presentations covering developmental biology, cell fate regulation, novel stem cell markers and populations, and therapeutic applications. The focus of therapy included the corneal epithelium, stroma and endothelial layers; directed differentiation and transplantation of retinal cells; and even use of progenitor cells to understand congenital disorders.
A particularly popular topic was the therapeutic application of pluripotent stem cell-derived retinal pigment epithelium. One study showed that autologous, induced pluripotent stem cells can be successfully transplanted subretinally, and that the graft was well-tolerated a year after transplant. (Kurimoto Y, et al. ARVO E-Abstract 3769) Two studies took the allogeneic route and used RPE derived from human embryonic stem cells for the treatment of wet age-related macular degeneration (Yin Z, et al. ARVO E-Abstract 3742) or Stargardt’s disease. (Mehat M, et al. ARVO E-Abstract 3768) Both studies showed that the stem cell-based therapies were well-tolerated, leading the way to efficacy trials and, perhaps, successful treatments of these blinding diseases with stem cells.
Another hot topic in the stem cell field was the effect of stem cell secretory products and vesicles on cell differentiation and tissue repair. One study found that microvesicles secreted by hESC can induce de-differentiation and trans-differentiation in Müller cells. (Farber D, et al. ARVO E-Abstract 2821) Another group found that vesicles derived from human mesenchymal stem cells increased corneal epithelial cell proliferation, thereby promoting corneal wound repair and reducing corneal neovascularization. (Ritter T, et al. ARVO E-Abstract 3477) In a similar study, mesenchymal stem cells derived from bone marrow were shown to secrete factors that accelerate corneal epithelial wound healing, supporting the results of the previous study. (Eslani M, et al. ARVO E-Abstract 3478)
Dry-eye disease was another therapeutic target for stem cell treatment this year. There were two notable studies that used stem cells to either increase tear production or to regenerate tear-producing tissue. One study showed that intraperitoneal injections of bone marrow-derived mesenchymal stem cells increased tear production in a mouse model of Sjögren’s syndrome. (Aluri H, et. al. ARVO E-Abstract 4921) This suggests that mesenchymal stem cells may act at a distance to treat dry-eye syndrome. Another study combined mesenchymal stem cells with lacrimal gland epithelial cells and human endothelial cells to create a functional lacrimal gland. (Massie I, et al. ARVO E-Abstract 5223) The group showed that, in defined culture conditions, the cells organized to form secretory spheroids that may eventually be used to replace damaged lacrimal gland tissue, restoring tear production in patients with dry-eye syndrome.
Retina
It was not too many ARVOs ago that anti-VEGF technology was at the cusp of clinical approval, similar to today’s viral gene therapy. Now, anti-VEGF therapy is an established therapeutic approach with indications that continue to be expanded and refined.
Two presentations focused on switching treatment from ranibizumab to aflibercept. In one study, 26 patients with polypoidal choroidal vasculopathy who were previously refractory to ranibizumab received intravitreal injections of aflibercept. Visual acuity improved or was maintained for two years; however, subretinal fluid was still visible in approximately 30 percent of patients. (Kohno T, et al. ARVO E-Abstract 514) In a second Phase III multicenter trial of switching treatments, 82 wet AMD patients with RPE detachment who hadn’t responded to ranibizumab were switched to intravitreal injection of aflibercept. This treatment change appeared to be effective in reducing PED volume and height and in improving visual acuity. (Gallemore R, et al. ARVO E-Abstract 4986)
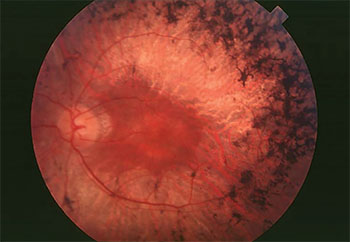 |
One of the primary targets for gene therapy is retinitis pigmentosa, a group of inherited diseases featuring hyperpigmentation of the retina and progressive loss of visual function. |
A different treatment target for aflibercept, in addition to VEGF-A, was identified in galectin-1, an angiogenic factor associated with proliferative diabetic retinopathy. In in vitro and in vivo studies, including eye tissue from PDR patients, aflibercept bound to and neutralized galectin-1. This activity was independent of VEGF binding, suggesting that aflibercept may also be effective as an anti-angiogenic treatment for PDR. (Kanda A, et al. ARVO E-Abstract 1352)
New alternatives to aflibercept and ranibizumab are on the horizon, and research continues on brolucizumab for neovascular AMD. A Phase III, international, two-year efficacy and safety study of approximately 1,600 patients, sponsored by Alcon, is ongoing. Alcon hopes that brolucizumab, which is smaller than other anti-VEGF molecules, may have a longer duration of effect than current anti-VEGF drugs, allowing for fewer injections, thereby reducing the treatment burden for patients. (Dugel P, et al. ARVO E-Abstract 5018)
While the potential of anti-VEGF treatments is impressive, some patients have a suboptimal response to anti-VEGF therapies or don’t respond to them at all. As a result, researchers are looking into other treatments targeting different pathways that may provide important complements to existing anti-VEGF approaches. Several presentations at this year’s ARVO focused on combination therapies. Some of these targeted wet AMD refractory to anti-VEGF treatment, and others were designed to improve the efficacy of anti-VEGF therapies. In a study of 10 patients with neovascular AMD, addition of topical dorzolamide-timolol therapy to anti-VEGF treatment significantly reduced macular edema and subretinal fluid. (Sridhar J, et al. ARVO E-Abstract 4441)
In another study of 24 wet AMD patients with suboptimal responses to prior anti-VEGF therapy, a combination of anti-angiopoietin (Ang2) monoclonal antibody (RG7716) and anti-VEGF was well-tolerated and improved best-corrected vision and optical coherence tomography parameters. This was one of the first efforts to use dual-action targeting of both VEGF and Ang2. (Chakravarthy U, et al. ARVO E-Abstract 4718) Another anti-angiogenic, VEGF-independent compound presented at ARVO, SH-11037, in combination with aflibercept, inhibited human retinal endothelial cell proliferation more than either treatment alone, suppressed CNV lesions in vivo and appeared to act synergistically. (Sulaiman R, et al. ARVO E-Abstract 1108)
A key objective of intravitreal therapy is to minimize the number of injections without compromising efficacy. One study examined this using staged combination anti-VEGF therapy (ranibizumab and/or bevacizumab) with a sustained-release corticosteroid (Ozurdex, Allergan) and optional laser treatment. One-year results in 90 subjects indicated that staged combination therapy was effective in treating retinal vein occlusion and related cystoid macular edema, with fewer injections needed over one year. Additionally, results indicated that disease severity was related to more frequent injections, that treating ischemia may enhance early disease stabilization and that early treatment of RVO before the development of CME might potentially halt disease progression and prevent complications. (Cikatricis P, et al. ARVO E-Abstract 4154)
A multicenter clinical trial of 106 patients with vitreomacular adhesion or vitreomacular traction investigated the safety and efficacy of Allegro Ophthalmics’ synthetic anti-angiogenic and vitreolytic oligopeptide, Luminate. Patients with VMA are at risk for progression to VMT and its potential consequences: retinal edema; bleeding; optic nerve damage; visual impairment and blindness. Sixty-five percent of patients treated with the highest dose of Luminate achieved release of VMA or VMT by day 90, compared to 10 percent in the placebo group. Pharmacological treatment of VMA or VMT could reduce the risks associated with surgical intervention (pars plana vitrectomy). (Kuppermann B, et al. ARVO E-Abstract 1809) Another VMT study of 113 subjects compared three non-surgical treatments, C3F8 gas, SF6 gas and intravitreal ocriplasmin, with follow-up of more than six months. C3F8 gas injection showed superior VMT release rates compared to SF6 and IVO treatments. (Steinle N, et al. ARVO E-Abstract 1806)
Dry AMD is the most common type of macular degeneration and, unfortunately, there are no pharmacological treatments currently available for it. In one study, however, a prosthetic implant placed within regions of geographic atrophy in late-stage dry AMD patients achieved successful integration of artificial (central) and natural (peripheral) vision. Surgeons implanted the Argus II electronic epiretinal prosthesis in four patients with subfoveal GA that severely affected their central vision. At follow-up (0.2 to 5.6 months), all of the patients showed central visual function elicited by the implant. (Stanga P, et al. ARVO E-Abstract 3733) In a related approach, surgeons implanted a prosthesis in three patients with advanced retinitis pigmentosa. After one year, this suprachoroidal-transretinal stimulating prosthesis elicited phosphenes in all three patients. Researchers observed the greatest improvements in visual tasks in patients with the electrode array implanted closer to the fovea centralis. (Fujikado T, et al. ARVO E-Abstract 5203)
In another study, investigators used quantitative spectral-domain OCT to develop a predictive model of GA designed to identify regions where GA is likely to appear in the future. They used scanning data to develop a statistical model that may eventually be used in clinical care, and as a biomarker for drug efficacy and device studies. (Leng T, et al. ARVO E-Abstract 1802)
Presbyopia
Current estimates project that around 1.8 billion people will be affected by presbyopia by 2050. With this staggering statistic, it’s not surprising that the condition was a dominant topic at this years’ ARVO. Treatments currently available for presbyopia include the use of reading glasses, contact lenses or refractive/intraocular lens surgery. Lens wear is the most widely used option for treatment, despite the fact that lenses can have a limited field of view and/or cause severe distortion, the latter of which can cause discomfort or dizziness when wearers use different parts of the lens for various visual tasks. Although pharmaceutical therapies have been explored, thus far all of them have been limited in their treatment of the condition and have had some undesirable adverse effects.
Since presbyopia is a condition associated with aging in which the eyes lose their ability to adjust their focal length in order to produce focused images of near objects on the retina, one study investigated several important lens parameters in an attempt to further understand the role of the lens in accommodation. (Martinez-Enriquez E, et al. ARVO E-Abstract 1380) More precise estimates of geometrical parameters of the whole lens may be important for providing better IOL selection and customization of premium presbyopia correction solutions.
Presbyopic patients are not able to accommodate to see near objects but usually exhibit almost intact convergence and near-pupil response capabilities. Researchers capitalized on these characteristics by designing a device in which the optical power of optoelectronic lenses was driven by the size of the subject’s pupils. (Mompean J, et al. ARVO E-Abstract 1816) In a controlled experimental setting, this system was successful in providing real-time focused images for objects placed at a variety of distances for presbyopic subjects.
Another group proposed a different approach to lens design for presbyopia treatment through a new design concept: harmonic diffractive liquid crystal lenses. (Guoqiang L et al. E-Abstract 1818) Today, switchable electro-optic LC lenses offer a possible solution for presbyopia by overcoming the shortcomings of current therapies. However, developing LC lenses with high optical quality is difficult to achieve, since LC lenses can’t provide the aperture and power needed for spectacle lenses. This group demonstrated that harmonic diffractive LC lenses can accomplish vision correction that’s not possible with conventional diffractive LC lenses, thereby providing a promising new therapy for the correction of presbyopia.
Allergy and Dry Eye
Although it’s more of a niche market now at ARVO, the allergic conjunctivitis session remains near and dear to our therapeutic hearts.
The prominent role of the interleukins in allergy was the subject of several presentations. IL-33 was shown to have a significant role in an animal model of ragweed conjunctivitis. The discovery of type 2 innate lymphoid cells in the lacrimal glands prompted one group to investigate whether these cells were responsible for the IL-33 and eosinophil infiltration seen in their allergic model. It turns out that the lacrimal gland isn’t the repository of these cells, since excision of the glands didn’t alter the course of the IL-33 mediated ragweed conjunctivitis. (Asada Y, et al. ARVO E-Abstract 306)
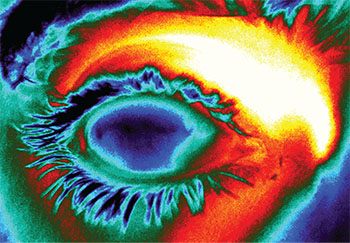 |
Thermal imaging of the ocular surface. Subtle differences in temperature can provide clues to the stability of the tear film and the underlying etiology of dry eye. (Sundstrom C, et al. ARVO E-Abstract 2851) |
The roles of the adaptive immunity and innate lymphoid populations were also studied in a mouse model of chronic and severe allergic inflammation. Immuno-phenotyping of the innate lymphoid population in conjunctival cells identified predominantly CD45+, CD3-, B220-, CD11b- and GR-1 cells. As clinical signs of ocular allergy intensified, the collective number of these cells increased more than fivefold. All three of the innate lymphoid populations within this pool, which included Tbet+, GATA3+ and RORγt+ cells, appeared to increase in the conjunctiva by differing amounts. (Smith R, et al. ARVO E-Abstract 311)
A different model of allergic conjunctivitis using a papain-soaked contact lens was used to study a variety of Th2 cytokines in knockout mice. IL-4-knockout mice had greatly reduced eosinophils compared to IL-13- and IL-5-knockout mice. Furthermore, IL-33-knockout mice had greatly reduced numbers of basophils, clearly indicating the differential mediation of cellular chemotaxis in allergic tissue. (Sugita et al. ARVO E-Abstract 304)
In conjunctival impression cytology samples from vernal keratoconjunctivitis and normal subjects, three- to twentyfold increases in RNA expression were demonstrated in Th2 cytokines (IL-4, -5, -9, -13, -23), chemokines (CCL13, -18, -24 and others), and adhesion molecules. Many others were downregulated, including the cytokine precursors activating enzyme caspase 1, and toll-like receptor 5. (Leonardi A, et al. ARVO E-Abstract 302) The ability to profile RNA from clinical ocular surface samples should allow us to home in on the mechanisms of allergic disease more easily and precisely.
Immunomodulatory agents are still the subject of clinical and preclinical investigation; for example, intraperitoneal, but not topical, sirolimus showed efficacy in a mouse allergy model. (Wang N, et al. ARVO E-Abstract 309) One novel therapy described was Nasapaque, an iodinated contrast agent from 3E Therapeutics Corp. Researchers tested Nasapaque for the relief of nasal and ocular itching induced by allergen exposure in the Ora Allergen Biocube chamber. Positive results provided further evidence of the neuronal nasal-ocular reflex for ocular itching. (Gomes P, et al. ARVO E-Abstract 305) Similar cross-talk was shown by a high, 82-percent incidence of itchy palate across five clinical trials using conjunctival allergen challenge, with 38 percent of subjects experiencing moderate to severe symptoms. (Schoemmell E, et al. ARVO E-Abstract 310) Using this same technology, Ocular Therapeutix researchers compared the pharmacokinetics of cyclosporine to Restasis in a canine model, (Smoot D, et al. ARVO E-Abstract 423) and tested a similar technology using intravitreal hydrogel depots for sustained release anti-VEGF in a rabbit model. (Blizzard C, et al. ARVO E-Abstract 1120)
Gap junctions, which are large, non-selective membrane channels connecting the cell cytoplasm to the extracellular milieu, were the subject of a mini-symposium at this year’s ARVO, with a focus on connexin 43 function in the cornea and retina. In the eye, hemichannels assemble to form a gap junction. The hemichannel has been referred to as a pathological pore, and is a key component in the inflammasome pathway during both its initiation and propagation. Under injury and disease conditions, both connexin 43 expression and hemichannel permeability are increased, and therapeutic connexin 43 modulation has resulted in sight-saving outcomes in humans with persistent trabeculectomy scarring or severe ocular surface burns. Along these lines, speakers at the mini-symposium discussed pathological roles of connexin hemichannels in ocular injury and their potential as intervention sites. Studies discussed during the mini-symposium employed a variety of models, including a rat cornea keratectomy model, a rabbit trabeculectomy model, a bright light retinal injury model and a rat retinal-ischemia reperfusion model, to demonstrate the general importance of this cell constituent. Data from these studies were correlated with ex vivo human donor tissue analysis and suggest that loss of vascular integrity may be a common component in ocular disease. We look forward to following the progress of hemichannel modulation as a therapeutic means of protecting the eye from injury in multiple pathologic settings.
Another common theme was recent advances in the science of aging, including studies of central nervous system neurodegeneration, age-related changes in the RPE, the influence of aging on the immune system, epigenetic changes with age and oxidative damage in the retina. Concepts discussed this year included autophagy and mitophagy, homeostatic processes that clean up degraded or damaged mitochondria and other cell components. These processes are key to neuronal health and can go awry and lead to autophagic “traffic jams” in diseases involving retinal degeneration such as AMD, (Ferrington D. ARVO E-Abstract 5650) and in glaucoma (Liton P. ARVO E-Abstract 5651) and corneal dystrophies. (Kim E. ARVO E-Abstract 5652)
Para-inflammation is a low-level immune activation stimulated to maintain homeostasis and restore functionality in chronic stress conditions such as diabetes. (Xu H. ARVO E-Abstract 1398) The innovative view is that para-inflammation may be beneficial, and different from detrimental chronic inflammation that leads to diseases such as AMD. This discussion circles back to autophagy in that oxidative stress leads to an imbalance between production of damaged cellular components and degradation, leading to accumulation of detrimental products such as intracellular lipofuscin and extracellular drusen. Autophagy is the central lysosomal clearance system that may play an important role in AMD development. (Kaarniranta K. ARVO E-Abstract 1400)
Therapies impacting these age-related defects include SkQ1, a novel antioxidant that accumulates in mitochondria where it’s reduced and regenerated, making it a potentially effective target for the treatment of the many diseases of oxidative stress. In an anterior chamber paracentesis rabbit model, topical application of SkQ1 demonstrated a significant reduction in fibrin and flare reactions. (Belen L, et al. ARVO E-Abstract 5414) SkQ1 was also shown to significantly enhance corneal wound healing in vitro, through enhancement of cell proliferation and migration. (Wei Y, et al. ARVO E-Abstract 1255)
Dry-eye sessions featured several related themes; there was the ever-present interest in linking disease signs and symptoms, and a continued interest in understanding the underlying physiology responsible for dry-eye heterogeneity. Research explored markers and biomarkers of disease, including INF-γ, Il-1R and MyD88. (Downie L, et al. ARVO E-Abstract 404; Courson J, et al. ARVO E-Abstract 405) Others examined chemokine and cytokine expression. (Kessal K, et al. ARVO E-Abstract 406)
The neural aspects of dry eye were a major topic, with many studies of anatomical and physiological changes in corneal nerve function and how these may impact dry-eye disease. In one study, hyperosmolar stress was shown to damage corneal nerve fibers, (Mizerska K, et al. ARVO E-Abstract 403) while a second study demonstrated a role for vitamin D deficiency in poor nerve function. (Deshmukh R, et al. ARVO E-Abstract 2854) Several presentations established the importance of TrpM8 and TrpV1, membrane sensors responsible for thermo-sensation, as potential players in the signaling pathways impacted by dry eye. (Rocha E, et al. ARVO E-Abstract 393; Song JS. ARVO E-Abstract 416; Situ P, et al. ARVO E-Abstract 2849; Corcoran P, et al. ARVO E-Abstract 2873) In parallel to these studies were those examining thermal imaging techniques to quantify minute temperature changes in the tear film and their potential impact on evaporative dry eye. (Sundstrom C, et al. ARVO E-Abstract 2851; Li W, et al. ARVO E-Abstract 2850; Watson M, et al. ARVO E-Abstract 2858)
ARVO provides a unique, research-oriented perspective on the state of ophthalmic science, allowing us to explore the latest trends and refresh our perspective on current technology and therapy. It’s also a great opportunity to exchange ideas with colleagues and recharge our batteries. As the meeting came to an end, we were reminded again of why we’ve made this pilgrimage for the past 30 years. See you next year in Baltimore. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Dr. Hollander is chief medical officer at Ora, and an assistant clinical professor of ophthalmology at the Jules Stein Eye Institute at the University of California, Los Angeles. Dr. Abelson may be reached at MarkAbelsonMD@gmail.com.
1. Doudna JA, Charpentier E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 2014;28:346:6213.



