Dry-eye syndrome can have a significant impact on visual function that can diminish a person's quality of everyday living, according to researchers in
The study population was drawn from the Women's Health Study and the Physicians' Health Study. Participants' history of DES was assessed with three DES-related questions. Subgroups of 450 WHS and 240 PHS participants were selected based on answers. By design, one-third of the study subjects had clinically diagnosed DES or severe symptoms and two-thirds did not.
Patients were given a supplementary questionnaire asking how their everyday activities were limited by symptoms of dry eye and to what degree eye problems limited them in various everyday activites.
The frequency distribution of participants' answers related to vision-related quality of life was examined, and the Wilcoxon rank-sum test was used to check for an association of each activity score with DES. Individuals who chose a response of not applicable were excluded from analysis of that particular activity. Responses were dichotomized to the presence vs. absence of any degree of problems with each activity. Logistic regression models were used to estimate the odds ratios (OR) and 95 percent confidence intervals (CIs) for the relationship of each activity of daily living with DES while controlling for potential confounding variables. Separate models for men and women were fit.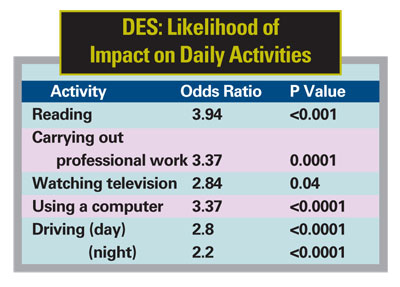
Of the participants invited, 85 percent completed the supplementary questionnaire, including 135 WHS and 55 PHS participants with DES, and 250 WHS and 149 PHS participants without DES. Controlling for age, diabetes, hypertension and other factors, those with DES were more likely to report problems with reading (OR=3.64, 95 percent CI 2.45 to 5.4, p<0.0001); doing professional work (OR=3.94 95 percent CI 1.72 to 7.09, p=0.001); computer use (OR=3.37, 95 percent CI 2.11 to 5.38, p<0.0001); watching television (OR=2.84, 95 percent CI 1.05 to 7.74, p=0.04); driving during the day (OR=2.8, 95 percent CI 1.58 to 4.96, p<0.0001); and at night (OR=2.2, 95 percent CI 1.48 to 3.28, p<0.0001).
Researchers say the study was limited by the classification of DES based on responses to the dry-eye questionnaire. The subjects are somewhat more educated and healthier than the general population, so results should be generalized with caution. The data add further weight to the consideration of DES as a significant public health problem that deserves further study.
(Am J Ophthalmol 2007;143:409-415)
Miljanovic B, Dana R, Sullivan DA, Schaumberg DA.
IVTA Shows Promise Against Pseudophakic CME
Intravitreal triamcinolone acetonide injection is a promising therapeutic tool for chronic pseudophakic macular edema resistant to other medical treatment, according to researchers in
The study included 14 eyes of 14 patients (seven male, seven female) with persistent pseudophakic cystoid macular edema after cataract surgery. The mean age ±SD of the patients was 68.07 ±9.87 years.
All patients underwent uneventful phacoemulsification, and a posterior chamber lens was inserted in the capsular bag. Inclusion criteria were persistent CME for less than six months that was unresponsive to treatment and absence of glaucoma or uveitis before the operation. None of the patients had other ocular diseases.
All patients underwent complete ophthalmic examination, including BCVA (by standard Snellen chart), fundus examination, fluorescein angiography, IOP management, OCT and mf-ERG recording. Patients were treated with triamcinolone acetonide injection and were followed up for one year. Results of OCT and mf-ERG were recorded before and after the injection.
At presentation, BCVA ranged from 0.02 (20/800) to 0.5 (20/40) (mean ±SD, 0.22 ±0.16). Twelve months after a single injection, VA ranged from 0.02 (20/800) to 0.7 (20/30), with the mean VA ±SD increasing to 0.36 ±0.24. In two cases VA remained the same and worsened in one after treatment. Foveal thickness measured by OCT of the affected eyes ranged from 309 µm to 665 µm (mean ±SD, 434.93 ±103.33 µm) before treatment and from 402 µm to 850 µm (mean ±SD, 402.74 ±162.22 µm) 12 months after treatment. In three cases, foveal thickness increased.
Before treatment, the retinal response density of the affected eyes in the fovea ranged from 2.53 nV/deg2 to 10.24 nV/deg2 (mean value ±SD, 4.75 ±2.17 nV/deg2) and from 2.68 nV/deg2 to 8.05 nV/deg2 (mean ±SD, 5.82 ±1.79 nV/deg2) in the parafovea. Twelve months after treatment, the retinal response density in the fovea ranged from 2.9 nV/deg2 to 13.8 nV/deg2 (mean ±SD, 8.27 ±3.13 nV/deg2) and from 7.16 nV/deg2 to 11.7 nV/deg2 (mean ±SD, 8.98 ±1.55 nV/deg2) in the parafovea.
Before treatment, IOP ranged from 12 mmHg to 20 mmHg (mean ±SD, 15 ±2.54 mmHg) and from 11 mmHg to 20 mmHg (mean ±SD, 15.5 ± 2.65 mmHg) 12 months after treatment. During the first three months after treatment, three patients were receiving IOP-lowering drops; 12 months after, only one patient was receiving the drops.
The researchers believe that further studies are needed to assess the treatment's long-term efficacy, its safety and the need for treatment.
(Retina 2007;27:159-164)
Koutsandrea C, Moschos MM, Brouzas D, Loukianou E, Apostolopoulos M, Moschos M.




