The Study
For the OTA, Stephen J. Kim, MD, program director of the vitreoretinal fellowship at Vanderbilt Eye Institute and associate professor of ophthalmology at Vanderbilt University School of Medicine, and his colleagues sought to determine whether previous studies demonstrated the effectiveness of topical NSAIDs in preventing CME-related vision loss after cataract surgery. They estimate that CME detectable by fluorescein angiography occurs in 9 to 19 percent of patients, with the incidence of “visually important” CME occurring in 1 to 4 percent. CME is treatable and often self-limiting, but it can cause permanent vision loss, and its occurrence raises the costs associated with surgery by approximately 50 percent, according to the study’s authors. To investigate NSAIDs’ effect on CME prevention and long-term visual outcomes, defined as visual acuity at three months postop, the researchers performed comprehensive searches of the Cochrane Library and PubMed databases. They ultimately selected and individually analyzed 15 relevant studies, then collectively summarized them. Dr. Kim and his colleagues concluded that topical NSAIDs hasten visual recovery in routine cataract surgery patients, but they found no gains in visual acuity three months postoperatively compared to patients treated with certain corticosteroids alone or placebos. They also found no support for the conventional wisdom that NSAID drops work synergistically with topical steroids.
“NSAIDs are fine drugs,” says Dr. Kim. “But they are a weaker anti-inflammatory than corticosteroids, and their effects are redundant. Their addition may speed visual recovery, but they add nothing to the end result.” To help speed attainment of best visual results, he says, surgeons can increase the dosages of topical steroids.
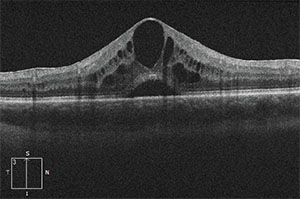 |
| OCT image of a retina with CME. Disruption of the blood-retinal barrier due to postop inflammation may contribute to the condition.2 |
As to why surgeons keep using topical NSAIDs, Dr. Kim says, “It is so ingrained in the culture. It’s also driven by industry.” He adds that the extant studies haven’t looked at the effect of NSAIDs alone in preventing CME. “Historically, all the studies done so far have not been fair studies, in that they’ve compared patients on two medications [NSAIDs and corticosteroids] to patients taking corticosteroids alone. That’s not a one-to-one comparison. A truly fair study would be comparing one patient population using just NSAIDs to one using steroid medication alone, say, four times daily, for both groups. That study has never been done. It has always been a comparison of a corticosteroid group to people who are getting twice as much medication, and the effects of the NSAID are redundant there.
“The evidence we have so far is conflicted,” continues Dr. Kim, who emphasizes that his position with a nonprofit teaching hospital precludes any potential financial interest in his findings. He also acknowledges that the community practice of using postop NSAIDs will probably remain in place for the foreseeable future. “It may take 10 or 20 years to move the standard of care,” he says.
Should the Standard Change?
An editorial accompanying the OTA anticipated that it would be “provocative,” and disclosed that expert reviewers from the American Society of Cataract and Refractive Surgery had objected to the initial draft because they believed its emphasis on Snellen chart acuity three months postoperatively failed to consider potential problems arising from even transient edema preventable by NSAIDs, such as patient anxiety, diminished productivity and independence, and costs of additional testing.3 The ASCRS reviewers recommended visual acuity at one month and patient-reported quality of life as better criteria to measure the value of NSAIDs. Because the OTA panel stuck with visual acuity at three months as its metric, the ASCRS experts declined to endorse the OTA.
While there may not be any one-to-one controlled studies comparing NSAIDs and steroids, other research hints at their standalone value in preventing CME. At the ASCRS 2014 Symposium, Keith Walter, MD, presented a paper suggesting that topical NSAID monotherapy may in fact be more effective than corticosteroids—either alone or with NSAIDs—to prevent CME.4 Dr. Walter’s five-year retrospective analysis of 5,000 cataract surgeries showed that name-brand bromfenac drops by themselves prevented CME as well or better than combinations of corticosteroids and NSAIDs.
It’s important to emphasize that the above-mentioned paper and the OTA investigated two subtly different things: NSAIDs’ efficacy in postoperative CME prevention versus the usefulness and cost-effectiveness of NSAIDs in preventing long-term, CME-related vision loss. Dr. Kim and his co-authors acknowledged this limitation in the OTA. “Although long-term visual acuity (≥ three months) after cataract surgery is an important clinical measure of a therapeutic intervention,” they wrote, “this assessment was not designed to comment on the rationale and potential value of NSAID therapy in preventing CME soon after surgery and the patient satisfaction and quality-of-life improvement associated with more rapid visual rehabilitation.”2
Dissenting Opinions
David R. Hardten, MD, in private practice with Minnesota Eye Consultants and an adjunct professor at the University of Minnesota Department of Ophthalmology and the Illinois College of Optometry, reports that his postop use of NSAIDs for cataract cases remains unchanged after the OTA. “The data has had some articles in favor of NSAIDs, and some articles suggesting that maybe there’s no benefit, but I’ve used them for a very long time and been happy with the results. I think they do provide a little bit better patient comfort after surgery, as well as reducing cystoid macular edema.
“I typically use them twice a day for the first week, and then once a day typically until the bottle’s empty or four weeks—whichever comes first,” he continues. “I use them in routine eyes, and I use them a little bit longer in patients who have risk factors for cystoid macular edema, like diabetics or folks with epiretinal membrane.”
One built-in limitation of the OTA is the historic lack of uniform criteria for identifying CME. However, OCT and fluorescein angiography detect macular thickening during the early postop period, even in the absence of visual CME symptoms such as loss of visual acuity on a Snellen chart, diminished contrast sensitivity and metamorphopsia.
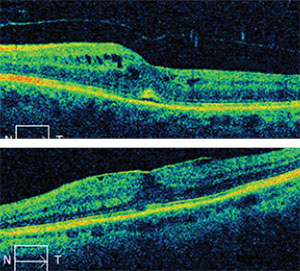 |
| Top: CME in an eye untreated by NSAIDs at five weeks. Visual acuity was 20/50. Epiretinal membrane was present preoperatively. Bottom: The same eye after a six-week course of treatment combining NSAIDs and steroids. Visual acuity was 20/20. |
Those early postop weeks can become especially fraught with high expectations if your patient is set to undergo a second consecutive cataract procedure, Dr. Hardten notes. “Sometimes, that’s right when you’re trying to get their second eye done. You want them to be pretty happy with that first result, but when they’re dealing with even a subtle amount of cystoid macular edema, sometimes it’s hard to have them be happy about the prospect of submitting to the surgery for a second time.”
Johnny L. Gayton, MD, in private practice at Eyesight Associates in Warner Robins, Ga., and adjunct professor of ophthalmology at Mercer University School of Medicine, also factors in patient expectations when prescribing topical NSAIDs and sees no reason to stop using them. Dr. Gayton concurs that patients want “premium outcomes” in this age of premium IOLs, but opines that the distinction between visually bothersome CME and macular thickening unaccompanied by patient complaint is meaningless when deciding to use NSAIDs: “If you have as little as 10 to 20 microns of macular thickening, which reduces your contrast, whether it bothers somebody or not is actually baseless. There are patients who are not going to complain if you cut their little finger off; there are other patients who are going to complain at just a slight decrease in contrast sensitivity. If you want the absolute best outcome for each patient, why not give them something that’s going to make that better outcome more likely?
“There are lots of reasons to use a nonsteroidal, and not just for the prevention of CME,” he continues. “Nonsteroidals help with pain. Nonsteroidals help get inflammation under control more quickly, and any time you get inflammation under control more quickly, you get quicker visual recovery. “ Dr. Gayton prescribes NSAID drops for four to six weeks postoperatively in patients with no known CME risk factors, and for a minimum of eight weeks in patients with known risks.
Dr. Gayton remains convinced of the synergistic effect of combining topical NSAIDs with steroids, and likens blocking multiple inflammatory pathways with two different eye drops to competing in mixed martial arts. “IN MMA, you get hit with fists, and you get kicked, both. If you have multiple weapons, you’re much more likely to be successful than if you only have one. So you use both a steroid and a nonsteroidal,” he says.
Dr. Gayton says that he would prescribe NSAIDs if forced to choose between drug classes, because they are specific and less prone to causing side effects. “You don’t get pressure spikes with a nonsteroidal: You do with steroids,” he says. Still, he routinely uses steroids with NSAIDs. “You use both to start with, and you get the inflammation under good control, then just continue with the nonsteroidal to prevent the long-term sequelae of inflammation, such as CME.”
Dr. Kim, however, maintains that combining NSAIDs and corticosteroids is an unnecessary step in routine eyes, because topical steroids alone can safely do the job of preventing CME in low-risk patients. While he acknowledges that there may be a role for NSAIDs in inflammation-prone patients such as those with severe diabetes, he says that topical steroid monotherapy delivers the same long-term outcome and is generally well tolerated. “We are only looking at use of steroid drops for a very limited time, four to six weeks, and any adverse effects tend to be very limited no matter which medication you’re using,” he says. “The potential adverse effects, including corneal haze, corneal melting and increased IOP are similar, whether you use NSAIDs or steroids for CME prevention.”
While he acknowledges that not every cataract patient will need postoperative NSAIDs, Dr. Gayton chooses to err on the side of caution. “Sure, there are people in high-risk categories, but we have all seen folks develop problems that you wouldn’t expect. Nonsteroidals make that less likely to happen.” In his experience, omitting NSAIDS opens the door to higher incidences of CME. Dr. Gayton relates that with the advent of “dropless” cataract surgery, he continued to prescribe NSAID drops postoperatively—and saw CME cases increase in the dropless patients of colleagues who didn’t. “I’ve had cataract surgery myself,” he says. “I’m a low-risk guy, but I used my nonsteroidal. My mother is low risk as well, but I used a nonsteroidal on her.”
Long-term Outcomes vs. Short–term Value
In addition to valuing NSAIDs as a means of shutting the door to the early development of CME and speeding visual recovery, both Dr. Hardten and Dr. Gayton prescribe them for pain control. “Another thing to consider is that it may provide some comfort to the patient, because the NSAID has a little bit of an anesthetic effect on the ocular surface,” notes Dr. Hardten. “So sometimes that incisional discomfort on the first few days is less with an NSAID.”
As a former cataract patient, Dr. Gayton gives credence to patient complaints of postoperative pain and says NSAIDs definitely help. “If people don’t hurt, they love it,” he says.
Pain control, like speed of visual recovery, is a short-term, quality-of-life measure not evaluated in the OTA. Dr. Kim and his colleagues estimated that topical NSAIDs have an average wholesale price of $70 to $130 per bottle, representing up to $180 in added surgery costs.2 Even in the face of the OTA’s finding that these additional costs may well be unnecessary in the long run, surgeons and their patients seem to consider NSAIDs a worthwhile expense for reasons outside the scope of the study: closer alignment of early visual results with patient expectations, comfort, and overall quality of life. REVIEW
Dr. Kim and Dr. Hardten report no relevant financial interests; Dr. Gayton is a paid consultant for Bausch + Lomb, Shire, Sun and Omeros.
1. Irvine SR. A newly defined vitreous syndrome following cataract surgery. Am J Ophthalmol 1953;36;5:599-600,600a,600b,601-19.
2. Kim SJ,Schoenberger SD, Thorne JE et al. Ophthalmic technology assessment: Topical nonsteroidal anti-inflammatory drugs and cataract surgery. Ophthalmology 2015;122;11:2159-68.
3. Jampel HD. Ophthalmic technology assessments. Ophthalmology 2015;122;11:2157-8.
4. Walter K. Effect of perioperative drop regimen on CME after cataract surgery. ASCRS 2014 Symposium. Presented April 25, 2014.



