Point: Reply on Limbal Anterior Vitrectomy
Robert Maloney, MD, MA
Los Angeles
 |
I’m concerned to see how often pars plana vitrectomy is promoted as the optimal approach to vitrectomy for the anterior segment surgeon. Pars plana vitrectomy carries some serious risks, such as retinal tears and detachments. These are unnecessary chances to take, since most cases that require vitrectomy can easily be handled by a limbal approach. In this article, I’ll explain why the limbal approach is preferable for most patients.
No Problems with Vitreous
The most significant reason given for anterior segment surgeons to do pars plana vitrectomy is that limbal vitrectomy causes vitreous to come forward into the anterior chamber. This is not true. If there’s a central tear in the posterior chamber—or no posterior capsule—the vitreous can be managed without difficulty by using a limbal approach. With bimanual instruments, make watertight paracenteses and place the port of the vitrectomy cutter well behind the posterior capsule. You’ll clean up the vitreous without bringing any of it forward into the anterior chamber. The idea that vitreous will continue moving forward is a misconception arising from three sources:
 |
• Source 1: Surgeons place the cutting port too anteriorly. Vitreous comes to the cutting port of your aspirating handpiece, meaning it moves to wherever you put the port. If you perform a limbal vitrectomy and put the port behind the posterior capsule, vitreous won’t come forward. However, surgeons tend to place the vitrectomy port in the iris plane, where, of course, the port will pull the vitreous forward. It’s fine to start in the iris plane, but the surgeon should move the port posteriorly, cutting all the while to avoid traction, until the port is well behind the posterior capsular opening. Ideally, the port is just anterior to the most posterior focal plane of the operating microscope. This location is in the anterior third of the vitreous, where it’s not possible to cut the posterior capsule or iris. Vitreous will then stay in the posterior chamber.
• Source 2: Surgeons used to do coaxial vitrectomy with a single handpiece. In the old days, surgeons did vitrectomy with a combined infusion-cutting device. The irrigation sleeve was positioned over the aspiration-cutter, meaning that the handpiece hydrated the vitreous while it was simultaneously pulling vitreous into the cutter. Convection currents dispersed vitreous away from the cutting port and into the anterior chamber. Everyone now uses (or should use) bimanual vitrectomy instruments, with separated infusion and aspiration/cutting ports.
• Source 3: Surgeons tolerate leaky limbal wounds. Wound leaks bring vitreous forward, because vitreous moves to any area of low pressure. If you have leaky paracenteses around your bimanual instruments, vitreous will move into the anterior segment and to the wound. Make small watertight paracenteses for your vitrectomy probes.
Exceptions to Consider
If you can’t get good access to the vitreous when entering the eye through the limbal port, you may want to use pars plana. Two classic situations are as follows:
• You have zonular dehiscence, and vitreous is coming forward around the zonule. You can’t move the vitrectomy port around the zonule and into the posterior chamber. Pars plana vitrectomy is the preferred approach for the anterior segment surgeon at moments like these.
• After the IOL is already implanted, you discover a posterior capsule tear or create a posterior capsule tear. You can usually access the vitreous more easily by using the pars plana approach, rather than trying to work around the intraocular lens prosthesis.
Other than when anterior segment surgeons are dealing with exceptions such as these, they should consider limbal anterior vitrectomy to be their procedure of choice.
Risks of Pars Plana Vitrectomy
The primary risks of pars plana vitrectomy are retinal tear and detachment, which can occur in several ways. The surgeon can engage the vitreous base with the instrument, causing a dialysis or giant retinal tear. Alternatively, if the surgeon uses an MVR blade to make a scleral opening rather than using a trocar system, a knuckle of vitreous can prolapse through the incision. This can create retinal traction, particularly in the vitreous base area, and can become a scaffold on which fibrosis can develop. These responses can lead to a retinal detachment.
It’s a rare anterior segment surgeon I know who can intraoperatively manage a retinal tear caused by a pars plana vitrectomy. Retina surgeons, on the other hand, routinely check the pars plana by scleral depression after they complete a vitrectomy. They can treat any retinal tears they find—right then and there. Anterior segment surgeons almost universally do not or cannot do this. And that means when anterior segment surgeons perform a pars plana vitrectomy, they take on higher risks and put their patients at higher risks than retina surgeons do.
Trocar systems, an important advance, lower the risk of traction on the vitreous base, but they’re risky in an open eye because the globe can collapse from the pressure of insertion. This point is important to consider because we anterior segment surgeons usually don’t know that we need a vitrectomy until the eye is already open. Retinal surgeons routinely remove all the vitreous in the eye before operating on the retina. They also perform pars plana surgery quite regularly, while we do it very rarely. Sub-specialists like Steve Charles are really good at it. To be candid, we anterior surgeons, for the most part, are not very good at it.
In Closing
At the completion of the anterior vitrectomy, use triamcinolone acetate to confirm the anterior chamber is free of vitreous. You’ll find limbal vitrectomy is a very effective way to remove vitreous from the posterior chamber without bringing vitreous forward—as long as you perform bimanual vitrectomy with watertight incisions and place the cutting port well behind the posterior capsule.
Counterpoint: Pars Plana is the Better Approach
Steve Charles, MD
Germantown, Tenn.
 |
There is currently a controversy concerning whether the vitreous cutter should be used through a limbal sideport or the pars plana when anterior vitrectomy is required during cataract surgery. Though the former may seem more appealing to the typical anterior segment surgeon, it has several disadvantages that make a pars plana approach better. Here, I’ll explain the benefits of pars plana in detail and provide insights on challenges you’ll need to meet if and when you use this preferred method for anterior vitrectomy.
The Drawbacks of Limbal
Pars plana is the better approach because it involves less endothelial trauma caused by turbulence, more complete anterior vitrectomy because of posterior movement of the vitreous and less risk of iris and capsule damage from direct contact with the cutter.
For example, in one study that compared limbal and pars plana microincision vitrectomy for removal of congenital cataracts with primary intraocular lens implantation, more eyes had at least one intraoperative complication in the limbal group (40 eyes in 26 patients) than in the pars plana group (41 eyes in 30 patients). The most common intraoperative complications were iris aspiration, iris prolapse and iris injury. The study recommended use of the pars plana approach to ensure a lower incidence of complications.1
 |
| All illustrations: ByronWood |
Some anterior segment surgeons, in fact, have promoted pars plana as a safer approach because it lets you efficiently remove vitreous from the anterior chamber without it; limbal infusion creates the pressure gradient that results in this advantage. This is safer than pulling vitreous anteriorly, which can potentially create vitreoretinal traction and retinal breaks. Limbal anterior vitrectomy can result in residual vitreous strands that can be challenging to remove and may even appear the day after surgery.
The pars plana approach allows the surgeon to use the vitreous cutter to remove remaining lens fragments in a much more efficient manner than can be achieved from the limbus. Dislocation of lens fragments is a serious issue because it increases risks of retinal detachments, secondary glaucoma and cystoid macular edema.2
When used with cataract surgery, pars plana vitrectomy’s advantages have been documented in another study. Researchers looked at 335 eyes that had undergone anterior vitrectomy, and they concluded that a sutureless pars plana approach might be considered a safe and reliable solution for anterior segment surgeons in managing vitreous prolapse during anterior segment surgeries.3
Meanwhile, the principal advantage of limbal vitrectomy is the cataract surgeon’s familiarity with the approach, although some argue that the limbal approach also reduces risk to the peripheral retina.
Minimize the Drawbacks
One of the purported drawbacks of a pars plana approach is the heightened risk of retinal damage. However, in my experience, you can minimize this risk with the proper technique (and this logic applies to whichever approach you choose). A pars plana approach is just as safe as the limbal approach with respect to the risk of retina damage if you keep critical principles in mind:
• Never use cellulose sponges to remove or test for vitreous. The sponges create unacceptable instantaneous intraoperative traction.
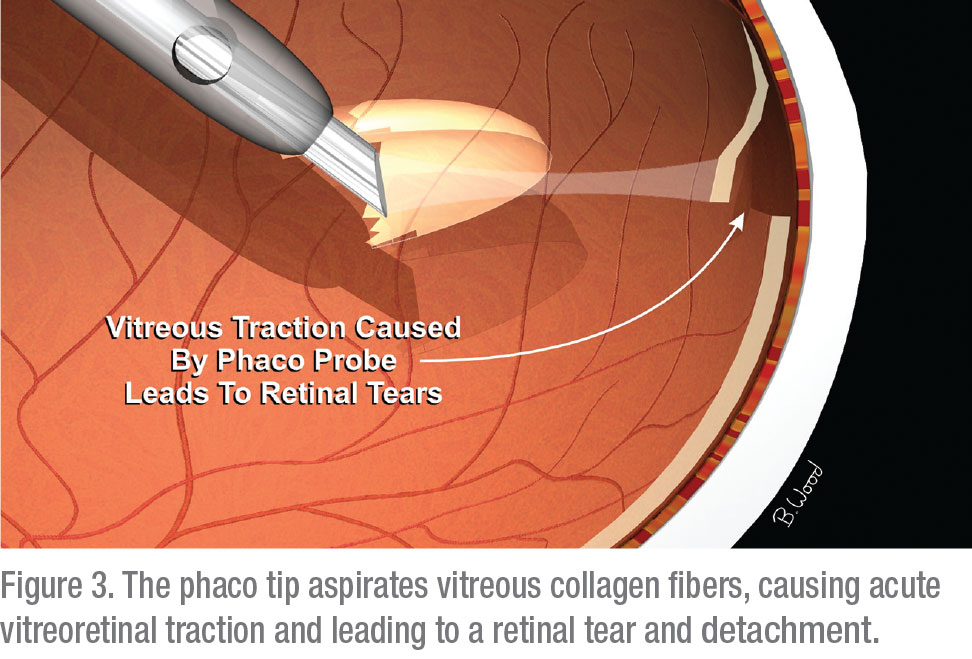
• Never apply aspiration to a vitreous cutter without first activating the cutting function. This prevents acute vitreoretinal traction from causing retinal tears.
• Never pull a vitreous cutter back while you’re applying aspiration. This is important to prevent acute vitreoretinal traction from causing retinal tears. Remember: Use the opposite of I/A technique in these situations.
Besides following these principles, you’ll always need to make sure you use the highest possible cut setting to reduce pulsatile vitreoretinal traction. Also, use the lowest effective flow rate (peristaltic pump) or vacuum (venturi) to decrease intraoperative traction and therefore the risk of iatrogenic retinal breaks. Using triamcinolone particulate marking will help you visualize better and judge how effectively you’re performing the procedure.
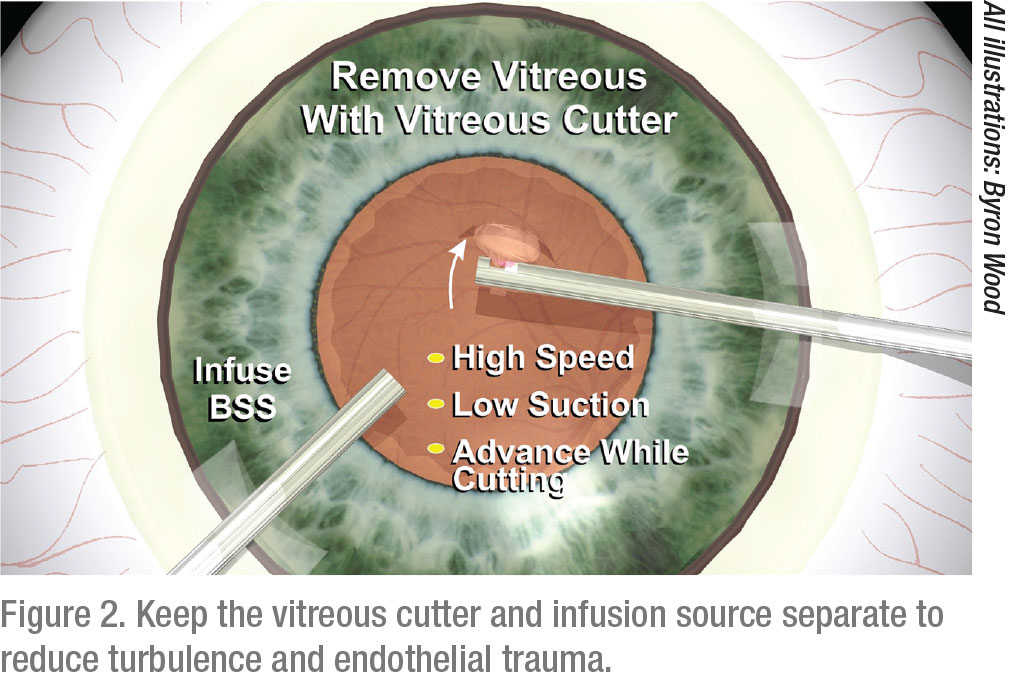
Also, always make sure you place the infusion through a sideport—whether using a limbal or the pars plana route for the vitreous cutter. Never use a sleeve over the vitreous cutter for infusion. The vitreous cutter and infusion source must be separate to reduce the turbulence and the endothelial trauma I mentioned and to more effectively remove vitreous.
Remember that anterior vitrectomy is performed close to the vitreous base, the region of permanent and very strong vitreous adherence to the retina. Furthermore, keep in mind that the peripheral retina has 1/100th the tensile strength of the retina near the optic nerve.
Forego a Trocar Cannula
Another way to avoid common complications with pars plana anterior vitrectomy is to forego the use of a trocar cannula. Remember that a trocar-cannula system requires greater insertion force, produces much higher intraocular pressure during insertion, and is therefore more likely to cause wound disruption and iris prolapse and even penetration of the opposite side of the eye. The primary purpose of cannula-based surgery is to protect the wound during multiple tool exchanges, which is not relevant to anterior vitrectomy during cataract surgery.
 |
To prevent wound disruption when performing any anterior vitrectomy, the anterior segment surgeon must make sure the cataract wound is sutured, not hydrated, and this is true whether or not the surgeon is using a trocar-cannula system. In addition, to avoid complications often cited by advocates of limbal-based anterior vitrectomy, the pars plana surgeon needs to keep in mind that a scleral tunnel approach to pars plana wound construction is inappropriate for anterior vitrectomy during cataract surgery. This is because a relatively soft eye can lead to instrument insertion under the retina or in the choroid, resulting in catastrophic suprachoroidal hemorrhage and/or retinal detachment. A straight-in approach, with the cutter roughly perpendicular to the scleral surface and without a scleral tunnel, is the safest technique.
Parting Thoughts
In general, keep this point is mind: There is no such thing as a “simple” anterior vitrectomy. Patients don’t want—nor do they expect—a retinal detachment after cataract surgery. It’s critical, of course, for us to do everything we can to prevent such a poor outcome, employing vitrectomy as safely and effectively as possible.
When the need for vitrectomy arises during cataract surgery, as it will from time to time, surgeons need to be prepared to act quickly and confidently. The pars plana approach will help them succeed if they apply these principles. REVIEW
Dr. Charles is a clinical professor of ophthalmology at the University of Tennessee Hamilton Eye Institute. Contact him at: Charles Retina Institue, 6401 Poplar Ave., Ste 190, Memphis, Tenn. 38119. scharles@att.net.
He consults with Alcon.
Dr. Maloney is director of the Maloney Vision Institute in Los Angeles and clinicial professor of ophthalmology at the David Geffen School of Medicine at UCLA. He reports no financial interest in any products mentioned.
1. Liu X, Zheng T, Zhou X, et al. Comparison between limbal and pars plana approaches using microincision vitrectomy for removal of congenital cataracts with primary intraocular lens implantation. J Ophthalmol 2016;8951-53.
2. Jacobs PM. Vitreous loss during cataract surgery: Prevention and optimal management. Eye (Lond) 2008:10:1286-9.
3. Thornton IL, McMains BK, Snyder ME. Long-term safety and efficacy of single-port pars plana anterior vitrectomy with limbal infusion during anterior segment surgery. J Cataract Refract Surg 2018;44:7:878-883.



