Strabismus is one of the most common ocular problems in children, affecting 5 percent of the preschool population.1 It also affects a significant proportion of adults, both as an acquired condition as well as a lifelong condition necessitating continued symptomatic management. Though there are different approaches to treating the condition, we’ve found muscle plication to be effective in many cases. Here, we describe details of the technique, in addition to potential benefits of the procedure.
Plication vs. Resection
Surgical alternatives to rectus muscle resection have been available for over 100 years. The cinch technique, originally described in 1916, involves weaving a cable of suture (four strands of 3-0 nylon tied together to create an eight-strand cable) through a split muscle and tying the cable off to create a resection effect.2 The technique gained limited popularity in the 1930s, but eventually fell out of favor. Muscle tucking was introduced in 1983 as a quick procedure that avoided cutting the extraocular muscle.3 This procedure, however, has also fallen out of favor for rectus muscles, as the muscle-to-muscle suture fixation relaxes over time.4 An alternate approach was introduced by Los Angeles surgeon Kenneth Wright in 1991: a modified rectus tuck where muscle is sutured to sclera, representing the plication procedure.5 More recently, several authors have studied the effectiveness of the plication technique with favorable reviews.6-11
Several advantages of plication have been proposed: There’s no risk of a lost muscle, since the muscle is never disinserted from the sclera; it preserves anterior ciliary circulation; and there’s less tissue trauma and bleeding than in resection.12,13 Additionally, the procedure’s technique is arguably simpler than resection’s and can possibly result in decreased operative time. One disadvantage, however, is that because the muscle is never disinserted from the sclera, plications can’t be used to shift muscles for pattern strabismus (i.e., A- or V-pattern esotropia) or small vertical deviations in which the surgeon wishes to perform a vertical transposition of the horizontal rectus muscle(s) to address the vertical deviation.
 |
Surgical Technique
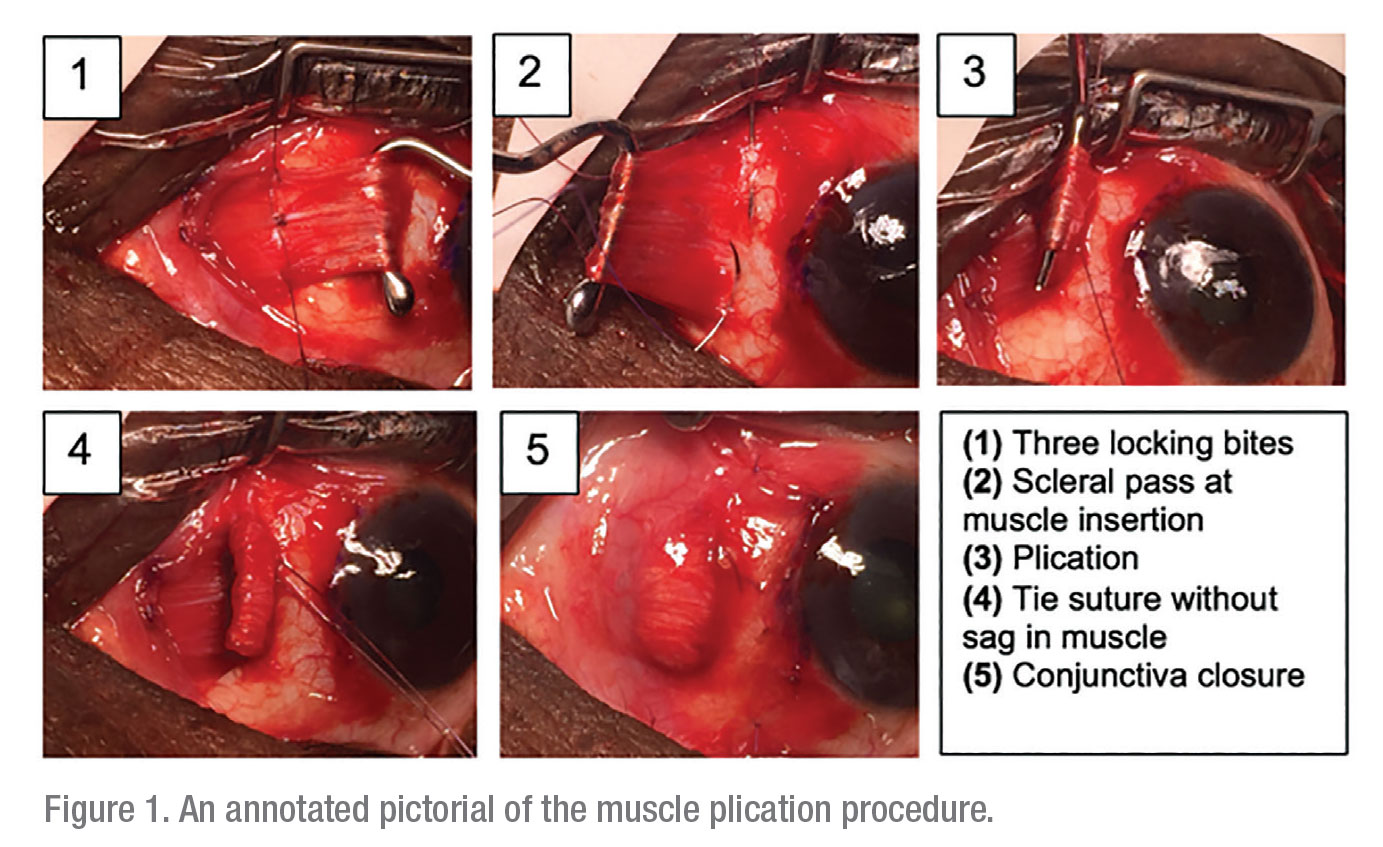
The muscle plication surgical technique can be performed through either a fornix or limbal incision using surgical dose tables identical to those used for traditional resection, as described by Marshall Parks, MD, and co-authors.14 Figure 1 outlines the steps of the plication procedure.
Using a 6-0 double-armed Vicryl (Ethicon) suture with a spatulated needle, a locking bite is placed at either pole of the muscle with an optional central locking bite for secure imbrication at the desired location, according to standard charts for resection. Each suture needle is then passed through partial-thickness sclera, just anterior to the poles of the muscle insertion. A wide, narrow-gauge hook, such as the Helveston Finder hook (Katena), is then placed under the muscle to create the plication fold. We prefer this particular hook, as it’s not only thin but also has no knob at the end, making it easier to slide the instrument out after the plication suture is tied securely. The posterior portion of the muscle is advanced up to the original insertion by pulling on the two suture ends until the posterior suture line is flush with the insertion, thereby creating the appropriate resection effect.
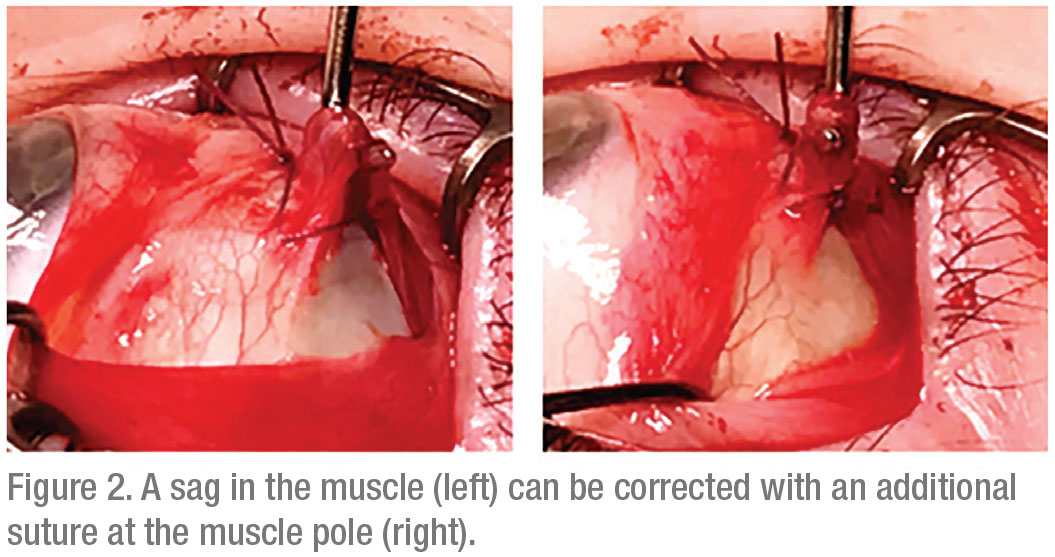
To ensure success, it’s imperative that no gap is left between the suture line and muscle insertion. Full approximation of the muscle fold segments at the muscle borders should be confirmed before the second locking knot is tied over the first double or triple-wrap suture throw. If any residual muscle gap is noted after the suture is tied, we recommend augmenting the plication with an additional suture throw at the pole of the muscle (muscle through partial-thickness sclera) to close the gap, as shown in Figure 2.
Postoperative Results
With plication, patients can expect postoperative alignment similar to that achieved with resection. In one study, surgeons compared 22 plication procedures to 31 resections and found an overestimation of surgical effect for exotropia at doses less than 4 mm and overestimation of effect for resection exceeding 7 mm.6 Therefore, a typical range of 20 to 50 PD of exotropia led to similar results with plication or resection. The immediate postoperative result and the long-term result (119 days for plication and 966 days for resection) didn’t vary significantly.
Other studies have found negligible differences between plication and resection for esotropia. A 2018 paper reviewed 88 plications for esotropia and 31 plications for exotropia with follow-up ranging from four weeks to 72 months.11 All surgeries were combined with recession of the antagonist muscle. Surgical success, defined as ≤10 PD of undercorrection and of ≤4 PD overcorrection (measured between postoperative weeks four and 16), was found in 95.5 percent of plications for esotropia and 77.4 percent of plications for exotropia—this was similar when compared to resection for similar amounts. Re-operation rates between the two groups were also similar after as long as 72 months of follow-up.
 |
Several studies cite similar surgical results for plication and resection up to a year following surgery.8,10 However, there’s sparse literature regarding success of the plication procedure several years out from the surgery. In a study by Boston surgeons Maan Alkharashi and David Hunter, they suggested that there’s a decreased surgical success rate with rectus muscle plication.15 Their study included 48 resections and 24 plications with surgical success defined as ≤10 PD deviation for horizontal muscles and ≤6 PD for vertical muscles. The success rates of 89 percent for resection versus 59 percent for plication were similar at six and 12 weeks of follow-up, as well as the final mean follow-up (19 ±13 months; range: three to 56 months). One could argue, however, that the quoted short-term success rate in this study varies from the favorable short-term success rates quoted in the aforementioned studies.6-11 We’ve been pleased with the surgical result of plication at our institution, with some patients having a follow-up of up to five years. We are currently reviewing our long-term data for plication procedures.
Postoperative Healing
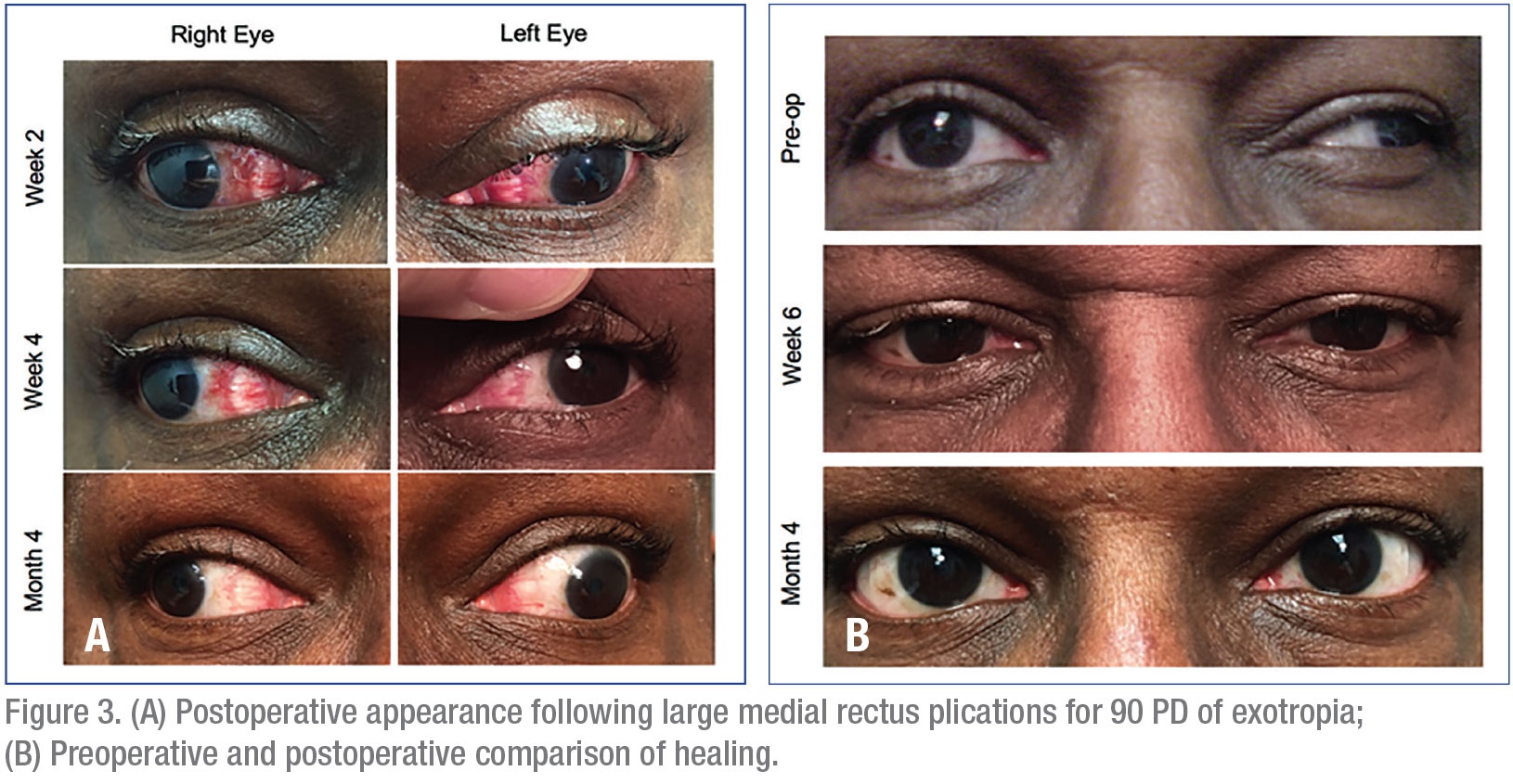
Some surgeons express concern regarding the appearance of the eye during wound healing, with a temporary visible “bump” of tissue after surgery. To date, we haven’t encountered any patients with significant concerns regarding cosmesis or plication adversely effecting ocular surface healing. We use this approach for both adults and children with strabismus. A randomized, prospective study evaluated an aggregated inflammatory score (congestion, chemosis, discharge, foreign body sensation and drop intolerance) in addition to scar visibility at one month, between patients undergoing resection or plication. It found similar results between groups.9 Figure 3 shows the typical postoperative appearance of the eye following plication and a comparison of the preoperative appearance to the postop appearance after healing. Even with a large plication, the fold of muscle settles nicely several months following surgery. In our experience, patients and family members are generally not concerned about the appearance of the eye following plication. For patients who may be concerned about cosmetic appearance, we recommend a discussion regarding postop expectations, during which you let them know that a noticeable “bump” of tissue may be seen, but will settle several months after surgery. This timing coincides with that of our typical second postop visit three months following surgery.
 |
Other Benefits
Anterior segment ischemia (ASI) is a rare but potentially serious complication of strabismus surgery that can result from disinsertion of the rectus muscles disrupting the blood supply to the various anterior segment structures via the anterior ciliary arteries. Multiple studies have examined the effect of strabismus surgery techniques on anterior segment circulation in both primates and humans. These studies have demonstrated that plication procedures spare the anterior segment circulation as long as care is taken to avoid the anterior ciliary arteries, both superficial to the muscle tissue and in the sclera, when passing the needle.12,13,16,17 Furthermore, one study found that postoperative iris-filling defects seen on iris angiograms were more common following vertical rectus muscle surgery that involved muscle disinsertion, consistent with the distribution of anterior ciliary and long posterior ciliary arteries providing anterior segment circulation.13,17 Therefore, plications may be a safer alternative for certain muscle surgeries in patients at risk for ASI. This is especially pertinent for re-operations and multi-muscle surgeries such as those for nystagmus.5,17
Plications are also potentially reversible in the early postoperative period since no tissue is removed as in a traditional resection.6 However, in his description of the technique, Dr. Wright cautions that any reversals need to be done within three days of the original surgery, prior to the muscle healing to the sclera.5 Our personal experience confirms that the muscle can’t be separated from sclera as early as one month postoperatively, and by three months or more, one cannot even find visible evidence that a plication has been performed (as demonstrated in Figure 3). One group of researchers, however, described an adjustable plication procedure which may offer an additional option for those situations wherein early modification may be desired.18
In conclusion, muscle plication provides results comparable to resection as a strengthening procedure in strabismus surgery. Advantages include its procedural simplicity with short operative time, decreased risk of tissue trauma and bleeding, and decreased risk of lost or slipped muscle, since the muscle is never disinserted from the globe. Further, it may be beneficial in cases where anterior segment ischemia is a specific concern, as plications may preserve anterior segment circulation if done correctly. We feel that plication is a surgical equivalent to traditional resection in terms of alignment and cosmetic outcomes, and our patients have tolerated plication procedures very well to date. Muscle plication is an important skill to have on hand in the strabismus surgeon’s toolkit. REVIEW
Drs. Stunkel and Mehner are completing their pediatric ophthalmology fellowship at Indiana University. In the summer of 2020, Dr. Stunkel will be joining Mercy Hospital in Saint Louis and Dr. Mehner will be joining the University of Colorado in Denver.
Dr. Boente is an assistant professor of clinical ophthalmology and ophthalmology residency program director at Indiana University.
Dr. Neely is a professor of clinical ophthalmology at Indiana University and an international expert in the fields of pediatric ophthalmology and adult strabismus.
None of the authors have any financial interest in the surgical products cited within this article.
1. Robaei R, Rose KA, Kifley A, Cosstick M, Ip JM, Mitchell P. Factors associated with childhood strabismus: Findings from a population-based study. Ophthalmol 2006;7:113.
2. Williams AT, Metz HS, Jampolsky A. The O’Connor cinch revisited. Br J Ophthalmol 1978;62:11:765-9.
3. Hamtil LW. A study in tucking extraocular muscles to correct strabismus. Ann Ophthalmol 1983;15:2:136-7.
4. Wright, KW, Ning, YJ. Pediatric Ophthalmology and Strabismus. New York: Oxford University Press, 2012.
5. Wright KW. Rectus strengthening procedures. In: Wright KW, ed. Color Atlas of Ophthalmic Surgery: Strabismus. Philadelphia: Lippincott, 1991.
6. Chaudhuri Z, Demer JL. Surgical outcomes following rectus muscle plication: A potentially reversible, vessel-sparing alternative to resection. JAMA Ophthalmol 2014;132:5:579-85.
7. Kühne J, Palmowski-wolfe A. Plication versus resection in horizontal strabismus surgery. Klin Monbl Augenheilkd 2019;236:4:442-445.
8. Sukhija J, Kaur S. Comparison of plication and resection in large-angle exotropia. J AAPOS 2018;22:5:348-351.
9. Sonwani P, Amitava AK, Khan AA, et al. Plication as an alternative to resection in horizontal strabismus: A randomized clinical trial. Indian J Ophthalmol 2017;65:9:853-858.
10. Kimura Y, Kimura T. Comparative study of plication-recession versus resection-recession in unilateral surgery for intermittent exotropia. Jpn J Ophthalmol 2017;61:3:286-291.
11. Huston PA, Hoover DL. Surgical outcomes following rectus muscle plication versus resection combined with antagonist muscle recession for basic horizontal strabismus. J AAPOS 2018;22:1:7-11.
12. Wright KW, Lanier AB. Effect of a modified rectus tuck on anterior segment circulation in monkeys. J Pediatr Ophthalmol Strabismus 1991;28:2:77-81.
13. Oltra EZ, Pineles SL, Demer JL, Quan AV, Velez FG. The effect of rectus muscle recession, resection and plication on anterior segment circulation in humans. Br J Ophthalmol 2015;99:4:556.
14. Parks MM, Mitchell PR, Wheeler MB. Concomitant esodeviations. In: Tasman W, Jaeger EA, eds. Duane’s Foundations of Clinical Ophthalmology, vol 1. Philadelphia: Lippincott Williams & Wilkins, 2002:12.
15. Alkharashi M, Hunter DG. Reduced surgical success rate of rectus muscle plication compared to resection. J AAPOS 2017;21:3:201-204.
16. Park C, Min BM, Wright KW. Effect of a modified rectus tuck on anterior ciliary artery perfusion. Korean J Ophthalmol 1991;5:1:15-25.
17. Pineles SL, Chang MY, Oltra EL, Pihlblad MS, et al. Anterior segment ischemia: etiology, assessment, and management. Eye 2018;32:173-178.
18. Velez FG, Demer JL, Pihlblad MS, Pineles SL. Rectus muscle plication using an adjustable suture technique. J AAPOS 2013;17:5:480-483.



