 |
Researchers compared two-year outcomes of primary mitomycin-C augmented combined phacotrabeculectomy (phaco+trab) with isolated trabeculectomy (trab) in phakic patients with primary open angle glaucoma and primary angle closure glaucoma.
They retrospectively reviewed primary glaucoma patients who underwent MMC-augmented trabeculectomy and completed two years of follow-up. Failure rate, postoperative intraocular pressure, percentage of IOP reduction, and the number of glaucoma medications at 24 months after surgery were compared between the phaco+trab and trab groups.
The study included 146 eyes of 121 patients; 74 underwent trab and 72 underwent phaco+trabeculectomy. Here are some of the findings:
• POAG was present in 71 eyes and PACG was present in 75 eyes.
• Defining a failure with IOP criteria of >18 mmHg or IOP reduction of <30 percent, the failure rates were 42 percent for phaco+trab and 62 percent for trab.
• The phaco+trab group had a significantly lower failure rate than the trab group for all subjects (risk ratio [RR] 0.60; CI, 0.44 to 0.81, p=0.001):
— POAG subgroup (RR, 0.61; CI, 0.41 to 0.93, p=0.02); and
— PACG subgroup (RR, 0.53; CI, 0.33 to 0.86; p=0.01).
• Differences in the postoperative intraocular pressure, percentage of IOP reduction and number of glaucoma medications weren’t significant between the two groups for all subjects: POAG and PACG (all p>0.05).
• The magnitude of effect of adding phacoemulsification to the trabeculectomy was comparable for POAG and PACG groups for each outcome (all p>0.05).
Researchers found the final 24-month failure rate in the phaco+trab group was lower than that in the trab group in both the POAG and PACG subjects. They reported that the impact of adding phacoemulsification to trabeculectomy was similar between eyes with primary open-angle and primary angle-closure glaucoma.
J Glaucoma 2023; Jan 3. [Epub ahead of print].
Winuntamalakul Y, Chansangpetch S, Ratanawongphaibul K, et al.
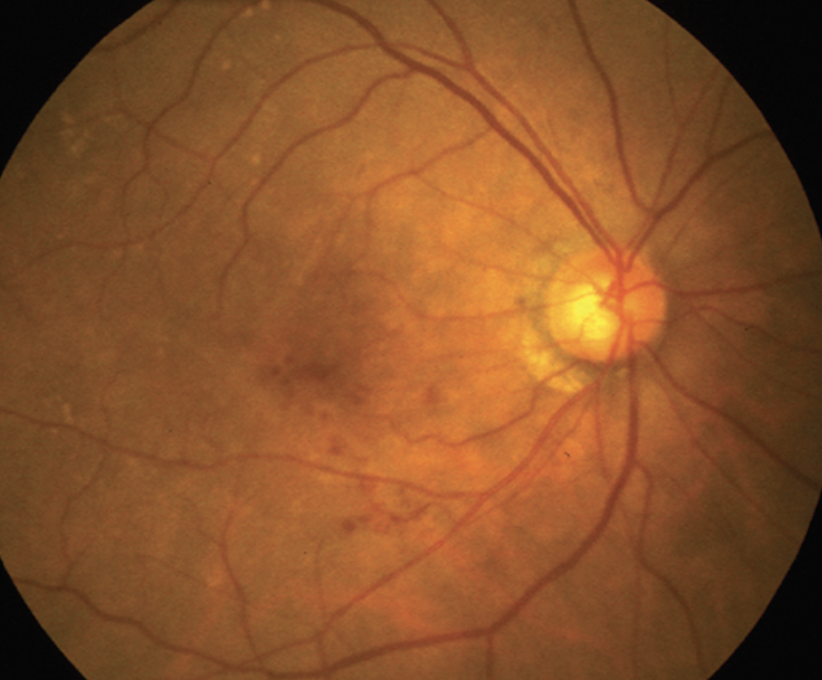
AMD Risk Factors Studied
Researchers in the U.K. reported the prevalence of, and risk factors associated with, age-related macular degeneration in addition to AMD features on multimodal retinal grading, in a multidisciplinary, population-based, longitudinal cohort study of aging.
The Northern Ireland Cohort for the Longitudinal Aging (NICOLA) Study health assessment included stereo color fundus photography (CFP)(Canon CX-1) and spectral-domain optical coherence tomography (Heidelberg Retinal Angiograph + OCT; Heidelberg Engineering). Medical history and demographic information were obtained during a home interview. Descriptive statistics were used to describe the prevalence of age-related macular degeneration and individual AMD features. Multiple regression modeling was used to explore risk factor associations including relationships with AMD genetic risk score.
Retinal images from 3,386 participants were available for analysis. Mean age of the sample was 63.4 (SD, 9.01; range: 36 to 99). Here are some of the findings from the researchers’ report:
• Population weighted prevalence of AMD using color grading in those over 55 years was:
— no drusen: 6 (0.4 percent);
— drusen <63 µm: 15.9 percent;
— drusen 63 to 125 µm: 13.7 percent;
— drusen >125 µm or pigmentary changes: 8.3 percent; and
— late AMD: 1.6 percent.
• Prevalence of AMD features in those over 55 years was:
— OCT drusen: 27.5 percent;
— complete outer retinal pigment epithelium and outer retinal atrophy (cRORA) on OCT: 4.3 percent;
— reticular drusen: 3.2 percent; and
— subretinal drusenoid deposits (SDDs): 25.7 percent.
• The genetic risk score was significantly associated with drusen and cRORA but less so for SDD alone and non-significant for hyperpigmentation or vitelliform lesions.
Researchers concluded that multimodal imaging-based classification provided evidence of some divergence of genetic risk associations between classic drusen and subretinal drusenoid deposits. They added that the findings support a pressing need for a review of current AMD severity classification systems.
Br J Ophthalmol 2022; Oct 10. [Epub ahead of print].
Hogg RE, Wright DM, Quinn NB, et al.
Metformin and AMD Development
Researchers looked at a possible association between metformin use and age-related macular degeneration.
The Diabetes Prevention Program Outcomes Study cross-sectional follow-up phase of a large multicenter randomized clinical trial, Diabetes Prevention Program (1996 to 2001) investigated the association of treatment with metformin or an intensive lifestyle modification vs. placebo with preventing the onset of type 2 diabetes in a population at high risk for developing diabetes. Participants with retinal imaging at a follow-up visit 16 years post-trial (2017 to 2019) were included. Analysis took place between October 2019 and May 2022.
Participants in the study were randomly distributed between three interventional arms: lifestyle, metformin and placebo. Main outcomes and measures included prevalence of AMD in the treatment arms.
Of 1,592 participants, 514 (32.3 percent) were in the lifestyle arm, 549 (34.5 percent) were in the metformin arm and 529 (33.2 percent) were in the placebo arm.
All three arms were balanced for baseline characteristics including age (mean age at randomization, 49 ±9 years), sex (1128 [71 percent] male), race and ethnicity (784 [49 percent] white), smoking habits, body mass index, and education level. Here are some of the findings:
• AMD was identified in 479 participants (30.1 percent); 229 (14.4 percent) had early AMD, 218 (13.7 percent) had intermediate AMD, and 32 (2 percent) had advanced AMD.
• No significant difference in the presence of AMD was reported between the three groups: 152 (29.6 percent) in the lifestyle arm; 165 (30.2 percent) in the metformin arm; and 162 (30.7 percent) in the placebo arm.
• No difference was reported in the distribution of early, intermediate and advanced AMD between the intervention groups.
• Mean duration of metformin use was similar for those with and without AMD (mean: 8 ±9.3 vs 8.5 ±9.3 years; p=0.69).
• In the multivariate models, history of smoking was associated with increased risks of age-related macular degeneration (OR, 1.30; CI, 1.05 to 1.61; p=0.02).
Researchers determined the data didn’t suggest metformin or lifestyle changes initiated for diabetes prevention were associated with the risk of any AMD, with similar results for AMD severity. They added that duration of metformin use also wasn’t associated with AMD.
The investigators noted the analysis didn’t address the association of metformin with incidence or progression of age-related macular degeneration.
JAMA Ophthalmol 2022; Dec 22. [Epub ahead of print].
Domalpally A, Whittier SA, Pan Q, et al.



