It may seem unusual for a surgeon to do cataract surgery only on children. However, in the United States, many pediatric surgeons do so. This fact speaks to how different the medical decision-making and the surgery itself are from the standard adult procedure. The fact that I don’t operate on adults with cataracts does not mean that I do not keep up with the constant flow of innovations being developed in the higher volume and more lucrative adult cataract market. I listen carefully, and I watch intently. With the knowledge and experience I have in the pediatric sphere, I carefully pick and chose techniques that are applicable to the eyes of children. In some cases, techniques are borrowed from both the adult cataract and the adult retina subspecialty areas (See Figure 1).
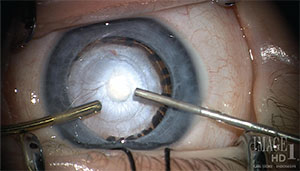 |
| Figure 1. In this case of persistent fetal vasculature, advanced cataract procedures must be combined with an extensive knowledge of applicable vitreoretinal techniques. |
In pediatrics, our first decision is when to operate, if surgery is even indicated at all. Adult cataract surgery is thought of as a refractive procedure that can correct hyperopia, myopia and astigmatism in a precise and predictable manner. Pediatric cataract surgery removes the all-important offset to changes in globe axial length,—the growing and pliable young lens—irreversibly derailing the eye’s natural emmetropization.
Deciding when or whether to operate on a partial cataract in a pre-literate toddler with anisometropia and amblyopia can be daunting. Even if glasses and patching are started first, compliance may be an issue and quantitating improvement from these non-surgical first steps may be nearly impossible. A rush to surgery may be appropriate, but it renders the eye permanently presbyopic and subject to a large and somewhat variable myopic shift over time. Children may be more spectacle-dependent after surgery than before surgery. On the other hand, excessive delays in surgery may worsen form-vision deprivation, and this may drastically change the eye-growth feedback loop, resulting in excessive axial elongation. Admittedly, it is an art. Experience in pediatric assessment is as critical as the acquisition of surgical skills (See Figure 2).
The fact that general anesthesia is usually required also makes pediatric cataract surgery less efficient and more time-consuming. Biometry often has to be done after the child is asleep. Microphthalmia, pre-existing capsular abnormalities and even congenital retinal abnormalities may be found at the surgical exam-under-anesthesia.
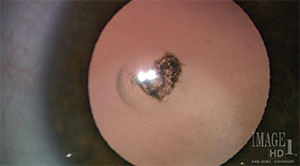 |
| Figure 2. An example of a partial cataract in a toddler. |
Surgeons who underestimate the differences between surgery on a young child and surgery on the elderly may find themselves struggling in the operating room. The lack of a hard nucleus, vastly reduced scleral and corneal rigidity and enhanced posterior vitreous pressure demand a surgical approach that differs in many ways from the adult procedure. After surgery, the surgeon must deal with an increased propensity for postoperative inflammation and capsular opacification; a refractive state that is constantly changing due to growth of the eye; difficulty in documenting anatomic and refractive changes due to poor cooperation and compliance; and a tendency to develop amblyopia.
Pediatric Cataract Pearls
For the procedure itself, here are a few pearls that I have learned over the course of nearly 30 years of operating on children with cataracts.
1. Stitching the wounds is the safest approach. I attribute the poor self-sealing to low corneal rigidity resulting in fish-mouthing of the wound, leading to poor approximation of the internal corneal valve to the overlying stroma. The recommended closure material is a 10-0 synthetic absorbable suture.
2. Bimanual irrigation and aspiration works best. Pediatric cataracts are soft, but they may be “gummy.” Working one instrument against the other can squeeze the cortex into the aspiration port. A curved irrigation cannula can also be used to gently and continuously hydrodissect lens material out from the equator of the bag.
3. When tearing the highly elastic capsules of children, the capsulorhexis force vector must often be directed more toward the center of the pupil in order to control the turning of the CCC edge along a circular path. I re-grasp the capsulorhexis edge frequently and begin with a smaller capsulotomy than desired. Because of the elasticity, the opening will be larger than it appears once the forceps release the capsule flap.
4. Don’t fear the vitrectomy. It is vitreoretinal traction that should be meticulously avoided. A primary posterior capsulotomy and an anterior vitrectomy during intraocular lens implantation in the young child gives the best chance for maintaining a long-term clear visual axis (See Figure 3). Fortunately, and unlike in adults, the incidences of cystoid macular edema and retinal detachment are exceedingly rare after capsulectomy and vitrectomy in children. Anterior segment surgeons are often more accustomed to, and more comfortable with, a limbal (or anterior) approach to the vitreous. However, I prefer to perform these procedures via the pars plana/plicata, with the irrigation cannula remaining in the anterior paracentesis (See Figure 4).
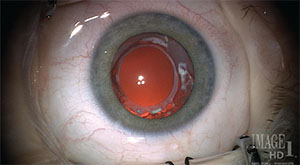 |
| Figure 3. Clear visual axis two years after primary posterior capsulectomy and vitrectomy. The anterior and posterior capsulorhexes are fused. This capsular bag remnant can be re-opened and cleaned of cortical lens regrowth (Soemmering’s ring) when the child is ready for a secondary intraocular lens placement. |
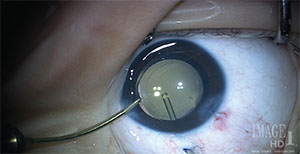 |
| Figure 4. A pars plana approach to the posterior capsule is shown using a 25-ga. vitrector with the irrigation cannula remaining in the anterior chamber. |
5. Intracameral medications are key and can militate against postoperative non-compliance, which is more common in children than adults. After the surgical wounds have been closed, I place intracameral antibiotics in the eye. Currently I am using 0.1 cc of a 50% solution of moxifloxacin (Vigamox, Alcon). Alternatively, 0.05 cc of undiluted Vigamox can be used. There is no preservative in Vigamox, and its safety in the anterior chamber has been studied. I also inject 1 to 2 mg (0.025 to 0.05 cc) of triamcinolone (Triesence, Alcon) intracamerally at the end of surgery in most children. The triamcinolone crystals are visible in the anterior chamber for five to seven days and help control the aggressive early inflammation that can be present in children.
6. For children under 7 months of age, it may be best to leave the eye aphakic and prepare the parents for a secondary IOL in the pre-school or early grade school ages. This approach, when applicable, is less traumatic for the infant eye, and reoperation is less common than when an IOL is inserted this early in life. When I use this approach, I place a Silsoft (Bausch + Lomb) extended-wear silicone contact lens on the eye at the end of surgery without a patch or shield. Since I don’t place any subconjunctival injections, the eye is white and quiet and the image well-focused from the outset. A lens constant of 112.176 is used with biometry to select the Silsoft contact lens power. The initial lens can stay in place for the entire first postoperative month. After a four-week course of postoperative drops has been completed, the parents are taught to remove and clean the contact lens weekly.
7. When placing an IOL in a child’s eye, in-the-bag implantation is strongly recommended, although we have observed that some IOL designs are very well-tolerated in the child’s ciliary sulcus even after many years of follow-up. When using your IOL of choice, it is important to customize the A-constant after analysis of your pediatric results separately from your adult cases.
Surgical management of cataracts in children is markedly different from adults. The eyes are not only smaller because of age but many are also microphthalmic. Decreased scleral and corneal rigidity and increased posterior vitreous pressure make surgical manipulations within these eyes more difficult. The anterior chamber is often unstable; the capsule management requires special considerations. Variability in ocular growth makes selection of an intraocular lens power less certain. Normal childhood behavior may reduce compliance with postoperative instructions, even when the parents are diligent. Finally, examinations of the eye after surgery may be less detailed and precise when cooperation is lacking. The long expected life span after surgery for children also deserves consideration when surgical decisions are made. These special patients are uniquely challenging but caring for them as they mature and grow from children into adults is immensely gratifying. REVIEW
Dr. Wilson is a professor of ophthalmology and pediatrics at the Albert Florens Storm Eye Institute at the Medical University of South Carolina in Charleston. He holds the N. Edgar Miles Endowed Chair in Ophthalmology.
He is the current president of the American Association for Pediatric Ophthalmology & Strabismus (AAPOS) and the council chair for the American Ophthalmological Society. He is a Senior Honor Award recipient from the American Academy of Ophthalmology and a Lifetime Achievement Award recipient from AAPOS. The second edition of his textbook with Rupal Trivedi entitled: Pediatric Cataract Surgery: Techniques, Complications and Management, was published in 2014. Contact him at wilsonme@musc.edu.



