Corneal collagen cross-linking has made significant headway in the United States as a method for halting keratoconus progression. While the procedure is an effective option for the disease, especially for young patients who are quickly progressing, there are some cases in which cross-linking may not be indicated. In this article, specialists describe non cross-linking candidates and methods for managing their keratoconus.
Non Cross-linking Candidates
Kenneth Beckman, MD, FACS, director of corneal services at Comprehensive Eyecare of Central Ohio, and clinical assistant professor of ophthalmology at Ohio State University, says that in his experience, only a few people are unable to undergo cross-linking. He adds, however, that some patients may not need it.
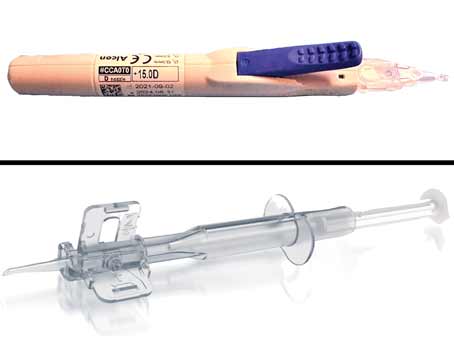
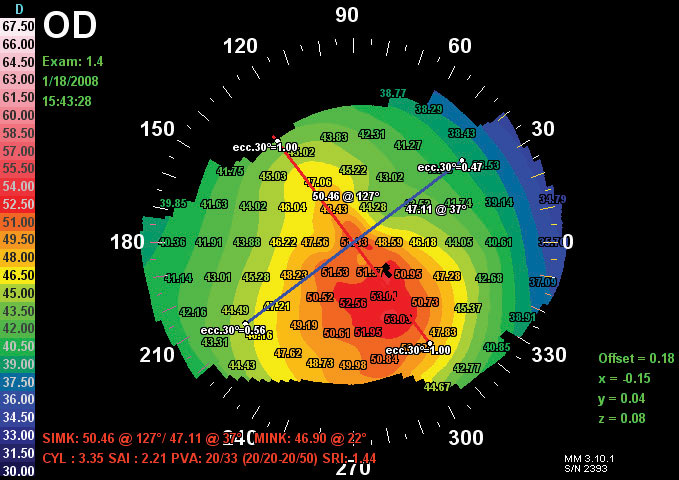 |
All images courtesy of Wuqaas Munir, MD Figure 1. An abnormal topography of a cornea showing keratoconus |
While criteria for a non cross-linking candidate aren’t always clear, here are some special cases in which the procedure is considered unnecessary, or could potentially threaten eye health.
• The stable patient. Doctors say that older, stable patients aren’t good candidates for cross-linking as the procedure, in many instances, becomes unnecessary over time. Anat Galor, MD, MSPH, associate professor of ophthalmology at Bascom Palmer Eye Institute, says that cross-linking is meant to be used in individuals whose keratoconus is progressing. However, “The likelihood of progression goes down with age and most people stop progressing once they get to 35 or 40 years old,” she says. “So cross-linking isn’t needed if someone is 60 years old and has stable disease.”
Julie Schallhorn, MD, MS, assistant professor of clinical ophthalmology at the University of California, San Francisco agrees, commenting that young people are much more likely to progress, and at a much more rapid rate. She shares why doctors think this occurs. “Cross-linking essentially bonds collagen fibrils and, as you age, through natural exposure to UV sunlight, the collagen in your cornea stiffens and is naturally cross-linked.”
• Very thin cornea. Dr. Schallhorn says that if the patient’s cornea is too thin, he can’t undergo cross-linking since there’s a risk of damaging the corneal endothelium. “There’s a minimum corneal thickness that you need in order to be able to cross-link,” Dr. Schallhorn says. “Four hundred microns is what they used in the FDA-approval studies for Avedro, which was recommended based on studies looking at endothelial damage from cross-linking.” Wuqaas Munir, MD, associate professor of ophthalmology and visual science, and associate program director for the residency program at the University of Maryland School of Medicine, explains that the current thinking is that the application of UV-light could potentially damage the endothelium during the cross-linking procedure if the cornea isn’t thick enough. “So in this case, a patient who wouldn’t qualify [for cross-linking] would have too advanced a form of the disease where the cornea has become too thin,” he says.
Though doctors note the potentially harmful effects of performing cross-linking on a patient whose cornea is less than 400 µm thick, Dr. Beckman emphasizes that this is just the recommended guideline for minimum thickness. It’s not clear-cut as to whether damage is necessarily done to the endothelium if the cornea is below that threshold. “Some have experienced damage when the cornea was thicker than
400 microns, and there are plenty of cases of thinner corneas that haven’t had damage,” he says.
While a thin cornea may be a sign that a patient isn’t a good cross-linking candidate, doctors are investigating different techniques to decrease the risk of harm to the endothelium. This includes changing the intensity of the UV light, altering the duration of treatment, putting a contact lens over a thin cornea to reduce UV-light penetration, and using hypotonic riboflavin (Photrexa Viscous, Avedro) to swell the cornea.
• Scarred cornea. “Corneal scarring could be another issue; but that usually ties in with thinning,” says Dr. Munir. “A patient with significant scarring is usually someone whose cornea is so thin that they can’t be treated with cross-linking.” If the cornea is scarred, especially centrally and significantly, Dr. Beckman says that’s going to limit vision. He says a transplant may ultimately be needed in that case, as there may be no visual benefit from cross-linking.
• Ocular surface disease. “A person with bad ocular surface disease—like those with a history of herpes or severe dry eye—may not be able to have a cross-linking procedure as these conditions make healing difficult,” notes Dr. Beckman. “Herpes patients have trouble re-epithelializing, and in cross-linking you remove the epithelium. Also, ultraviolet light may trigger a herpes flare-up.” Dr. Beckman notes, however, that this isn’t an absolute contraindication, and says that the physician has to weigh the risks and benefits.
• Inability to sit still or fixate. Dr. Beckman adds that a cross-linking procedure could be difficult if a patient is unable to sit still. “For some of those patients, physicians may consider doing the procedure under sedation or even general anesthesia, which has its own risks,” he says. “Patients that are very young or have cognitive issues may require this. Fortunately, it’s very rare.” However, Dr. Beckman notes that this isn’t necessary in every one of these cases. He points out that he has treated young patients and patients with Down syndrome without using sedation, and he reports that they’ve done very well.
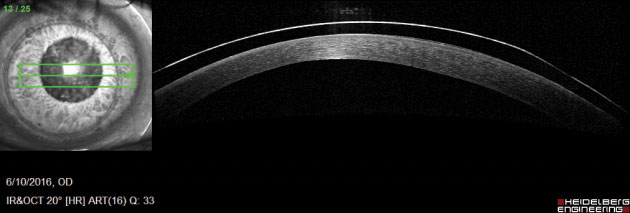 | 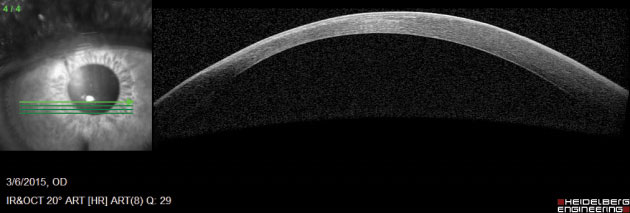 |
| Figure 2. Left: OCT of a keratoconic cornea fitted with a contact lens. Right: OCT of a keratoconic cornea. | |
Management Options
“As of now, the only thing that can change the course of [keratoconus], or halt its progression, is cross-linking,” says Dr. Munir. However, there are devices and techniques for managing various stages of the disease when cross-linking isn’t the best option. Of course, it’s important to note that many of these options aren’t exclusively used in non-cross-linking candidates; they’re frequently employed before, after and in conjunction with cross-linking.
• Soft lenses. The purpose of contact lenses is to help the patient see, says Dr. Munir. “Since keratoconus causes the cornea to steepen, contact lenses aim to negate that steepness and improve the optics of the eye,” he explains. “To do this, the lens sits on top of the cornea and when light penetrates the eye it hits a more uniform surface.” With that in mind, Dr. Schallhorn says that soft lenses are great for people with regular astigmatism who have little change in the contour of the cornea. “If you have mild keratoconus and can refract well in glasses, then a soft lens generally works,” she says. “But for a patient with significant amounts of irregular astigmatism, [someone with moderate to severe keratoconus], he or she won’t be able to wear a soft lens.”
“The problem with a soft lens is that it’s soft,” muses Dr. Munir. “It drapes over the cornea and has very limited ability to overcome shape changes. If you have a steep cornea, the soft lens will follow the shape of that steepness and you won’t get a smooth contour anymore.” Justin Sherman, OD, an optometrist at Philadelphia Eye Associates, outlines another shortcoming of soft lenses. “In my experience, soft-lens patients tend to overwear their lenses,” he says. “And that comes with the associated complications.”
• Rigid lenses. “Rigid gas-permeable small-diameter contact lenses work very well for [more advanced cases of] keratoconus because they cancel out the irregular astigmatism of the cornea,” says Dr. Schallhorn. Dr. Munir says RGPs aren’t limited as much by the shape of the cornea and can be used in steeper forms of keratoconus to achieve better optical quality. And Dr. Sherman notes that being able to change the optical zone sizes and peripheral curve systems [with the use of an RGP], makes it possible to fit a wide variety of cones. “One of the best qualities of RGP lenses is the significantly lower rates of overwear and infection relative to soft lens designs,” he says.
Dr. Sherman adds, however, that these lenses become less effective in patients with severe, more peripheral cones that produce significant differences in peripheral corneal elevation. Dr. Schallhorn agrees. “The problem with RGP lenses is that there’s kind of a limit as to how steep your cornea can be to wear [them],” she says. “They’re also kind of tricky to fit. You need to be working with an optometrist who’s good at fitting RGP’s, which is tough because you’re basically fitting on top of a mountain.”
• Piggybacking. “Piggybacking a rigid lens on a soft one used to be considered a great way to provide comfort to a patient who can’t comfortably wear their RGPs any longer,” says Dr. Sherman. “However, the need for piggybacking has been dramatically reduced with the advent of irregular cornea RGPs, scleral lenses and hybrid-lens designs. This is great because the complexity of caring for two different lens types with different solutions and replacement schedules would often lead to patients misusing their contact lenses in some capacity.” Dr. Schallhorn outlines another disadvantage to the technique. “The two-lens combination can cause a lot of corneal hypoxia and could cause corneal neovascularization,” she says. “Those vessels put the patient at higher risk for transplant.” However, Dr. Sherman notes that there are cases in which patients manage their piggybacking technique well and are very happy.
• Hybrid lenses. Dr. Munir says that hybrid lenses provide the optical advantage of the rigid lens but the comfort of a soft lens. However, while Dr. Sherman acknowledges the optical and comfort advantages, he outlines a few disadvantages. “[Hybrid lenses] are similar to RGPs in that they begin to misbehave when patients have more peripheral disease,” he says. “They’re probably the most difficult for patients to handle. The edge of the lens has to be pinched to remove it, but many patients have a difficult time knowing where the GP optic ends and the soft skirt begins. Difficulty with insertion and removal is the most common reason I have patients drop out of hybrid-lens wear.” He adds that hybrid lenses are also the most expensive design.
• Scleral lenses. “Scleral lenses have revolutionized treatment options,” says Dr. Beckman. “No matter how distorted the cornea may be, if it’s optically clear—meaning there’s no central scar—then you can fit almost any cornea with a scleral lens and get good vision.”
Dr. Beckman says the advantages of scleral lenses include the ability of the lens to vault in front of the cornea without touching it. He says the lens creates a smooth round optical surface, which corrects vision. “Since the lens doesn’t rub on the cornea, scleral lenses are good for patients with dry eye,” he notes. “The patient’s tear film fills in the gap between the lens and cornea, so the surface of the cornea is kept moist as it constantly bathes in liquid.”
Dr. Sherman agrees that scleral lenses can be very therapeutic for ocular-surface disease issues, which many keratoconus patients have. He says that scleral lenses are a great choice for patients with severe, more peripheral cones. “These lenses vault the cornea entirely and are supported by a haptic that lands on the conjunctiva,” he explains. “Because the conjunctiva is much less sensitive than the cornea, these lenses are exceptionally comfortable, so long as they match the patient’s scleral profile. They also have extremely low rates of complication and infection.”
Due to advancements over the past few years, Dr. Munir says that in many cases, a steep cornea, which previously may not have been manageable with a rigid lens, can now be fit with a scleral lens. However, Dr. Munir acknowledges a few disadvantages. “[Scleral lenses are] very large and potentially more uncomfortable than a standard RGP,” he says. “It can be difficult to insert and remove scleral lenses because of the large size. The patient instruction is more difficult and it’s harder for patients to build up a tolerance, in terms of lack of comfort.”
Doctors say generic scleral lenses work for almost everybody, but there are still extremely advanced cases of keratoconus where the cornea is too steep for a generic lens. Due to a more recent development in scleral-lens technology, however, doctors say that steep cones can now be fit using custom scleral lenses such as
BostonSight’s PROSE and EYEprint’s EyePrintPRO. “[These are both] types of scleral lenses that allow you to customize the lens to fit the contour of the patient’s cornea and therefore fit people with very irregular corneas,” Dr. Galor says. Dr. Schallhorn describes the options: “PROSE is a custom-made scleral lens that can vault over almost any cone,” she says. “EyePrintPRO is another custom scleral lens in which you take a mold of the corneal shape and then make a lens based on that.”
• Intacs. “The goal is to insert Intacs to make the cornea more regular and improve contact lens comfort,” says Dr. Galor. “A good candidate for intrastromal rings is an individual who has sufficient corneal thickness and contact-lens intolerance.”
Dr. Beckman says the placement of Intacs may provide better spectacle vision and better-uncorrected vision. He outlines a scenario in which Intacs may be used in order to decrease dependence on contacts. “If progression has stopped and there’s still significant residual astigmatism, patients may try glasses or contacts,” he says. “Often, they get good vision with both but, at other times, they may only get good vision with contacts. For these patients Intacs may be considered.”
Due to advancements in contact-lens technology over the past decade, Dr. Sherman says that fewer and fewer Intacs segments are being implanted. Dr. Galor notes, however, that the world of corneal rings is more varied outside of the United States. “In Europe, they have many different types of intrastromal rings and they’ve developed really sophisticated algorithms that customize the length, thickness, number and location of the rings to counteract a particular shape of the cornea,” she says.
Transplants
“People that have really advanced keratoconus who are no longer able to fit into generic scleral lenses, who can’t afford or are unable to get custom lenses (which physicians say are, unfortunately, very expensive), or have a history of hydrops with scarring, are people we’re doing transplants on,” says Dr. Schallhorn. She adds that a patient having an episode of hydrops already has extremely advanced keratoconus, and therefore a very thin cornea, which makes for a poor cross-linking candidate.
• DALK. Since keratoconus doesn’t affect the endothelium, Dr. Munir says deep anterior lamellar keratoplasty is an option. “The endothelial cells are what we consider one of the primary sources of transplant rejection,” says Dr. Munir. “However, we can do a deep anterior lamellar keratoplasty, which will replace everything but the endothelium.” In DALK, the corneal stroma is removed but Descemet’s membrane and the endothelial cells remain. “The risk of rejection is much lower with this type of procedure than it is with a full-thickness penetrating keratoplasty in which the stroma and endothelium are replaced by donor tissue,” Dr. Munir shares.
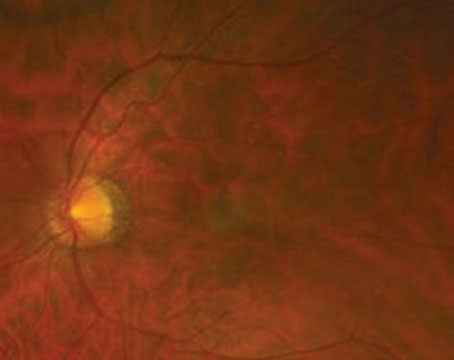
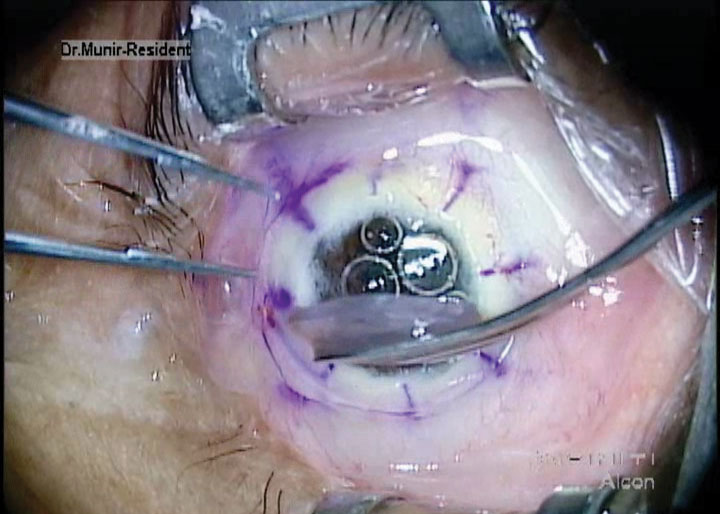 |
|
|
Dr. Beckman says there are pros and cons to DALK. “The advantages are that you’ve done a procedure without having the eye completely open—just a thin membrane remains—so there’s less risk intraoperatively,” he says. “And since there’s less risk of graft rejection, you could potentially get the patient off steroids quicker. However, disadvantages include the learning curve. Not every doctor performs DALK. It’s a long procedure that’s technically more difficult than PK, and there’s always the possibility of popping through Descemet’s and the endothelium and having to convert to a PK. If the patient has endothelial disease or a distorted cornea that’s too thin and the endothelium decompensates, then DALK wouldn’t be an option, you’d have to do PK.”
• Corneal transplant. “Sometimes, if there’s a lot of scar tissue, as in a patient who has very advanced keratoconus and a thin cornea, you can’t perform DALK,” Dr. Munir says. “In that case we do a PK. The risk with PK is that you have a little more of a chance for rejection since you’re removing the endothelium.”
Dr. Schallhorn notes a few instances where a PK would be indicated. “I find that for patients who have a lot of endothelial scarring from an episode of hydrops, many times you just blow out the area of the old scar with DALK and end up having to do PK,” she says.
Dr. Galor says there are possible long-term concerns for transplant patients. “One issue with DALK and PK is that the integrity of the cornea is never as strong as the native cornea,” she says. “As such, if patients experience trauma to the eye, even years after transplantation, they’re at risk for graft dehiscence, in which the area of the scar opens.” However, she notes that outcomes are good after full-thickness corneal transplants for keratoconus, compared to other indications.
Outlook: Positive
Ultimately, Dr. Schallhorn says cross-linking is a very exciting technology, especially for younger patients. As for older patients, she says the jury is still out regarding who’s considered a good candidate for cross-linking and who’s at risk for progression. “That’s something people need to address,” she says. “However, I think that referring people to optometrists who are skilled scleral-lens fitters and can get good refractive correction can really change the life of a person who has keratoconus.” REVIEW
Drs. Schallhorn and Beckman are consultants for Avedro. Drs. Galor, Munir and Sherman report no financial interests.