Pairing intravitreal triamcinolone acetonide with laser to treat diabetic macular edema results in a doubling of improvement in vision by 10 letters or more compared with laser alone, according to an Australian study. The prospective, double-masked, randomized, placebo-controlled study at the Save Sight Institute in Sydney tested the 24-month treatment outcomes in 84 eyes of 54 patients. Forty-two eyes were randomly assigned to receive IVTA plus laser and 42 randomly assigned to receive laser treatment alone. Primary end point data were available for 71 eyes (84.5 percent) at 24 months, with the last visual acuity observation carried forward for the remaining eyes. Best-corrected logarithm of minimum angle of resolution, visual acuity and central macular thickness by optical coherence tomography were measured after laser treatment preceded by either IVTA or sham. The primary outcome was the proportion of eyes with improvement in visual acuity of 10 letters or more at 24 months. The secondary outcomes were mean visual acuity, requirement for further treatment, change in CMT and adverse events.
At 24 months, improvement of 10 letters or more was seen in 15 (36 percent) of 42 eyes treated with IVTA plus laser compared with 7 (17 percent) of 42 eyes treated with laser only (p=0.047; odds ratio, 2.79; 95 percent confidence interval, 1.01 to 7.67). There was no difference in the mean CMT or mean logMAR visual acuity between the two groups. At least one retreatment was required in the second year of the study in 29 (69 percent) of 42 IVTA plus laser-treated eyes compared with 19 (45 percent) of 42 laser-only eyes (p=0.187). Cataracts were removed from 17 (61 percent) of 28 phakic IVTA plus laser-treated eyes versus none of 27 laser-only eyes (p<0.001). Treatment for elevated intraocular pressure was required in 27 (64 percent) of 42 IVTA plus laser eyes compared with 10 (24 percent) of 42 laser-only eyes (p<0.001).
Gillies MC, McAllister IL, Zhu M, et al.
Risk Factors for Progression in Treated Glaucoma
Peak intraocular pressure is a better predictor of visual field progression than IOP mean or IOP fluctuation, suggests new research. In a study to determine IOP-dependent and IOP-independent variables associated with progression in treated glaucoma, researchers at the Einhorn Clinical Research Center in New York launched a retrospective cohort of the Glaucoma Progression Study. Consecutive, treated glaucoma patients with repeatable VF loss who had eight or more VF examinations of either eye using the 24-2 SITA-Standard, Humphrey Field Analyzer II, between 1999 and 2009, were included. Progression was evaluated using automated pointwise linear regression. Evaluated data included age, sex, race, central corneal thickness, baseline VF mean deviation, mean follow-up IOP, peak IOP, IOP fluctuation, a detected disc hemorrhage and presence of beta-zone parapapillary atrophy.
Researchers evaluated 587 eyes of 587 patients (mean age, 64.9 ±13 years). The mean number of VFs was 11.1 ±3, spanning a mean of 6.4 ±1.7 years. In the univariable model, older age (odds ratio: 1.19 per decade; p=0.01), baseline diagnosis of exfoliation syndrome (OR: 1.79; p=0.01), decreased central corneal thickness (OR: 1.38 per 40 µm thinner; p<0.01), a detected disc hemorrhage (OR: 2.31; p<0.01), presence of beta-zone parapapillary atrophy (OR: 2.17; p<0.01), and all IOP parameters (mean follow-up, peak, and fluctuation; p<0.01) were associated with increased risk of progression. In the multivariable model, peak IOP (OR: 1.13; p<0.01), thinner central corneal thickness (OR: 1.45 per 40 µm thinner; p<0.01), a detected disc hemorrhage (OR: 2.59; p<0.01) and presence of beta-zone parapapillary atrophy (OR: 2.38; p<0.01) were associated with progression.
De Moraes CG, Juthani VJ, Liebmann JM, et al.
Intravitreal Anti-VEGF Improves VA with Minimal Side Effects
Results from a new study show that intravitreal ranibizumab delivers a significant improvement in visual acuity and central retinal thickness with minimum side effects. Researchers from Vitreous-Retina-Macula Consultants of New York and LuEsther T. Mertz Retinal Research Center in New York launched a prospective interventional case series, evaluating patients with central retinal vein occlusion who were administered intravitreal ranibizumab 0.5 mg at baseline and monthly for two additional doses. Thereafter, the patients were given additional ranibizumab if they had macular edema by OCT, leakage during fluorescein angiography or any intraretinal hemorrhage.
Thirty-five eyes of 35 patients at baseline had a mean visual acuity of 44.2 Early Treatment of Diabetic Retinopathy Study letters and a mean central macular thickness of 638 µm. At 12 months, mean visual acuity of 32 eyes improved by 16.5 letters and macular thickness decreased to 164 µm (p<0.001 vs. baseline for each). At 24 months, mean visual acuity of 24 eyes improved by 17.8 letters and macular thickness was 263 µm (p<0.001 vs. baseline for each). Patients received an average of 10.2 injections during the first year and 6.6 injections during the second year. No cases of endophthalmitis, retinal detachment or neovascularization were observed.
Chang LK, Spaide RF, Klancnik JM, et al.
“Twist Method” Allows Safer Sutureless Vitrectomy
A gently twisting insertion maneuver during trocar insertion could significantly reduce the intraocular pressure elevation to allow a safer sutureless vitrectomy. An interventional prospective study conducted at numerous sites in Taiwan and New Zealand evaluated two trocar insertion methods—direct insertion and gently twisting insertion—using a 25-ga. vitrectomy system (Alcon). The methods were used to create a scleral wound using trocar blade and trocar cannula in freshly enucleated porcine eyes. The IOP changes induced by the procedures were recorded with a pressure transducer connected to the posterior chamber by direct cannulation.
Fourteen porcine eyes were studied in each group. During insertion, the mean highest IOP rise (peak IOP rise) was 63.9 ±25.5 mmHg in the direct insertion group compared with 30.3 ±16.9 mmHg in the twisting insertion group (p=0.001). During insertion, the mean of average IOP rise in the direct insertion group was 39.9 ±16.5 mmHg, compared with 21.5 ±8.9 mmHg in the twisting insertion group (p=0.002). The total time needed to complete the procedure in the twisting insertion group was significantly longer than that in the direct insertion group (43.3 ±21.8 vs. 14.9 ±8.1 seconds, p=0.0003).
Wu PC, Tiong IS, Chuang YC, Kuo HK.
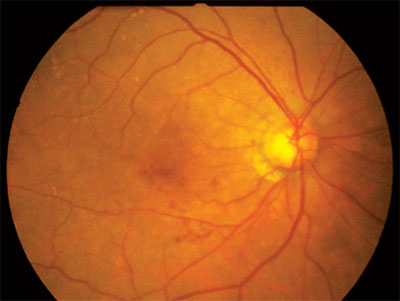 |
| Simple changes in lifestyle could significantly reduce the risk of AMD. |
A change in lifestyle could reduce the risk of age-related macular degeneration as much as three fold, suggests new research from Department of Ophthalmology and Visual Sciences at the University of Wisconsin, Madison. To investigate the relationships between lifestyle behaviors of diet, smoking and physical activity and the subsequent prevalence of AMD, researchers reviewed the 1,313 participants (aged 55 to 74 years) in the Carotenoids in Age-Related Eye Disease Study, an ancillary study of the Women’s Health Initiative Observational Study. Scores on a modified 2005 Healthy Eating Index were assigned using responses to a food frequency questionnaire administered at baseline of the Women’s Health Initiative Observational Study (1994 to 1998). Physical activity and lifetime smoking history were queried. An average of six years later, stereoscopic fundus photographs were taken to assess the presence and severity of AMD; it was present in 202 women, 94 percent of whom had early AMD, the primary outcome.
In multivariate models, women whose diets scored in the highest quintile compared with the lowest quintile on the modified 2005 Healthy Eating Index had 46 percent lower odds for early AMD. Women in the highest quintile compared with those in the lowest quintile for physical activity (in metabolic energy task hours per week) had 54 percent lower odds for early AMD. Although smoking was not independently associated with AMD, having a combination of three healthy behaviors (healthy diet, physical activity, and not smoking) was associated with 71 percent lower odds for AMD compared with having high-risk scores (p<0.001). These results suggest not only a better quality of life, but also a potential lowering of the social and economic costs of AMD to society.
Mares JA, Voland RP, Sondel SA, et al.



