Few would dispute that femtosecond laser technology is here to stay. However, many would debate its readiness to replace existing technologies in specific surgical situations—partly on grounds of cost, and partly on grounds of not yet having proven its superiority over other approaches, especially in terms of visual outcomes.
One area in which femtosecond lasers are increasingly being used is corneal transplantation. Here, four experts share their thoughts on the current status of this technology as a tool for use in penetrating keratoplasty and the numerous partial-transplant options that have been developed in recent years.
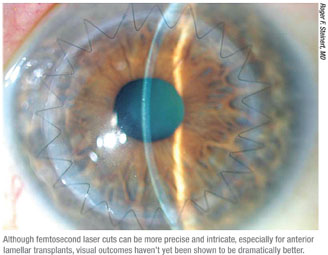 |
There’s no question that a computer-guided laser can trump manual surgery in some respects, including precision and reproducibility. But does that make the laser a superior choice for performing a corneal transplant? Opinions are mixed.
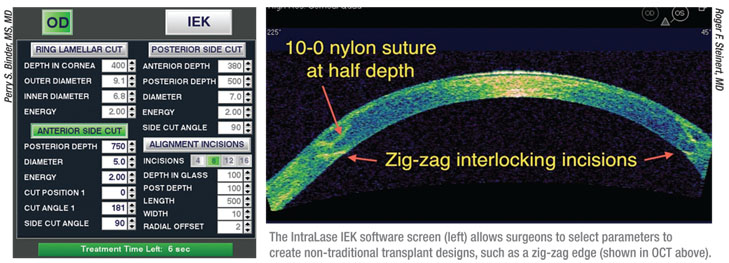
One advantage the laser possesses is the ability to create complex side-cut patterns such as the top hat, mushroom, zigzag, flask, zig-square and Christmas tree. “This software was introduced in 2006,” notes Perry S. Binder, MS, MD, clinical professor in the Gavin Herbert Department of Ophthalmology at the University of California, Irvine, and a medical monitor for AMO. “About 20 such side-cut patterns have now been designed and tested. These more complex cuts allow the donor tissue to fit very nicely into the recipient, which allows you to place less tension on sutures while providing more surface area for wound healing. Other designs include grafts that are octagonal, for example, rather than round, to prevent the graft from rotating. Intralase has also created an option that etches the locations at which the surgeon should place the suture—so-called alignment incisions.”
“It’s clear that we can make very accurate keratoplasty incisions with the femtosecond laser—overlapping incisions that can’t be made manually, such as tongue-in-groove,” says William W. Culbertson, MD, director of the Bascom Palmer Eye Institute Laser Vision Center, and professor of ophthalmology at the University of Miami Miller School of Medicine. “We believe that doing so creates a stronger incision, for several reasons. One, the more complex incision creates greater surface area for healing. Two, using the femtosecond laser appears to stimulate the healing process more than a manual cut. And three, the more complex cuts are often overlapping or interdigitating incisions like the zigzag or mushroom incisions, and the shapes help to make the tissues fit together more tightly.
 |
Dr. Binder agrees. “The original hope was that this type of modification would result in less postop astigmatism,” he continues. “The good news is that the goal of more rapid wound healing, more rapid suture removal and faster vision recovery has been realized. Almost all of the published papers have demonstrated those things. The bad news is that with sutures out, over time, most of the studies have found no difference in astigmatism. I think there are other things we need to look at to make penetrating grafts produce better visual results.”
Thomas John, MD, clinical associate professor at Loyola University at Chicago and editor of several books on corneal transplantation, acknowledges that the laser can do some things more accurately than a surgeon using manual techniques, but doesn’t see the laser as a superior alternative for full-thickness transplants at the present time. “The femtosecond laser has no significant advantage, except that the wound seems to heal somewhat faster, and it increases speed and reproducibility,” he says. “The downside is, just like manual keratoplasty, it induces corneal astigmatism. Corneal transplantation isn’t entirely about earlier suture removal; it’s primarily about vision. Can the patient see better? Is the final outcome better?”
Roger F. Steinert, MD, Irving H. Leopold Professor and Chairman, and director of the Gavin Herbert Eye Institute at the University of California, Irvine, has studied the capabilities of the laser as a transplantation tool extensively. He says his data has shown that the laser gives better results in terms of astigmatism and more rapid recovery of a high level of vision. “That’s been true whether we’ve done a full-thickness penetrating transplant or a deep anterior lamellar keratoplasty,” he notes. “Our original study produced very consistent data regarding full-thickness transplants, and those data have held up during two years of follow-up.
“However,” he continues, “not every center that has studied this has found an advantage to using the laser. My personal viewpoint is that this is an issue of methodology, rather than any fundamental issue with the laser. I think that if surgeons follow the protocols that we’ve outlined, they generally will get better results with the laser. In any case, we’re continuing to accumulate data, to find out what happens when the sutures come out, for example, and what will happen over a longer period of time.”
 |
Anterior Lamellar Keratoplasty
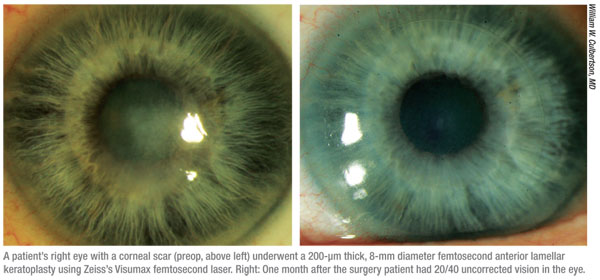
In general, the femtosecond laser seems to be advantageous when transplants involve a relatively thin button of anterior corneal tissue. However, issues arise when the cuts go deeper, because of changes in corneal tissue, issues with the laser’s ability to cut effectively at greater depth, and concerns about harming Descemet’s membrane.
Dr. John sees more reason to use the laser when performing certain partial-thickness transplants than when performing PK. “Partial thickness procedures can be divided into two major groups: anterior lamellar keratoplasty, or ALK, and posterior lamellar keratoplasty, or PLK,” he notes. “The laser is especially useful in the ALK subset. In the PLK group, it depends on the technique.”
Dr. John notes that anterior lamel-lar keratoplasty includes a whole gamut of procedures which are distinguished in part by the depth of the tissue replacement. “The depth largely determines whether the laser is a safe option to use,” he says. “If you’re replacing a very superficial scar, either a microkeratome or laser can be used to cut the patient’s cornea and donor cornea.”
“Currently,” says Dr. Binder, “some surgeons are trying to use the femtosecond laser to perform deep anterior lamellar procedures by making a deep pass with the laser and then removing a thick piece—300 to 350 µm of a specified diameter of the anterior cornea—and then replacing that with a donor button, with or without a PTK treatment to the surface. A second approach is to do exactly the same thing, but inject air under the remaining 100 to 150 µm of stroma—the so-called ‘Anwar’s Big Bubble’ technique.”
Dr. Culbertson notes that the laser can be helpful when using the Big Bubble technique. “When performing Descemet’s anterior lamellar keratoplasty, or DALK, we use the femtosecond laser to make a very deep side cut in the recipient and donor corneas,” he explains. “Then we use the Big Bubble technique to manually dissect Descemet’s membrane away from the stroma. The combination of laser and manual allows us to create a more complex edge like the zigzag, and then get a smooth interface without having to use the laser too close to Descemet’s membrane, which would risk harming the endothelium.”
Dr. Binder says a new way to separate stroma from Descemet’s membrane is under development by Jaime Martinez, MD, also at AMO. “To make the smoothest possible dissection when performing DALK, surgeons are using an injection of air to push Descemet’s membrane away from the cornea,” he says. “Dr. Martinez’s idea was to use the gases created by the laser during the dissection to help dissect Descemet’s away from the stroma. The result is a system in which we make several passes at the same depth. Dr. Martinez calls this the ‘small bubble technique.’ It’s another approach for creating smooth dissections in the posterior cornea that we didn’t have three years ago.”
Making Deep Beds Smoother
Dr. Binder acknowledges that issues have arisen when using the femtosecond laser to make deep cuts. “Our group is studying this right now,” he says. “The corneal anatomy becomes less compact the more posterior we go. As a result, any cuts with a laser made below 220 µm are more rough and irregular than cuts in the anterior because the laser beam focus is reduced. Three or four years ago when microkeratomes were being used to cut in the posterior cornea they created much smoother resections than the femtosecond lasers. Whether that led to better vision, I don’t know—no one has done that study.
“Since then, surgeons have been looking for ways to create smoother posterior beds,” he continues. “Two major advances have taken place. First, lasers have been developed that create more focal energy, putting the spots closer together, so by adjusting the spot and line separation, the surgeon can create a smoother dissection, even when making deeper cuts.”
Dr. John agrees that the laser itself no longer has a problem cutting deeper in the tissue. “That issue has been resolved,” he says. “The new lasers can go much deeper without any problem. Of course, that’s a separate issue from not going too close to Descemet’s membrane.”
 Dr. Binder says the second advance that’s helping make a smoother bed is that some surgeons are now doing DALK in two steps. “First, they debulk the cornea by using the laser to remove a button that only goes partway down, leaving about 100 µm of tissue,” he explains. “Then they reapply the laser to remove the rest. Now the laser only has to go through 100 µm of tissue instead of 500 µm. That makes the laser more efficient, so that second pass can create a smoother bed. We’ve done laboratory studies that show that this approach works quite well.”
Dr. Binder says the second advance that’s helping make a smoother bed is that some surgeons are now doing DALK in two steps. “First, they debulk the cornea by using the laser to remove a button that only goes partway down, leaving about 100 µm of tissue,” he explains. “Then they reapply the laser to remove the rest. Now the laser only has to go through 100 µm of tissue instead of 500 µm. That makes the laser more efficient, so that second pass can create a smoother bed. We’ve done laboratory studies that show that this approach works quite well.”
Dr. Binder believes that despite its limitations, the laser’s advantages in anterior lamellar keratoplasty are significant. “It’s true that the way we currently make deep cuts is not as good as we’d like it to be,” he acknowledges. “However, as far as lamellar dissection, every single dissection done with a femtosecond laser is smoother than freehand. And every dissection done anterior to 200 µm is also smoother than with a microkeratome. That will only improve as the laser technology advances and we switch to making two passes instead of one and/or refine laser energy delivery.“
Posterior Transplants
“The next goal for transplants with femtosecond lasers is to eliminate the need for blades or trephines for the more popular posterior segment procedures,” notes Dr Binder. “This use was stimulated by the work of an ophthalmologist in the Netherlands, Dr. Gerrit Melles, who introduced Descemet’s stripping endothelial keratoplasty, Descemet’s stripping automated endothelial keratoplasty, Descemet’s membrane endothelial keratoplasty and other variations. Some surgeons are using the femtosecond laser to remove the posterior cornea from both donor and recipient, to try to get better posterior wound apposition without damaging the endothelium.”
“When the endothelium is suboptimal, the most popular transplant technique is DSAEK,” notes Dr. John. “But the best technique, in my opinion, is DMEK, in which we only replace Descemet’s membrane with healthy donor endothelium. That’s what I do exclusively, and with DMEK, there’s no advantage to using the laser. Cutting close to Descemet’s membrane with the laser is problematic; if it gets too close, there’s a good chance it will damage the endothelium. So the laser is not a good option.
“With DSAEK, you can use the laser to prepare the donor tissue, because in DSAEK the donor button includes both Descemet’s membrane and stroma,” he explains. “When you cut the stroma with the laser, it definitely does a better job than a person can do manually. So if you prepare the donor button using a laser, the donor part of the interface will be of higher quality. Of course, the other 50 percent of the interface is part of the patient’s cornea, and removing Descemet’s membrane is currently done manually. That part of the procedure is the same for DSAEK or DMEK.”
Dr. Culbertson believes that so far, at least in the clinic, the laser has not worked out well for posterior transplants. “The problem has been cutting the donor button for the DSEK procedure with the laser,” he explains. “There are two issues.
“First, the posterior cornea has less-compact tissue than the anterior stroma, and the lasers currently available in the clinic don’t cut that tissue very smoothly,” he says. “Consequently, the surface of the tissue that results is rougher than desirable.” However, he notes that advancing technology may solve this problem. “I recently attended the International Congress of Femtosecond Lasers in Dana Point, Calif., where I saw a demonstration of an advanced femtosecond laser guided by OCT that produces a greater quantity of smaller bubbles, presented by Holger Lubatschowski of Germany,” he says. “That laser was able to make a very smooth posterior interface for doing DSEK.
“The second problem has to do with the way the laser is coupled to the eye—the applanation device,” he continues. “With the Intralase it’s a flat device that flattens the cornea, which deforms the posterior cornea a lot more than the anterior cornea; it creates round folds in the posterior tissue. If you cut a flat surface onto something that’s got circular folds in it, when you unflatten it you’ll find that you now have round folds in the bed you’ve created. This isn’t a factor when making LASIK flaps or doing anterior lamellar keratoplasty, because the applanation mostly has this effect in the posterior side of the cornea. But it’s an issue when you try to make an interface in the posterior cornea for either deep lamellar keratoplasty or the DSEK procedure.”
Could a curved applanator solve this problem? “There are two types of applanation being done by the five femtosecond lasers that are out there,” observes Dr. Binder. “Three of them use flat applanation, two of them use curved applanation. We expected to get more predictable cuts with the curved applanation than with the flat, but it turns out that some of the procedures are not demonstrating that. That’s another reason it makes sense to debulk 300 µm of tissue and then make another 100-µm pass. You eliminate some of those concerns.”
Dr. Culbertson says he doesn’t know of anyone right now who’s making tissue for DSEK posterior lamellar keratoplasty with the laser, because of these problems. Dr. Steinert agrees. “Today, many people do not see the laser as having an advantage for preparing DSEK buttons compared to using a microkeratome, with current techniques,” he says. “We’re currently working on a better way of doing that dissection with the laser and getting very favorable results, but it’s still a little too early to share that approach; we’re still working out the kinks in the technique. We hope to have results to report by this fall.”
Other Pros and Cons
Aside from these issues, surgeons see other advantages and disadvantages to using the laser. Advantages include:
- More sutureless wounds. “We often perform a lamellar transplant involving 100 to 250 µm of anterior cornea without using sutures,” says Dr. Culbertson. “We lay the transplanted tissue on the recipient’s cornea as if it were a LASIK flap. The laser is useful here because it’s hard to construct a lamellar keratoplasty manually in which the margins fit as precisely as they do with the femtosecond laser. The close match of the recipient resection with the donor tissue architecture and dimensions results in a very good fit. We just put a contact lens on the eye and it heals.”
- Precision eye bank preparation. Dr. Binder notes that many eye banks are also using the femtosecond lasers to prepare donor buttons. “If the surgeon has a femtosecond laser, he can tell the eye bank the type of cut he wants and the exact parameters,” he says. “Most eye banks today have an Intralase laser, although I’m aware of another new femtosecond laser that’s being designed just for eye banks.”
- Postop refractive correction. Dr. Binder points out that astigmatism isn’t the only problem following corneal transplantation or cataract surgery. “Residual refractive error is also an issue,” he says. “One of the advantages of femtosecond lasers over microkeratomes is that you don’t have to raise the pressure as high inside the eye to create a flap for a post-transplant refractive correction. For that reason, LASIK flaps are often created with the femtosecond laser if correction is needed following penetrating keratoplasty or cataract surgery, with less risk of wound compromise.”
Managing the Cost
When it comes to disadvantages of the laser, a key factor slowing its acceptance as a tool for corneal transplants is the expense of purchasing the laser—and the fact that surgeons cannot currently get additional reimbursement for using it. “The government uses what’s called the golden scalpel rule, which says that if you’re doing an operation, it doesn’t matter how you do it—whether you use a half-million-dollar laser or a $10 scalpel,” says Dr. Culbertson.
Dr. Binder is skeptical that we’ll see a separate reimbursement for laser transplants any time soon. “The government won’t approve a new procedure when they’re having to decrease expenditures,” he says. “Until we can show that visual outcomes are better, I don’t think reimbursement will improve.”
Dr. Culbertson notes that some surgeons are letting the patient cover the extra cost of using the laser, if the patient agrees. “I believe some surgeons treat this as a different operation, a laser keratoplasty,” he explains. “They charge the patient what they feel the procedure is worth and tell the patient in advance that they’re doing a procedure that doesn’t have a code. Other surgeons have taken the position that you get better early results with the laser, so it has a refractive component— the improved refractive outcome in the early postop period. They charge for that refractive component, for which there’s no code or Medicare reimbursement. Other doctors are simply absorbing the cost, but that makes the procedure less desirable because the margin for profit is much lower.”
Dr. Binder is hopeful that using the femtosecond laser for this purpose might eventually be categorized as a premium channel. “With more of these procedures being done, there’ll be more pressure to get reimbursement for some of them,” he notes. “Hopefully the eye bank associations and other major societies can push to allow surgeons to charge a premium for this technology.”
Dr. Binder also believes the cost issues surrounding the laser will likely improve. “Like everything else, the cost of the laser is already coming down,” he points out. “For example, the Ziemer laser is about 33 percent less expensive than some of the others. A second example is that because AMO has two models to sell—the FS 60 and the newer FS 150 (iFS), the FS 60, which has capabilities similar to the FS 150 (iFS), can be sold for about the same as the Ziemer laser. I think as competition heats up over time, we’ll see prices go down. The economy could also force prices down, simply because the recession is undercutting people’s ability to recoup the cost.
“Improving technology will also be a factor,” he adds. “As we develop new lasers and laser engines with new speeds and wavelengths, we may be able to come up with even less expensive technology for performing some of these procedures. For example, in September, Schwind is going to be introducing a new nanosecond laser for making LASIK flaps that uses an entirely different wavelength and speed. Its footprint is one-half to one- third of the current femtosecond laser footprint, and its cost is expected to be less than the current cost of a femtosecond laser.”
Having to Move the Patient
Another factor that may be slowing acceptance of the femtosecond laser for corneal transplantation is the reality that the procedures that most readily justify the expense of purchasing the laser are not performed in the operating room. Since purchasing a separate laser for the OR isn’t feasible, this means patients must receive treatment from the laser in a different location from the location at which the surgery is completed. In the case of penetrating keratoplasty, this is done by using the laser to create an incomplete cut which is later completed in the OR.
Dr. Steinert notes that it’s quite safe to leave a little bridge of tissue posteriorly. “That’s sufficient to allow the patient to have the laser done one day and the surgery done the next day, for example,” he says. “Most patients are given antibiotic drops and then patched, and they do just fine.” Dr. Binder says that his group hasn’t heard of any complications occurring.
Dr. Culbertson notes that there’s a second reason for not completing the cut with the laser. “The other reason for only creating a partial cut is that the eye is under pressure because of the flattening caused by the appla-nation plate,” he says. “I know of a couple of cases in which the laser cut all the way through, and it can be a disaster for the eye. I think you’d have to use a partial cut even if the laser was in the OR.”
Surgeons who prefer to use the laser find ways to manage the inconvenience of having to move the patient. Dr. Culbertson says that in his situation the femtosecond laser is in the same building as the OR; the former is on the third floor, the latter on the sixth floor. “When doing penetrating keratoplasty, we interrupt our surgical schedule to go down and make the cuts in the recipient cornea,” he says. “Then we go upstairs with the patient and finish the procedure.
“In contrast,” he continues, “we can do an anterior lamellar keratoplasty right at the laser; we don’t take the patient upstairs to the OR. We create the donor tissue at the laser right before we incise the patient’s cornea; then we lay the donor tissue in place and put a contact lens over it. For penetrating keratoplasty, we cut the donor corneas here, too, often the day before the procedure so we’ll have the tissue ready.” (Dr. Culbertson acknowledges that the majority of surgeons probably don’t even have a femtosecond laser in the same building as the OR.)
Dr. Steinert notes that it will be interesting to see what happens if cataract-refractive femtosecond lasers become popular. “They need to be in the OR environment too,” he points out. “So, although none of the current versions are set up to do corneal incisions, that could change rapidly. If it did, it might increase the number of people using femtosecond laser technology for transplants as well.”
However, Dr. Binder is skeptical. “Even if the laser eventually has the capability to do all of the steps for cataract surgery—clear cataract clear corneal incisions, intrastromal astigmatic keratotomy, capsulorhexis and lens fragmentation—you’d leave the laser where it is and add those modules onto the laser,” he says. “I think most companies and surgeons would prefer to have the laser close to where they’ll do their cataract surgery, not necessarily in the OR.”
The Laser: Standard of Care?
Despite its advantages, most surgeons seem to feel that it’s far too early to consider the femtosecond laser the standard of care for corneal transplants. “To say that femtosecond laser is the standard of care for corneal transplants would be a severe exaggeration,” says Dr. Steinert.
“Standard of care is a very loaded term medico-legally, so we should be reluctant to use it unless something is overwhelmingly favored by surgeons. Right now, physicians using the femtosecond laser for corneal transplants remain in the minority. As with many new procedures, not everyone is immediately convinced that it offers an advantage. In addition, cost is a significant barrier. There’s no straightforward mechanism for appropriate reimbursement to cover the cost of buying and running the laser and the cost of the time to do the procedure.”
Dr. John agrees. “I don’t believe the laser has improved outcomes enough to be considered the gold standard,” he says. “That could conceivably change in the future, but for now I don’t think it’s earned that label.”
“I wouldn’t say that using the laser has become the gold standard, by any means,” says Dr. Culbertson. “It’s clearly nowhere near that point, both because the long-term outcomes aren’t that much improved, and for practical, finan-cial and time reasons. But I think it’s probably better in terms of the security and strength of the incision, and it seems to be better for early visual rehabilitation after penetrating keratoplasty.”
Dr. Binder is less certain about the laser’s status in this respect. “Standard of care is defined locally,” he notes. “I think that in locations where surgeons can afford a femtosecond laser, they would consider it the standard of care for performing corneal transplantation and creating LASIK flaps. Obviously, that isn’t the case worldwide.”
Dr. Binder acknowledges that long-term astigmatic outcomes with the femtosecond laser for post-keratoplasty astigmatism haven’t yet shown superiority, but notes that that’s not the only consideration. “The femtosecond laser procedures have resulted in faster suture removal, faster recovery of vision, and greater wound strength from a traumatic rupture,” he says. “There have been several reports of patients who had femtosecond transplants who received direct trauma to the eye, which heretofore would have led to blindness because the wounds would pop open. These eyes are resisting that. So although the astigmatism and long-term visual results do not appear to be better with the laser using current approaches, I think the advantages I just mentioned are an improvement. In addition, the speed of the procedure is greatly increased over traditional trephination surgery with this technology.”
At the same time, Dr. Binder believes microkeratomes are here to stay. “Microkeratomes are good instruments,” he says. “They’re less expensive and more easily obtainable—certainly in countries that don’t have a lot of money. They’re not going to go away, and they shouldn’t.”
Whether or not this use of the femtosecond laser is standard of care, why not switch to the laser just to gain the advantages it does offer? “A couple of factors make that less than optimal,” says Dr. John. “The first thing is logistics: The laser part of the procedure has to be done at a different location. Second, it adds out-of-pocket cost for the patient. That would be okay if the laser brought value to the table, like a premium lens that allows you to read up close without glasses. In this case, the value is not equal to the out-of-pocket expense.”
Despite all of the disadvantages, Dr. Culbertson believes it’s worth using the laser to do these procedures. “I believe it’s better,” he says.
Dr. Culbertson is a consultant to AMO, and Dr. Binder is a medical monitor for the company.
“Standard of care is a very loaded term medico-legally, so we should be reluctant to use it unless something is overwhelmingly favored by surgeons. Right now, physicians using the femtosecond laser for corneal transplants remain in the minority. As with many new procedures, not everyone is immediately convinced that it offers an advantage. In addition, cost is a significant barrier. There’s no straightforward mechanism for appropriate reimbursement to cover the cost of buying and running the laser and the cost of the time to do the procedure.”
Dr. John agrees. “I don’t believe the laser has improved outcomes enough to be considered the gold standard,” he says. “That could conceivably change in the future, but for now I don’t think it’s earned that label.”
“I wouldn’t say that using the laser has become the gold standard, by any means,” says Dr. Culbertson. “It’s clearly nowhere near that point, both because the long-term outcomes aren’t that much improved, and for practical, finan-cial and time reasons. But I think it’s probably better in terms of the security and strength of the incision, and it seems to be better for early visual rehabilitation after penetrating keratoplasty.”
Dr. Binder is less certain about the laser’s status in this respect. “Standard of care is defined locally,” he notes. “I think that in locations where surgeons can afford a femtosecond laser, they would consider it the standard of care for performing corneal transplantation and creating LASIK flaps. Obviously, that isn’t the case worldwide.”
Dr. Binder acknowledges that long-term astigmatic outcomes with the femtosecond laser for post-keratoplasty astigmatism haven’t yet shown superiority, but notes that that’s not the only consideration. “The femtosecond laser procedures have resulted in faster suture removal, faster recovery of vision, and greater wound strength from a traumatic rupture,” he says. “There have been several reports of patients who had femtosecond transplants who received direct trauma to the eye, which heretofore would have led to blindness because the wounds would pop open. These eyes are resisting that. So although the astigmatism and long-term visual results do not appear to be better with the laser using current approaches, I think the advantages I just mentioned are an improvement. In addition, the speed of the procedure is greatly increased over traditional trephination surgery with this technology.”
At the same time, Dr. Binder believes microkeratomes are here to stay. “Microkeratomes are good instruments,” he says. “They’re less expensive and more easily obtainable—certainly in countries that don’t have a lot of money. They’re not going to go away, and they shouldn’t.”
Whether or not this use of the femtosecond laser is standard of care, why not switch to the laser just to gain the advantages it does offer? “A couple of factors make that less than optimal,” says Dr. John. “The first thing is logistics: The laser part of the procedure has to be done at a different location. Second, it adds out-of-pocket cost for the patient. That would be okay if the laser brought value to the table, like a premium lens that allows you to read up close without glasses. In this case, the value is not equal to the out-of-pocket expense.”
Despite all of the disadvantages, Dr. Culbertson believes it’s worth using the laser to do these procedures. “I believe it’s better,” he says.
Dr. Culbertson is a consultant to AMO, and Dr. Binder is a medical monitor for the company.



