Optic neuritis is defined as an inflammatory disease of the optic nerve. Though this disease is more common in adults, the pediatric ophthalmologist should also be aware of it, as well as its evaluation and treatment, because associations between optic neuritis and other neuro-inflammatory syndromes may affect final visual and systemic outcomes. Differences in presentation and underlying causes of optic neuritis in children are important to understand in order to avoid misdiagnosis and to guide neuroimaging and laboratory testing. In this article, we’ll cover the various aspects of optic neuritis in pediatric patients that the ophthalmologist needs to know.
Presentation
Optic neuritis is commonly defined as the clinical presentation of decreased vision, impaired color vision or visual field defects
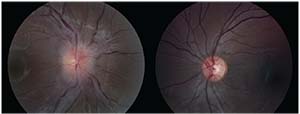 |
| Figure 1. Fundus photographs of a patient with optic neuritis in the right eye demonstrating optic nerve edema. |
with pain on eye movement, often in the presence of a relative afferent pupillary defect unless the disease is bilateral and symmetric. Patients in the pediatric age range may present with different clinical characteristics than those found in adults.1
Obtaining a clear history of the illness can be difficult, if not impossible, in children. As a result, determining exactly when vision loss occurred may not be feasible. Children with optic neuritis may go without detection of the disease until one eye is incidentally covered or closed for some reason, leading the child to complain that he can’t see and prompting a visit to the ophthalmologist or the emergency room. Bilateral involvement is more common in children than in adults, and often a child will present to the emergency room only if bilateral simultaneous disease occurs, or after the second eye becomes involved. A meta-analysis of isolated pediatric optic neuritis studies found that 72 percent of children under the age of 10 presented with bilateral involvement, while in children older than 10 years, 70 percent presented with unilateral optic neuritis.2
Pain or pain with eye movement isn’t a consistent feature of pediatric optic neuritis; therefore the absence of pain doesn’t rule out optic neuritis.3 Severe vision loss to worse than 20/200 is common in children with optic neuritis (90 to 95 percent), in contrast to adults in the optic neuritis treatment trial, of whom 64 percent had visual acuities better than 20/200.4,5 However, final visual outcomes are usually very good, with visual acuities better than 20/40 in most cases.4,6,7 Children with optic neuritis will present more frequently with an anterior optic neuritis, rather than the retrobulbar optic neuritis more common in adults, with the majority of cases presenting with optic nerve edema (Figure 1).8,9 Optic nerve pallor commonly develops following resolution of the optic neuritis. Visual field defects in patients with optic neuritis are variable, and some patients are too young to perform formal visual field testing with any reliability. Optical coherence tomography of the retinal nerve fiber layer may initially demonstrate thickening followed by thinning as optic nerve pallor develops.10,11 One study found that ganglion cell layer thickness can be affected in any pediatric demyelinating disease, with thinning occurring with or without the presence of optic neuritis.12
Epidemiology
In contrast to adult optic neuritis, optic neuritis in children is a relatively rare event. Incidence estimates for adults were 5.1/100,000 in one population-based study; incidence in the pediatric population is 0.5/100,000.13,14 As a result of the incidence of pediatric optic neuritis being approximately 10 percent of the adult rate, studying pediatric optic neuritis in a systematic manner is more difficult. However, research has found that in children assumed to be pre-pubertal, the female:male ratio for involvement of optic neuritis is close to 1:1 according to one study, while post-pubertal children mimic the adult population with a female:male preponderance of 2:1.15
Evaluation & Underlying Causes
As opposed to adults, in whom optic neuritis is most often of the idiopathic demyelinating type, an underlying cause can be found more frequently in the pediatric population.1 Often a history of a flu-like illness preceding the onset of vision loss by a week or so can be elicited from the parents, and these cases can be attributed to a post-infectious optic neuritis.1 Optic neuritis can also follow vaccination. Other causes for optic
 |
| Figure 2. T1-weighted fat-saturated MRI of the orbits, post-gadolinium, of the patient in Figure 1, demonstrating longitudinally extensive right optic neuritis. |
neuritis in children can include, but are not limited to, sarcoidosis, syphilis, tuberculosis, varicella zoster, Epstein-Barr virus and treatment with etanercept or infliximab. Differentiating between optic neuritis and neuroretinitis or Leber hereditary optic neuropathy may be difficult at initial presentation, but neuroimaging and the appropriate laboratory workup in addition to clinical history (such as bilateral sequential painless vision loss with negative neuroimaging in Leber hereditary optic neuropathy) can help to make the appropriate diagnosis in these patients.
Neuroimaging in pediatric optic neuritis is essential. Given the absence of typical symptoms associated with adult optic neuritis and the frequently bilateral nature of pediatric optic neuritis, neuroimaging is key in ruling out the possibility of an underlying intracranial lesion that could cause bilateral optic disc edema, and confirming the presence of optic nerve enhancement (Figure 2).
Children should undergo an MRI of the brain and orbits with and without contrast to evaluate for other white matter lesions as well, such as in acute disseminated encephalomyelitis (ADEM) and multiple sclerosis. Some children will also require neuroimaging of the spinal cord if you suspect neuromyelitis optica, or if the patient has signs of spinal cord dysfunction. Working with a pediatric neurologist is extremely helpful in these situations.
A lumbar puncture may be indicated to look for oligoclonal bands that are present in multiple sclerosis if the patient has white matter lesions on brain MRI.
Other Disorders
Acute disseminated encephalomyelitis is usually a monophasic illness with multifocal involvement of the central nervous system and encephalopathy, which may include optic neuritis.16
Informed parents will ask the physician, “What is our child’s risk for developing multiple sclerosis?” Overall, the risk for developing multiple sclerosis appears to be lower for the pediatric population following isolated optic neuritis in comparison to adults. However, similar to the adult population, the presence of white matter lesions on initial brain MRI is associated with a 27-fold increased risk of developing multiple sclerosis.2 In addition, as the age at presentation of pediatric optic neuritis increases, the risk of developing multiple sclerosis increases by 32 percent per year.2 Currently, a wide range of results have been published regarding the rates of conversion to multiple sclerosis from isolated pediatric optic neuritis.17
Neuromyelitis optica (NMO) and neuromyelitis optica spectrum disorder (NMO-SD) are more devastating immune-mediated neuroinflammatory disorders that may present initially with optic neuritis. Making the diagnosis is important as immunomodulatory agents can prevent disease flares and loss of function. In NMO, the discovery of the aquaporin-4 antibody has revolutionized making the diagnosis. The International Panel for NMO Diagnosis published criteria for making the diagnosis of NMO-SD, with stratification based on the presence or absence of aquaporin-4 antibodies,18 which are are highly specific for NMO-SD. The panel’s criteria have since been deemed appropriate for use in the pediatric population.19 Treatment of NMO-SD should be performed with a neuroimmunologist where available.
A more recent discovery that’s been shown to be involved in neuroinflammatory disorders is anti-myelin oligodendrocyte glycoprotein (MOG) antibody, though testing for this antibody is not yet commercially available in the United States. Anti-MOG antibody positivity appears to be associated with ADEM in younger patients, and with optic neuritis in older patients.20 A positive anti-MOG antibody appears to exclude the possibility of being aquaporin-4 antibody positive.21 The clinical implications of anti-MOG positivity are still being studied, but it appears associated with an NMO-SD-like disease that’s different from aquaporin-4 antibody-mediated NMO-SD.
Treatment Regimen
The treatment regimen often prescribed for adults with typical isolated demyelinating optic neuritis is dictated by the Optic Neuritis Treatment Trial. No such trial has yet been performed for children with optic neuritis. As a result, there’s no standard regimen for treatment of pediatric optic neuritis, and the choice of treatment is dependent upon the clinician.
Using data on adults from the ONTT and applying it to children, the initial treatment of choice for pediatric optic neuritis is intravenous methylprednisolone for three to five days (20 to 30 mg/kg/d, 1 g maximum).17 Some physicians follow this with an oral prednisone taper similar to that in the ONTT. In cases of refractory vision loss or more extensive CNS involvement, intravenous immunoglobulin or plasma exchange are used as well. Lack of improvement despite treatment should raise your level of suspicion for neuromyelitis optica or NMO-SD.
Treatment of neuromyelitis optica and multiple sclerosis is beyond the scope of this article, and should be managed by a pediatric neurologist or neuroimmunologist, with vision monitoring performed by the ophthalmologist.
Future Directions
Many questions remain concerning pediatric optic neuritis, and future evaluations are likely to depend more upon molecular biomarkers to classify disease. Also, a standardized consensus regarding the treatment of pediatric optic neuritis remains to be developed. The Pediatric Eye Disease Investigator Group currently has a pediatric optic neuritis registry that’s enrolling patients under the age of 16 with optic neuritis with an onset of symptoms within two weeks.22 This registry will systematically evaluate patient outcomes and, hopefully, lead to a prospective treatment trial for pediatric optic neuritis patients. Elucidating the role of anti-MOG antibodies in pediatric demyelinating diseases may help to define a distinct disease entity, similar to what has occurred for aquaporin-4 antibody-positive NMO-SD. REVIEW
Dr. Peragallo is an assistant professor in the departments of ophthalmology and pediatrics at Emory University School of Medicine in Atlanta. He has no financial interest in any products mentioned in the article.
1. Brodksy, MC. The swollen optic disc in children. In Pediatric Neuro-Ophthalmology, 3rd Edition. New York, NY, Springer, 2016:121-198.
2. Waldman AT, Stull LB, Galetta SL, Balcer LJ, Liu GT. Pediatric optic neuritis and risk of multiple sclerosis: Meta-analysis of observational studies. J AAPOS 2011;15:441-6.
3. Yeh EA, Graves JS, Benson LA, Wassmer E, Waldman A. Pediatric optic neuritis. Neurology 2016;87:S53-8.
4. El-Dairi MA, Ghasia F, Bhatti MT. Pedatric optic neuritis. Int Ophthalmol Clin 2012;52:29-49.
5. Beck RW, Cleary PA, Anderson MM Jr, Keltner JL, Shults WT, Kaufman DI, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med 1992;326:581-8.
6. Liu GT, Volpe NJ, Galetta SL. Visual loss: Optic neuropathies. In Neuro-ophthalmology: Diagnosis and Management, 2nd ed. Saunders Elsevier, Philadelphia, 2011;103-198.
7. Wan MJ, Adebona O, Benson LA, Gorman MP, Heidary G. Visual outcomes in pediatric optic neuritis. Am J Ophthalmol 2014;158:503-7.
8. Wiljeto M, Shroff M, Buncic JR, Kennedy J, Goia C, Banwell B. The clinical features, MRI findings, and outcome of optic neuritis in children. Neurology 2006;67:258-62.
9. Morales DS, Siatkowski RM, Howard CW, Warman R. Optic neuritis in children. J Pediatr Ophthalmol Strabismus 2000;37:254-9.
10. Yeh EA, Weinstock-Guttman B, Lincoff N, Reynolds J, Weinstock A, Madurai N, et al. Retinal nerve fiber layer thickness in inflammatory demyelinating diseases of childhood onset. Mult Scler 2009;15:802-10.
11. Kupersmith MJ, Mandel G, Anderson S, Meltzer DE, Kardon R. Baseline, one and three month changes in the peripapillary retinal nerve fiber layer in acute optic neuritis: Relation to baseline vision and MRI. J Neurol Sci 2011;308:117-23.
12. Yeh EA, Marrie RA, Reginald YA, Buncic JR, Noguera AE, O’Mahony J, et al. Functional-structural correlations in the afferent visual pathway in pediatric demyelination. Neurology 2014; 83:2147-52.
13. Rodriguez M, Siva A, Cross SA, O’Brien PC, Kurland LT. Optic neuritis: A population-based study in Olmstead County, Minnesota. Neurology 1995;45:244-50.
14. Langer-Gould A, Zhang JL, Chung J, Yeung Y, Waubant E, Yao J. Incidence of acquired central nervous system demyelinating syndromes in a multiethnic cohort of children. Neurology 2011;77:1143-1148.
15. Boomer JA, Siatkowski RM. Optic neuritis in adults and children. Semin Ophthalmol 2003;18:174-80.
16. Pohl D, Alper G, Van Haren K, Kornberg AJ, Lucchinetti CF, Tenembaum S, Belman AL. Acute disseminated encephalomyelitis: Updates on an inflammatory CNS syndrome. Neurology 2016;S38-45.
17. Borchert M, Liu GT, Pineles S, Waldman AT. Pediatric optic neuritis: What is new. J Neuroophthalmol 2017;37 Suppl 1:S14-S22.
18. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015; 85:177-89.
19. Chitnis T, Ness J, Krupp L, Waubant E, Hunt T, Olsen CS, et al. Clinical features of neuromyelitis optica in children: United States Network of Pediatric MS Centers report. Neurology 2016;86:245-52.
20. Fernandez-Carbonell C, Vargas-Lowy D, Musallam A, Healy B, McLaughlin K, Wucherpfennig KW, Chitnis T. Clinical and MRI phenotype of children with MOG antibodies. Mult Scler 2016;22:174-84.
21. Hacochen Y, Mankad K, Chong WK, Barkhof F, Vincent A, Lim M, et al. Diagnostic algorithm for relapsing acquired demyelinating syndromes in children. Neurology 2017;89:269-78.
22. Pineles SL, Liu GT, Waldman AT, Lazar E, Kupersmith MJ, Repka MX; Pediatric Eye Disease Investigator Group and the Neuro-Ophthalmology Research Disease Investigator Consortium. Pediatric Optic Neuritis Prospective Outcomes Study. J Neuroophthalmol 2016;36:115-7.



