Goniosynechialysis has significant potential for increased utilization, for two reasons: First, more surgeons are becoming comfortable performing gonioscopy in the office and the OR, thanks to the growing popularity of minimally invasive glaucoma surgeries, or MIGS. Second, the Effectiveness of Early Lens Extraction for the Treatment of Primary ACG study (EAGLE), published in The Lancet in October 2016,1 indicated that clear lens extraction is both more efficacious and more cost-effective than doing laser iridotomy in patients presenting with primary angle closure.
Given these two developments, if you’re going in to remove the lens in a patient in whom there’s a preoperative concern of angle closure, I believe it’s a good idea to perform intraoperative gonioscopy after the IOL has been placed. That will allow you to deter-mine whether there are lingering synechiae in the angle, or significant areas of synechial closure that could be opened relatively easily. If you do find synechiae in the angle, cataract surgery provides a perfect opportunity to perform goniosynechialysis to open the angle, improve trabecular outflow and potentially lower the patient’s pressure.
Performing the Procedure
The classic description of gonio-synechialysis in patients with acute or subacute angle-closure glaucoma appeared in 1984.2 Viscoelastic was used to deepen the anterior chamber; then the angle was directly visualized by gonioscopy. An irrigating cyclodialysis spatula was used to separate the synechiae from the peripheral cornea via anterior to posterior movement of the iris.
Interestingly, these surgeons noted a high rate of success (80 percent) in patients who had had angle closure for less than one year, because synechiae that have been in place longer than a year are not easily separated. (There’s also the issue of whether the trabecular outflow behind the synechiae is still functional when the angle has been closed for a significant time.) However, I would point out that we usually don’t know how long synechiae have been present—unless there was a clear attack of angle closure or a surgical intervention—so this procedure is usually worth a try.
In terms of instrumentation, there are a variety of techniques, but many surgeons use microsurgical forceps rather than a cyclodialysis spatula. When the procedure was first per-formed, it was done with an irrigating spatula because they didn’t have good-quality viscoelastics. Fluid irrigation into the eye kept it formed; then one could use the instrument to manipulate the tissue. This works—I’ve performed it in the past with a spatula—but I find it easier to perform with microforceps that allow me to grasp the tissue.
The postoperative protocol is straightforward. Treat any inflammation with steroids and NSAIDs. Pressure control is essential, especially in the early postoperative period, because a pressure spike can result from a release of pigment, blood or retained viscoelastic. I routinely inject a miotic intraoperatively after the procedure to try to keep the angle open; some surgeons advocate longer-term use of miotics as well.
Possible complications of gonio-synechialysis include:
• Mild to moderate postoperative inflammation. This is probably the most common event.
• Hemorrhage. Hemorrhages are relatively uncommon and usually self-limiting; they can be minimized by exercising care during the procedure. If a hemorrhage does occur, it’s most likely a tear in a very focal area, so the first thing to do is to stop pulling in that location. I inject a little more viscoelastic to decrease the hemorrhage by increasing the pres-sure in that location. I’ve never had a serious hemorrhage—one that recurred or lasted for a long period of time—during this procedure.
• Iridodialysis or cyclodialysis. If you perform direct or indirect visualization of the angle during the procedure, you’re much less likely to cause a dialysis of either the iris or the ciliary body.
• Corneal endothelial damage. In my experience, corneal endotheli-al damage is uncommon as long as one is careful to use viscoelastic and exercise caution near the cornea.
• Problems resulting from re-tained viscoelastic. This can be avoided by carefully removing visco-elastic at the end of the procedure.
GSL or Trabeculectomy?
In a primary angle-closure glaucoma patient, performing cataract extraction with goniosynechialysis instead of trabeculectomy often pro-vides an acceptable outcome without associated risks. In my experience, it makes sense to simply remove the lens, perform goniosynechialysis and then reassess the pressure. You may be pleasantly surprised with the long-term results. (You can always go back later and do a trabeculectomy.)
Consider a patient of mine who presented at the age of 49 with a one-year history of primary angle-closure glaucoma. She had a T-max in the low 40s in both eyes and she’d undergone iridotomies in both eyes. When I first saw her, she had excellent visual acuity and was on brimonidine and travoprost, with pressures of 16 and 18 mmHg. Gonioscopy at that time revealed angle closure of grade B(C) 20-s (the “s” referring to a steep ap-proach). Cupping was 0.6 and 0.8 with some pallor of both optic nerves. She had an inferior arcuate defect in both eyes, as well as a nasal step in her left eye. The angle had 1 to 2+ pigment, but I noted no PAS at that time.
I followed her for the next several years; her pressures, optic nerves and visual fields remained stable. Nevertheless, I continued to perform annual gonioscopy, which is very im-portant in these patients, and her angles gradually became narrower with appositional closure. For that reason, I performed an argon laser iridoplasty, which opened up her angles again.
After that, her pressure and visual fields remained stable for a while, but two years later at the age of 54, her pressures were 17 and 26 mmHg and she was starting to develop peripheral anterior synechiae. (During those five years her lens likely increased its anterior-posterior diameter, pushing the iris forward and shallowing the anterior chamber. This is a significant component in progressive angle closure.) Even though she didn’t have a visually significant cataract, it was “glaucoma significant” and I per-formed cataract extraction along with goniosynechialysis in both eyes.
She is now seven years postop. She remains 20/20 and is off of all glaucoma medications; she has open angles, IOPs in the low teens, and stable visual fields and optic nerves. All of this was accomplished without resorting to trabeculectomy, which meant a shorter recovery time and lower risk of complications.
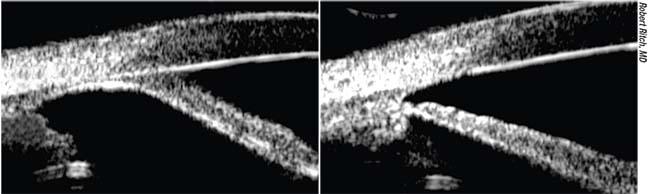 |
| An example of a narrow angle before (left) and after goniosynechialysis was performed. |
Since Campbell and Vela’s initial description, a review was published of 81 patients with primary ACG with uncontrolled IOP and more than six clock hours of synechiae that underwent phaco/GSL. Eighty-nine percent had reduction of PAS and controlled IOP without medications,3 consistent with the case described above. More recent literature also supports this alternative to trabeculectomy. One study found that patients had shorter recovery times and fewer complications with GSL compared to trabeculectomy;4 another found similar postoperative IOP and medication use, but decreased complications with GSL;5 and another found no difference in postop IOP, but improved visual acuity and a deeper anterior chamber with PAS resolution.6
A fourth study7 found that when the glaucoma in angle-closure patients was already well-controlled, there was no benefit to performing goniosynechialysis while undergoing cataract extraction. However, if you can minimize your patient’s use of medications long-term without the risks associated with trabeculectomy, that’s a winning combination. For that reason, I think it’s appropriate to consider GSL in primary angle-closure glaucoma patients who have well-controlled pressure, if they’re dependent on several medications.
Strategies for Success
These suggestions will help ensure the best possible outcome when performing GSL in conjunction with cataract surgery:
• Choose appropriate candidates. Considerations include:
— Goniosynechialysis is ideal when a patient has 90 to 180 degrees of synechiae.
— Any level of angle closure is acceptable, in my opinion, including acute, subacute and “chronic” angle closure, as well as angle closure in the presence of plateau iris.
— GSL can be performed in combination with endocycloplasty.
— GSL can be used to address residual angle closure after iridotomy or argon laser iridoplasty.
Contraindications, in my view, include patients with neovasculari-zation in the angle or the iris, as well as patients with chronic or recurrent uveitis, or ICE syndrome.
• Perform gonioscopy on your angle-closure patients regularly. Angle closure may progress, and synechiae may develop over time.
• Aim for IOP control during the procedure to minimize corneal edema and optimize visualization. Having a clear cornea for visualization is crucial. If your patient has markedly elevated pressure prior to the surgery, that requires treatment, including the use of IV mannitol preoperatively.
• If possible, perform goniosynechialysis under direct visualization. It’s important to be able to see what you’re doing during the procedure, in order to avoid tearing tissue, potentially causing significant bleeding or something worse than the synechiae. (A small amount of bleeding, however, isn’t unusual or harmful.) Of course, being sensitive to the feel of what you’re doing is equally important. If you have to pull forcefully and the tissue is still not releasing, it’s probably wise to leave that area alone to avoid causing a tear.
The concept behind goniosyn-echialysis is simple and straight-forward, but as with many surgical procedures, you don’t want to cause a bigger problem than the initial problem you’re attempting to treat.
• Avoid working with the pupil dilated. Constricting the pupil with Miochol or Miostat after cataract surgery is helpful; you have the pupil slightly more on stretch. If the pupil is widely dilated, it’s much more difficult to see if you’ve broken the synechiae.
• Using viscoelastic is crucial. Viscoelastic helps keep the chamber formed throughout the procedure. It also helps with hemostasis and the initial viscodissection. Injecting viscoelastic directly into the angle can help to “hyper-deepen” the peripheral chamber, making it easier to identify the synechiae.
Whether you can open up some of the synechiae just by using the viscoelastic to stretch the angle is questionable, but viscoelastic will definitely allow you to differentiate appositional from synechial closure.
• If necessary, make a second incision to reach all of the synechiae. A two-site entry may be necessary, depending on where the synechiae are located. If some are subincisional or on the temporal side of the eye, then you’ll need to make an incision on the opposite side to open those up.
• Remember that you don’t have to separate every synechia to improve outflow. If you only open up a significant portion of the angle and leave some synechiae untouched, that doesn’t mean the procedure has been a failure. Freeing up all 12 clock hours doesn’t have to be your ultimate goal; if you open six clock hours, you may totally change the outflow and improve IOP control.
• When performing a MIGS procedure, consider doing gonio-synechialysis first. Combining goniosynechialysis and a MIGS procedure could increase flow into the anterior chamber angle and then distal to the potentially less-functional trabecular meshwork. Other angle procedures may also be performed at these locations in the future.
• If you can’t ensure good visualization through the cornea, endoscopy can be used. Gonio-synechialysis can be performed with an endoscope using a 19- or 23-ga. probe if you don’t have good visualization through the cornea, but this is a more challenging technique.
• Be sure to carefully remove the viscoelastic after the procedure. As with any intraocular surgery, viscoelastic left behind can cause pressure spikes.
An Option Worth Considering
Performing goniosynechialysis in combination with phaco may be an effective and safe treatment option for many patients with primary angle-closure glaucoma. The technique isn’t highly complex, especially if you’re performing MIGS procedures, many of which require you to be comfortable visualizing and working in the anterior chamber angle.
By opening the angle, helping to re-establish trabecular meshwork flow and improving pressure control, goniosynechialysis may decrease the need for medication use, as well as saving the patient from undergoing more invasive and higher-risk procedures. REVIEW
Carla J. Siegfried, MD, is the Jacquelyn E. and Allan E. Kolker MD Distinguished Professor of Ophthalmology at Washington University School of Medicine in St. Louis. She has no financial ties to any product mentioned.
1. Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, Scotland G, Javanbakht M, Cochrane C, Norrie J; EAGLE study group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): A randomised controlled trial. Lancet 2016;388:10052:1389-1397.
2. Campbell DG, Vela A. Modern goniosynechialysis for the treatment of synechial angle-closure glaucoma. Ophthalmology 1984;91:9:1052-60.
3. Teekhasaenee C, Ritch R. Combined phaco-goniosynechialysis for uncontrolled chronic angle-closure glaucoma after acute angle-closure glaucoma. Ophthalmology 1999;106:669-75.
4. Lai JS, Tham CC, Lam DS. The efficacy and safety of combined phacoemulsification, intraocular lens implantation, and limited goniosynechialysis, followed by diode laser peripheral iridoplasty, in the treatment of cataract and chronic angle-closure glaucoma. J Glaucoma 2001;10:4:309-15.
5. Zhao X, Yang X, et al. Comparison of combined phacoemulsification, intraocular lens implantation, and goniosynechialysis with phacotrabeculectomy in the treatment of primary angle-closure glaucoma and cataract. The Asia-Pacific Journal of Ophthalmology 2013;2:5:286–290.
6. Zhang H, Tang G, Liu J. Effects of phacoemulsification combined with goniosynechialysis on primary angle-closure glaucoma. J Glaucoma 2016;25:5:e499-503.
7. Lee CK, Rho SS, Sung GJ, et al. Effect of goniosynechialysis during phacoemulsification on IOP in patients with medically well-controlled chronic angle-closure glaucoma. J Glaucoma 2015;24:6:405-9.




