 |
PREOPERATIVE CONSIDERATIONS
As with any surgery, patient selection and timing is key. It’s important to be mindful that we’re treating the patient, not just the eye. Factors to consider beyond intraocular pressure and optic nerve status include patient age, general health, life expectancy, lifestyle and family history. A filtering procedure that’s successful from the surgeon’s perspective may, in fact, diminish a patient’s quality of life due to long-term bleb-related complications. Therefore, it’s important to consider other IOP-lowering procedures before making the decision to proceed with filtering surgery.
Trabeculectomy requires frequent postoperative visits and the patient must be able and willing to keep these appointments. It’s also important to assess the risk of bleb infection in the context of the patient’s lifestyle. For example, a person who often travels to remote areas without access to medical care, or one who engages in water-based sports as a hobby or for a living, isn’t a good candidate for filtering surgery.
Carefully assess the ocular history, paying special attention to factors that may increase the risk for scarring, such as multiple prior surgeries and uncontrolled uveitis. You should also evaluate the factors that could increase the risk of complications. For example, patients with high myopia and pigment dispersion are at higher risk for hypotony maculopathy, whereas patients with angle closure disease and high hyperopia are at risk for malignant glaucoma after filtering surgery. Contact lens wearers may not be able to continue wearing lenses after filtering surgery and you should discuss this possibility with them beforehand. Finally, a history of a bad outcome after filtration surgery in the fellow eye should be taken seriously.
A careful preoperative slit lamp examination is a must. Specifically, assess the superior conjunctiva for mobility—this can be easily done by having the patient look down and then moving the eyelid over the superior conjunctiva. It’s also helpful to locate vascular landmarks in the superior conjunctiva that you can use later to identify the scleral flap site intraoperatively.
INTRAOPERATIVE CONSIDERATIONS
We typically perform modified trabeculectomy with an Ex-PRESS shunt (the P50 model) because the visual recovery is quicker compared to standard trabeculectomy.1 This is important for these patients because they don’t have visual symptoms before surgery, but the surgery ends up inducing some temporary visual distortion. So, the quicker they can recover their vision, the more acceptable the surgery is to them. Also, using the shunt obviates the need for a sclerectomy and an iridectomy.
Important aspects of surgery include:
• Adequate exposure. We use a Lieberman eyelid speculum and a superior corneal traction suture to provide adequate exposure of the superior quadrant. While passing the traction suture, take care to avoid corneal perforation, which will result in aqueous leak and low IOP, a situation that’s not ideal for scleral flap dissection. If inadvertent corneal perforation does occur, place viscoelastic in the AC, which will allow the case to proceed in the usual fashion.
• Conjunctival flap and closure. The conjunctival flap can be limbus- or fornix-based, with the latter being our preferred approach. Maintaining conjunctival integrity is critical for the success of filtration surgery, and therefore this tissue should be handled with great care, especially in eyes with thin or scarred conjunctiva in which buttonholes can easily form. Conjunctival manipulation should be gentle and minimal; when possible, grasp subconjunctival Tenon’s tissue rather than the conjunctival edge. A watertight conjunctival closure is critical for the formation of an elevated bleb, and you can ensure this by inflating the anterior chamber with balanced salt solution and confirming that there is no aqueous leak at the end of surgery.
• Scleral flap and closure. We use a 3x3-mm square, partial thickness scleral flap, typically closed with two 10-0 nylon sutures. During scleral flap dissection, care should be taken to maintain adequate flap thickness in order to cover the Ex-PRESS shunt, as well as an adequate scleral bed on which the device can rest.
• Mitomycin-C application. There are many ways to apply mitomycin-C during filtering surgery, but the main goal is a diffuse distribution as posteriorly as possible in order to minimize the formation of localized, cystic and avascular blebs. We perform a conjunctival snip incision at the limbus as the first step after placement of the corneal stay suture. We then use a cannula to instill 0.1 ml of 0.2 mg/ml mitomycin-C in the subconjunctival space and then use a Weck-Cel sponge to distribute the mitomycin-C diffusely. We create the conjunctival flap at the end of this step, and use BSS to irrigate the subconjunctival space.
POSTOPERATIVE CONSIDERATIONS
We often tell patients that half the work in filtering surgery is in the operating room performing the procedure and the other half is in the clinic with postoperative care. The goals during the postoperative follow-up period are monitoring for complications and identifying factors that may jeopardize long-term bleb function and then intervening appropriately. For example, if the IOP is high two weeks after surgery due to tight flap sutures, then the appropriate intervention is not to restart IOP-lowering medications but to lyse (or remove) one or more flap sutures so that a bleb can form (or enlarge).
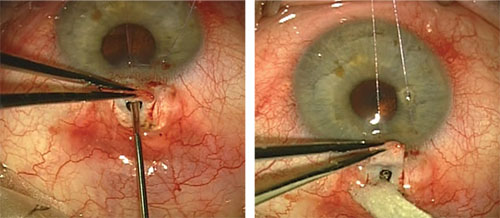 |
| Insertion of the Ex-PRESS shunt under a partial thickness scleral flap. |
Although postoperative care for filtering surgery is more intense than for other surgeries, most early complications are transient, and serious complications such as choroidal hemorrhage are fortunately rare. Following are some common postop situations and our response to them:
• Low IOP. If the IOP is too low after surgery, the first step is to identify the cause of the hypotony. The most common causes are overfiltration and wound leak. A careful slit lamp examination after instillation of fluorescein drops can identify most wound leaks; however, sometimes a fluorescein strip may be required to pinpoint the exact site of aqueous leak. Hypotony after filtering surgery is usually transient and most cases can be managed conservatively. The decision to intervene depends on several factors, such as the presence and extent of wound leak, bleb height, AC depth, presence and extent of choroidals, and the status of the macula. For example, a patient with a small wound leak in the presence of an elevated bleb and peripheral iridocorneal touch can be managed conservatively, whereas a patient with hypotony and a flat AC usually requires urgent intervention in order to prevent endothelial damage.
• High IOP. If the IOP is too high after filtering surgery, the first step, again, is to identify the cause. The most common causes are tight scleral flap sutures and retained viscoelastic. Other possibilities include ciliary block, suprachoroidal hemorrhage, early bleb encapsulation, and sclerostomy or Ex-PRESS lumen plugged by blood, iris or vitreous. The decision to intervene depends on factors such as the level of IOP elevation, the optic nerve status and the risk of hypotony. Tight flap sutures are effectively addressed by laser suturelysis, but this is best avoided in the first few days after surgery, if possible. Digital massage to separate the scleral flap edges allows aqueous outflow and usually lowers IOP until sutures can be lysed.
• IOP is acceptable. If the IOP is on target, a watchful eye must still be maintained on the bleb and surrounding conjunctiva to detect signs of early bleb scarring. Interventions in this situation have a better chance of succeeding when performed as early as possible, while the bleb is scarring, as opposed to when it has completely scarred. In many cases, the bleb can be revived with the use of interventions such as aggressive topical steroids, 5-fluorouracil injections, timely suturelysis, digital massage and bleb needling.
While the recent development of blebless surgeries is welcome and exciting, in some of our patients there’s just no substitute for filtering surgery. Therefore, it’s important for a glaucoma surgeon to be able to perform this procedure well and expertly manage the postoperative course and potential complications in order to minimize risk and maximize outcomes. REVIEW
Dr. Radhakrishnan is an associate at the Glaucoma Center of San Francisco and research director of the Glaucoma Research and Education Group in San Francisco. She has no financial interest in the products discussed. Dr. Iwach is the executive director of the Glaucoma Center of San Francisco, an associate clinical professor of ophthalmology at the University of California, San Francisco and a faculty instructor at the California Pacific Medical Center Department of Ophthalmology. He is a consultant to Bausch + Lomb, Alcon, Allergan and AcuMEMS.
1. Beltran-Agullo L, Trope GE, Jin Y, Wagschal LD, Jinapriya D, Buys YM. Comparison of visual recovery following ex-PRESS versus trabeculectomy: results of a prospective randomized controlled trial. J Glaucoma 2015;24:3:181-6.



