While aggressively treating patients for dry eye after corneal refractive surgery is considered standard of care, doing the same for post cataract surgery patients is far less common. Yet these are the types of patients, due to their age and their higher incidence of confounding systemic disease, that are more prone to dry eye than their younger, healthier refractive surgery counterparts.
Cutting the Corneal Nerves
It is widely accepted that the act of cutting via a microkeratome, or ablating via a laser, the corneal nerves during refractive surgery leads to an iatrogenic dry eye syndrome in nearly all patients. It is now the standard of care to treat all corneal refractive surgery patients for dry eye syndrome for at least a few months after surgery until the corneal nerves have had a chance to regenerate.
During clear corneal cataract surgery, which now accounts for 73 percent of cataract surgery according to this year's trends survey by the American Society of Cataract and Refractive Surgery, a large portion of the corneal nerves are cut. With a typical cataract surgery, the primary incision may be about 3.0 mm in width, and the paracentesis about 1.0 mm in width, giving a total arc length of 4.0 mm of full-thickness corneal incisions. If we add to this the additional incisions for astigmatic correction, such as limbal relaxing incisions, or the three-incision technique of bimanual cataract surgery advocated by some surgeons, the cutting of corneal nerves is even more severe.
The corneal nerves are important in the self-regulation of tears since they provide the sensation in the feedback loop that signals tear production. When we block or decrease the function of these nerves, we can significantly limit the eye's ability to create a proper tear film, which can lead to decreased vision and symptomatic patients.
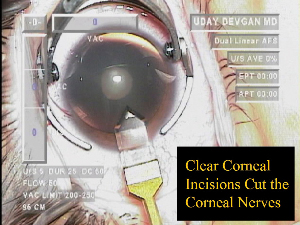
During clear corneal cataract surgery, a large portion of the corneal nerves are cut.
Visual Function
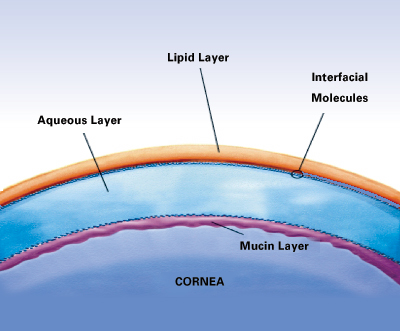
The first refractive surface of the eye is the tear film, and in order to maximize visual acuity and performance for our patients, we must ensure that this tear film is healthy and not dysfunctional. Robert Latkany, MD, director of the dry eye clinic at the New York Eye & Ear Infirmary, has suggested using the tear normalization test for the diagnosis of dry eye. This test involves checking the visual acuity of the patient, then instilling artificial tears and immediately re-checking the visual acuity. An immediate increase in the patient's visual acuity may signify a pre-existing insufficient tear film and therefore, suboptimal visual performance when dry.
Our modern day cataract surgery patients are very much refractive surgery patients: they expect great unaided vision immediately after surgery. Even if our IOL calculations are spot-on, and we eliminate the patients' pre-existing astigmatism, a dysfunctional tear film will significantly limit the post-op visual acuity and satisfaction level of the patient.
Dry-Eye Symptoms
As a resident, I was taught that patients who complained of a foreign body sensation or ocular irritation after clear corneal cataract surgery were just feeling their incisions, and that with time it would resolve. It always struck me as odd that a huge traumatic corneal abrasion would heal in a couple of days and the patient would be asymptomatic, but yet our controlled incisions, often made with diamonds, would cause the patients months of discomfort.
I now understand that the patients' symptoms of foreign body sensation and ocular irritation after cataract surgery are often due to dry-eye syndrome, induced or worsened by the act of cutting the corneal nerves. These patients will need a few months in order to regenerate these corneal nerves and have their symptoms subside.
Confounding Factors
The act of cataract surgery induces ocular inflammation, which may adversely affect patients' tear-film production and stability. In addition, we prescribe our postop cataract patients strong medications, which can cause further ocular irritation and tear-film disruption.
The fluoroquinolones have been a welcome addition to ophthalmology, but they can cause significant irritation with the ocular surface. Ciprofloxacin has been reported to cause deposits of medication within the cornea at certain dosing intervals, and all fluoroquinolones have the ability to cause a "medicamentosa" picture, where the drug and/or its solvent cause iatrogenic tear film disruption, punctate corneal epitheliopathy, and ocular surface irritation and inflammation.
Treatment Options
The treatment options for post-cataract surgery dry-eye syndrome can be divided into a few primary categories:
1. Topical traditional artificial tears
2. Topical fortified artificial tears
• Soothe (emollient lubricant that restores the tear's lipid layer)
• Systane (HP-guar gellable lubricant)
3. Topical lubricating gels and ointments
4. Topical anti-inflammatory medications
• Steroids
• Restasis
5. Mechanical blockage of tear drainage
• Punctual plugs
6. Systemic Treatments
• Oils: Flaxseed oil, omega 3 essential fatty acids
• Doxycycline, other treatments for blepharitis
When looking for a primary treatment suitable for nearly all patients after routine cataract surgery, the options that are most applicable tend to be the topical artificial tears. The lubricating gels and ointments tend to blur the patients' vision, and placement of punctual plugs or use of systemic treatments seems excessive for a first line treatment choice. Since the cataract patients are already typically taking a topical steroid during the post-op period, adding Restasis to their regimen would not likely be helpful according to its package insert. This leaves us with topical artificial tears.
The traditional artificial tears can restore the patients tear film temporarily, but their effect is often short lived due to the evaporation that occurs rapidly. These tears often require aggressive dosing schedules and can induce a toxic epitheliopathy if they contain preservatives. And with the higher dosing schedules, patient compliance and satisfaction both drop.
The newer fortified artificial tears work differently. Systane (Alcon) is a lubricant that contains demulcents and HP-guar, which binds to the hydrophobic tear surface and creates a gel. This can help to prevent pre-mature tear break-up and can give a relief that may last longer than traditional artificial tears.
Soothe (Alimera) is an emollient lubricant that contains a lipid restorative which restores the lipid layer of the tear film and provides a barrier to tear evaporation. In addition, the emollient nature of the drops promotes a soothing effect to the ocular surface. I tell patients to think of traditional artificial tears as the equivalent of licking your chapped lips – it helps for a few minutes, after which time, the water evaporates and the symptoms return. Soothe is akin to ChapStick in that it provides a lipid barrier surface that helps to lock-in the moisture and provide long-lasting relief. I've been so impressed with Soothe that I now give it to all of my routine post-op cataract patients.
Treatment During the Postop Period
Similar to corneal refractive surgery patients, I believe that all cataract patients should be treated for dry eye syndrome during the postoperative period. This treatment can help to prevent the signs and symptoms of tear film insufficiency and can result in higher patient satisfaction and ocular health.
 |
| Cataract surgery induces ocular inflammation, which may adversely affect patients" tear-film production and stability. Postop medications can cause further ocular irritation and tear-film disruption. |
My current postop regimen is to have the patients use topical fluoroquinolone antibiotics four times per day for one week and topical steroids four times a day for four weeks after surgery. I begin the patient on Soothe emollient topical lubricant at the end of the first week, when the patient is no longer using the topical fluoroquinolone.
For the past year, I have been treating all of my cataract patients with topical dry-eye therapy after their cataract surgery. The results have been impressive, with very few patients complaining of dry eyes or ocular irritation. In addition, I have recently started a study in my own practice to determine the most effective treatment for post-cataract surgery dry eye syndrome.
Refractive Cataract Surgery
With the many recent advances in cataract surgery such as micro-incisions, phaco power modulations, astigmatism correction, precise biometry, and now accommodating, multifocal, and diffracting IOLs, there is little doubt that we are in the age of refractive cataract surgery.
From the patient's perspective, the technology is great, but the bottom line is the quality of the vision and the lack of symptoms. Ensuring a good quality tear film in the postoperative period is instrumental and will likely become the standard of care as it has in corneal refractive surgery.



