Though much time and many dollars have been put into topographic keratoconus indices and instructional courses that teach how to spot keratoconus before LASIK, the diagnosis isn't always obvious. Here, surgeons and researchers familiar with topographic evaluations share their tips and techniques for catching keratoconus, and heading off what could be a LASIK disaster if one were to operate on such a patient.
Catching Keratoconus
Though a comprehensive exam is always the best way to rule out corneal thinning, the experts say there are some topographic clues that can help you in certain cases.
As many know, frank keratoconus appears as a localized area of steepening, usually appearing as a lopsided bow tie. But the diagnosis isn't always straightforward.
"Cones are sometimes subtle," says Houston surgeon Jack Holladay. "The ophthalmologist may see Vogt's striae, which are shear forces or lines that appear in the posterior stroma, but the cones can be very subtle and sometimes hard to see in early cases."
 |
| Figure 1. Pellucid marginal degeneration often takes on a "lobster claw" appearance. |
The first is a steep cornea. "If it's keratoconus, the mean keratometry reading is usually greater than 46 D," Dr. Holladay says. The flatter the K-reading, the more likely it's contact lens warpage.
The second is the location of the hot spot. "In keratoconus, the cone is rarely exactly at 6 o'clock—it's usually at 6:30 or 5:30, that is, slightly to either side of 6 o'clock," he says. "With contact lens warpage, it's almost always at 6 o'clock."
The third criterion is the appearance of the hot spot. In a cone, it is almost circular, but with contact lens warpage the shape looks like a smile or a horizontal ellipse. So, if it's very round, that's another vote for keratoconus. If it's a smile shape, then warpage is more likely.
The fourth parameter is the thickness of the hot spot compared to a symmetrical point above. "If one does not have a tomographer, such as the Bausch & Lomb Orbscan or the Oculus Pentacam, the surgeon can use an ultrasound probe to measure the thickness at the hot spot and then go to the corresponding point above it in the superior cornea that's the same distance from center and measure the thickness there," Dr. Holladay explains. For example, if the hot spot is 3.5 mm inferior at 5 o'clock, then you'd measure at 3.5 mm superior at 11 o'clock.
Dr. Holladay says that, normally, the inferior cornea is no more than 20 µm thinner than the corresponding value of the point above, especially in the afternoon after the patient's been awake for several hours. Since the inferior cornea dries out more in the exposure zone during the day, it's between 10 and 25 µm thinner as the day progresses. If the hot spot is more than 30 µm thinner than the corresponding superior point, then this is another vote for a cone.
Dr. Holladay adds that, in the majority of cases, all four parameters point to the same diagnosis, but occasionally one or two may be different. In these cases, the comparison of the thickness of the "hot spot" to the corresponding area above is key.
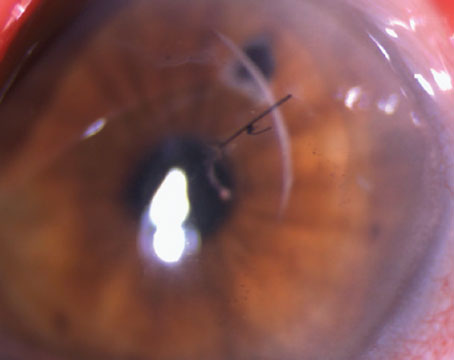
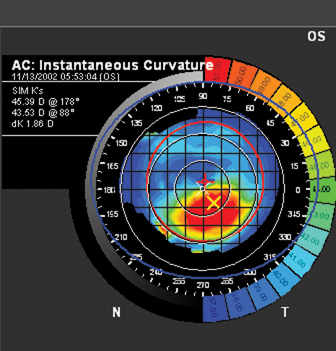 |
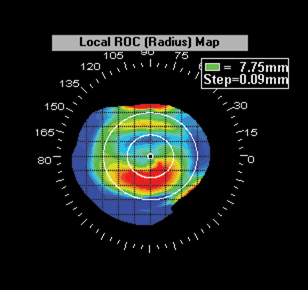 |
| Figure 2. Discerning keratoconus (left) from contact lens warpage (right) can be a challenge. The key is comparing the thickness of the corneal "hot spot" to the thickness in a corresponding area above it. | |
He also says that, just because it's contact lens warpage and not a cone, it doesn't mean the patient's automatically a LASIK candidate.
"In addition to these four criteria, we have found that thinner corneas (450 to 500 µm) are more likely to have contact lens warpage from rigid contact lenses than thicker ones," says Dr. Holladay. "When the criteria for contact lens warpage are present, corneal refractive surgery may still not be indicated because the overall thickness of the cornea may be much thinner than normal."
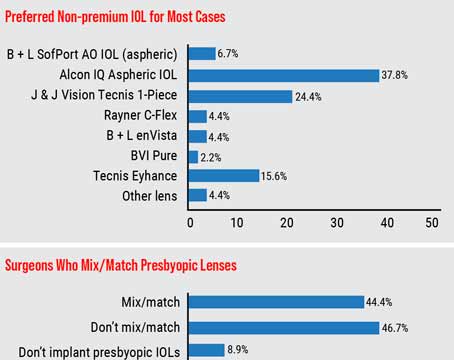
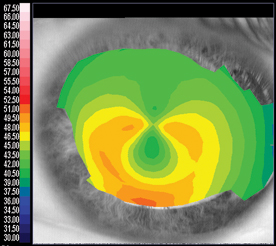
Though keratoconus is the focus of much study, Louisiana State University professor Stephen Klyce, PhD, reminds that pellucid marginal degeneration should also be ruled out. PMD presents topographically as a vertical negative bow tie. On most imagers, the lower half of the bow tie is surrounded by a C or claw-shaped elevation in corneal power (See Figure 1). A third pathology, basement membrane dystrophy (See Figure 3), is harder to discern, since it appears as an amorphous irregularity similar to that caused by a little dry eye or if the patient instilled some drops prior to the topography.
Wavefront may also help in subtle thinning cases.
"There are now correlations with wavefront," says Minnesota refractive surgeon Y. Ralph Chu. "Some suggest that keratoconus is associated with an increase in vertical coma on wavefront. So, if someone has normal corneal thickness but asymmetric topography and more coma, it throws up a red flag."
Equipment Tips
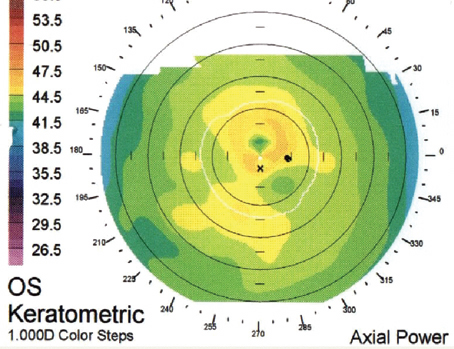
One of the most fundamental steps a surgeon can take to ensure patients with corneal thinning don't get through screening, says Dr. Klyce, is to keep the topographer on a standardized setting for everyone.
He advises to make sure the system isn't adjustable, noting that many systems are. These systems can use an adjustable dioptric or color scale that can "slide around," making it hard to recognize an abnormality because the view the surgeon is using isn't standardized.
Dr. Chu agrees. "It's important to use a consistent scale," says Dr. Chu. "Sometimes an 'auto-size' scale can overly magnify or exaggerate a normality on the cornea into an abnormality."
A machine's color contrast can be important, too.
"Some topographers use a poor choice of hues for representing the power levels," says Dr. Klyce. "This means they have so little contrast between the color intervals that you can't appreciate the irregularities in the corneal surface as well as you can with a good, higher-contrast scale."
In an effort to arrive at a useful, standardized topographic display, Dr. Klyce and his fellow researchers settled upon a scale that uses 1.5-D intervals between contours and axial power displays.
 |
| Figure 3. The general corneal irregularity of basement membrane dystrophy. |
"This kind of a presentation tends to mask features on the corneal surface that aren't of clinical significance," he says, "while, at the same time, it allows those irregularities that are of clinical significance to show up on the display."
Dr. Klyce says that he will evaluate a patient's topography for any surgeon who might need some advice, free of charge. His only proviso is that he can use the topography in his lectures later on, with the patient's identity and personal information masked, of course. He can be reached at sklyce@klyce.com. Dr. Holladay's e-mail address is
holladay@docholladay.com.