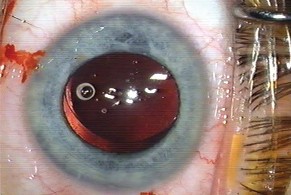
The study analyzed sequential images of 60 eyes taken from the PCO database at St. Thomas' Hospital, London, and included all patients with an AcrySof MA30 lens and a one-year retroillumination image.
The images were divided into those with greater or less than 10 percent PCO area. All images were analyzed to measure the degree of capsulorhexis contact with the anterior IOL surface in clock hours. The data was then grouped into 12 hours of contact, which represented full contact, between 11 and nine clock hours of contact, eight and six, five and three, and two and 0 clock hours of contact, where 0 clock hours represented complete loss of contact.
Twenty-one eyes had more than 10 percent PCO. Forty-eight eyes (80 percent) had some loss of rhexis-IOL contact. These eyes had increased PCO (P <.001) compared with eyes with complete IOL-rhexis contact. More PCO developed when the rhexis was partly on and partly off the IOL. Comparing the presence of PCO with the number of rhexis-IOL contact, as the rhexis contact decreased, the PCO increased (P=.001, r=.56). When the rhexis-IOL contact was further separated into groups of one to three, four to six, seven to nine, and 10 to 12 hours of contact and compared with full contact of the rhexis-IOL, the central two groups with between four and nine clock hours of contact showed a significant increase compared with the other groups where the amount of PCO was less (P=.01).
(Am J Ophthalmol 2005;139:691-694)
Wren S, Spalton D, Jose R, Boyce J, Heatley C.
Glaucoma: Specialists, Patients Share Similar Views
GLAUCOMA SPECIALISTS AND PATIENTS HAVE RELATIVELY similar views on desirable characteristics of eye drops for lowering intraocular pressure and place similar economic value on the cost to improve convenience and side effects. What is not clear from a survey of American Glaucoma Society members is whether the preferences are similar because glaucoma specialists have educated patients to think as they do, or if glaucoma specialists and patients arrived at their preferences independently.
Researchers at Johns Hopkins University correlated demographic data with what they call "willingness to pay" responses, and glaucoma specialists' responses were compared to previously obtained responses from patients. Of the 113 specialists interviewed (30 percent of the 373 members listed in the AGS 2002 Directory), almost all respondents were willing to pay extra to reduce the frequency of administration of eye drops from three times a day to once a day, and to avoid blurred vision, drowsiness, or inhibition of sexual performance (the three most valued characteristics of glaucoma drops as identified by 230 glaucoma patients surveyed). For only one characteristic—iris darkening, did glaucoma specialists seem reluctant to pay more (only 54 respondents or 48 percent were WTP).
The mean amount that respondents were willing to pay (relative to $50) differed significantly across eye drop characteristics (P <0.001.) The mean amount that the respondents were willing to pay was highest for avoidance of inhibition of sexual performance ($105), blurred vision ($92), and drowsiness ($92). Overall, among those who were willing to pay more, for every characteristic, the glaucoma specialists were willing to pay more than the patients. However, after adjusting for age and gender, these differences became quite small and are only statistically significant for characteristics including three times versus once, blurred vision, drowsiness, and sexual performance (99 percent confidence interval not including unity).
(J Glaucoma 2005; 14:151-156)
Jampel, H Parekh, P Johnson, E Robin, A Miller, R.
Study Assesses Best Corneal Incision Location
THE BEST LOCATION FOR CLEAR CORNEAL INCISION ON PATIENTS with preexisting astigmatism may be based on the amount of astigmatism present, according to a Spanish study.
Surgeons at the Hospital Ramón y Cajal, in Madrid, evaluated 574 patients between 1998 and 2003, all of whom proceeded through five stages, with different patients included in each phase (one eye per patient). Each was assigned the following incisions: superior or temporal (n=89), superior (n=141), superior or superior plus relaxing (n=102), nasal or temporal (n=156), and incisions based on applying conclusions of preceding and current studies (n=86). Visual acuity, refraction, biomicroscopy, keratometry and videokeratography were performed on each patient before and after phacoemulsification and intraocular lens implantation. The main outcome measures centered on the corneal refractive and surface regularity index change between preoperative and six-month postoperative examination. Visual acuity was checked at six months.
In patients without corneal astigmatism, corneal changes induced were greater in superior than temporal incision. After superior incision (preoperative steep axis at 90 degrees), a shift of the axis 90 degrees away was less likely with at least 1.5 D of astigmatism. A perpendicular relaxing limbal incision decreased corneal changes. Nasal incision induced greater corneal change than did temporal incision (preoperative steep axis at 180 degrees). A shift of this axis 90 degrees away was more likely with astigmatism < 0.75 D in temporal incision and < 1.25 D in nasal incision.
Based on the findings of the study the researchers conclude that determining the best location for clear corneal incision based on preexisting astigmatism in phacoemulsification depends on the amount of astigmatism present. Superior incision is recommended when there is at least 1.5 D of astigmatism and steep axis at 90 degrees. Temporal incision is recommended with astigmatism < 1.5 D and steep axis at 90 degrees, negligible astigmatism, or astigmatism < 0.75 D and steep axis at 180 degrees. Nasal incision is recommended when there is at least 0.75 D of astigmatism and steep axis at 180 degrees.
(Am J Ophthalmol 2005;139:767-775)
Tejedor, J Murube, J.



