(Unless otherwise stated, none of the studies presented here had any commercial support.)
Corneal Inlays and Lenses
Austrian researchers have amassed two-year data on the implantation of the AcuFocus KAMRA corneal inlay for the treatment of presbyopia. Several of the researchers have either received honoraria from AcuFocus or are employees of the company.
 The prospective study analyzed the implant’s results in 32 naturally emmetropic presbyopes. Over two years, the investigators evaluated bilateral reading acuity, reading distance, reading speed and smallest log-scaled sentence using a standardized testing procedure called the Salzburg Reading Desk.
The prospective study analyzed the implant’s results in 32 naturally emmetropic presbyopes. Over two years, the investigators evaluated bilateral reading acuity, reading distance, reading speed and smallest log-scaled sentence using a standardized testing procedure called the Salzburg Reading Desk.
The researchers say that the SRD results showed a significant improvement in each of the parameters tested. After a mean follow-up period of 24.2 ±0.8 months, the mean reading distance changed from 48.1 ±5.5 cm preop to 38.9 ±6.3 cm postop (p<0.001), the reading acuity “at best distance” improved from 0.3 ±0.14 logRAD (Snellen 20/40) to 0.24 ±0.11 logRAD (slightly worse than 20/32) (p<0.001) and the reading speed increased from 142 ±13 wpm to 149 ±17 wpm (p=0.029). One patient lost one line, and in one patient there was no change at all, while all other patients (30/32) improved up to six log-scaled lines, with a mean improvement of 2.7 ±1.6 lines.847
Researchers from Mexico say hyperopic presbyopes treated with a combination of the ReVision Optics corneal inlay and LASIK get good outcomes. The investigators either consult for or are employed by ReVision Optics.
In the study, 25 hyperopic presbyopes were implanted with ReVision Optics’ 2-mm diameter hydrogel intracorneal inlay and underwent a concurrent LASIK procedure to correct hyperopia. The mean preop sphere was +1.9 D. The Optec 6500 Vision Tester was used to record visual acuities, and a questionnaire was used to gauge the patients’ ability to perform everyday tasks without additional visual aid (there were five tasks for each of three distance ranges).
 In the implanted eye, near uncorrected visual acuity improved in all of the eyes at one month, with an average improvement of seven lines. More than 80 percent of implanted eyes achieved J1 (20/25) or better uncorrected near visual acuity, though none of them could achieve that preoperatively. This level of acuity was maintained at six months (n=11) at which point all patients could read the J1 line binocularly. Intermediate UCVA improved in all of the eyes at one month, by an average of five lines, to an average acuity of 20/25. Only one patient lost distance UCVA (one line) in the implanted eye at a month postop, and the overall improvement averaged two lines. Binocular UCVA was 20/20 or better for all of the patients at both one month and six months postop, improving from an average of 20/40 preop. At one month, 13 of the 15 visual tasks could be performed by all patients with one patient not being able to read distant street signs and two not being able to read medicine labels. By six months, only one patient reported inability to perform one task throughout all distance ranges.5765
In the implanted eye, near uncorrected visual acuity improved in all of the eyes at one month, with an average improvement of seven lines. More than 80 percent of implanted eyes achieved J1 (20/25) or better uncorrected near visual acuity, though none of them could achieve that preoperatively. This level of acuity was maintained at six months (n=11) at which point all patients could read the J1 line binocularly. Intermediate UCVA improved in all of the eyes at one month, by an average of five lines, to an average acuity of 20/25. Only one patient lost distance UCVA (one line) in the implanted eye at a month postop, and the overall improvement averaged two lines. Binocular UCVA was 20/20 or better for all of the patients at both one month and six months postop, improving from an average of 20/40 preop. At one month, 13 of the 15 visual tasks could be performed by all patients with one patient not being able to read distant street signs and two not being able to read medicine labels. By six months, only one patient reported inability to perform one task throughout all distance ranges.5765
A research team from Paris says the Artisan phakic IOL is effective, but that Artisan patients should be watched closely for complications.
Their study was a retrospective look at patients who underwent Artisan implantation between 2000 and 2009, and consisted of 60 eyes of 34 patients, including 52 myopic eyes and eight hyperopes. Fifty-five Verisyse/Artisan and five foldable Artiflex lenses were implanted. Five eyes underwent further keratorefractive surgery (a bioptics procedure) and the mean follow-up was 68 months.
The mean preoperative best spectacle-corrected visual acuity was 0.17 logMAR (a little better than 20/32). The mean postoperative uncorrected visual acuity was 0.32 logMAR (a little worse than 20/40) and the mean postoperative best spectacle-corrected visual acuity was 0.13 logMAR (just below 20/25). In the myopic group, the mean preoperative spherical equivalent was -13.5 D, and the mean postoperative SE was -1.5 D. In the hyperopic group, preoperative SE was +6.75 D and the mean postoperative SE was plano.
 The mean preoperative endothelial cell density was 2,818 cells/mm². At one year postoperatively, the mean endothelial cell density was 2,455 cells/mm² (n=40). The mean change in endothelial cell count from baseline to 68 months was -24 percent. There were no cases of endophthalmitis or glaucoma. Five eyes of three patients underwent explantation of the phakic lens combined with lensectomy. Two eyes presented with a post-op IOL dislocation leading to IOL repositioning and one eye presented with corneal decompensation leading to a corneal graft.5778
The mean preoperative endothelial cell density was 2,818 cells/mm². At one year postoperatively, the mean endothelial cell density was 2,455 cells/mm² (n=40). The mean change in endothelial cell count from baseline to 68 months was -24 percent. There were no cases of endophthalmitis or glaucoma. Five eyes of three patients underwent explantation of the phakic lens combined with lensectomy. Two eyes presented with a post-op IOL dislocation leading to IOL repositioning and one eye presented with corneal decompensation leading to a corneal graft.5778
Femtosecond Findings
Researchers from Mexico say that the new procedure known as refractive lenticule extraction may be as safe and effective as LASIK in myopia and myopic astigmatism. The ReLEx procedure uses the Visumax femtosecond laser (Carl Zeiss Meditec) to create a corneal lenticule that the surgeon then removes through a small incision, also created by the laser.
In the prospective study, researchers treated 10 consecutive patients (20 eyes) who had myopia and myopic astigmatism in which the spherical equivalent between each patient’s eyes was less than 1 D. The right eye of each patient was assigned to ReLEx and the left to conventional LASIK using the CZM Mel 80 excimer laser. Follow-up was done at day one, one week, one month and three months. At the one-month interval an independent blind questionnaire was applied over the telephone to assess patient preference. Statistical analysis was done using the software Statistical Package for the Social Sciences v.13.
The mean preop spherical equivalent in the ReLEx eyes was -3.68 ±1.40 D, and it was -3.61 ±1.58 D in the LASIK group. The difference in postop uncorrected visual acuity at one month wasn’t statistically significant (p=0.54) with half of the eyes achieving 20/20 or better and 90 percent (18 eyes) achieving 20/40 or better in both groups. Fourteen eyes (70 percent) were within 1 D of emmetropia. No eyes lost more than two lines of best-corrected acuity. On the questionnaire, half of the patients (five people) stated they see better with ReLEx and seven patients said they were more comfortable during the surgery and would recommend having ReLEx over conventional LASIK for the correction of myopia and myopic astigmatism.2845
Another group of Mexican researchers looked into the FLEx procedure, or femtosecond lenticule extraction, and say that, though the results are safe and effective, improvements need to be made for the treatment of high astigmatism.
The surgeons analyzed 55 FLEx eyes. The mean preoperative spherical equivalent was -4.57 ±1.64 D. Mean preoperative sphere was -3.67 D (r: 0 to -7.25 D), and mean preoperative cylinder was -1.80 D (r: 0 to -6 D). Preoperative mean uncorrected visual acuity was 1.27 logMAR (worse than 20/200 Snellen), with BSCVA of 0 (20/20) or 0.1 (20/25) logMAR.
Mean postoperative UCVA at one month was 0.20 logMAR (20/32) (p≤0.05), with a SE of +0.019 ±1 D. At three months, two-thirds of the eyes achieved UCVA of 20/20, and all could see 20/40 or better uncorrected. Eighty percent of eyes were within 1 D of emmetropia and two-thirds were within 0.50 D of the intended correction. Two eyes (13.3 percent) lost two or more lines of vision. Optical decentration of the lenticule occurred in one eye.5792
Surgeons from the Private Medical University of Salzburg, Austria, and the University of California in Irvine have amassed preliminary results using the IntraLase iFS femtosecond laser to perform intrastromal arcuate keratotomy.
In this prospective, single-center study, two groups of patients with astigmatism (either naturally occurring or post-cataract surgery) were treated with iFS laser arcuate cuts that were made completely intrastromally on the steep axis. Depending on the amount of astigmatism (treatment goal: 0.75 to 3 D) four different treatment patterns were used, and varied based on the diameter of the zone, the side cut angle and the width of the incision according to the pachymetry values. They followed the patients for a minimum of three months after surgery.
To date, 15 eyes were treated with this method, 13 patients starting with naturally occurring astigmatism and two additional patients with astigmatism following cataract surgery. The surgeons say that the laser system predictably delivered the preselected cut patterns. No perforations occurred and all incisions were placed at the planned locations. The investigators report that the incisions were barely visible by slit-lamp examination at the first postoperative day, but could be detected with optical coherence tomography (Visante, Carl Zeiss Meditec). The reduction of astigmatism was found to be between 0.25 and
2.5 D, and the surgeons say the refractive error and corneal topography were highly stable over time, and that the amount of induced change depended a great deal on the cut angle (between 30 and 150 degrees). Endothelial cell count was found to be unchanged as compared with preoperative values. The surgeons say that their preliminary results show that the procedure has a good safety profile and has the potential for highly precise incision creation and placement.5747
A group of researchers from the Capital University of Medical Science in Beijing found that flaps produced by the IntraLase laser and the Moria One-use Plus SBK microkeratome are very uniform, regular, accurate and reproducible when compared to the Moria M2 Single-use 90-µm head.
In the prospective study, surgeons enrolled 81 patients (161 eyes) and divided them into three groups: IntraLase flaps (59 eyes); Moria One-use Plus SBK flaps (44 eyes) and Moria M2 Single-use 90-µm head flaps (58 eyes).
The researchers say that the flaps created by the IntraLase and the Moria One-use Plus SBK device were more uniform and regular, showing an almost planar configuration, when compared to the “meniscus-shaped” flaps created with the Moria M2 Single-use 90-um head microkeratome. The mean flap thickness of the IntraLase group was 110.81 ±2.26 µm, while the Moria One-use plus SBK and Moria M2 automated groups’ thicknesses were 113.04 ±4.90 µm and 119.87 ±13.64 µm, respectively. For the IntraLase flaps, the average thickness values in the central (111.18 ±3.33 µm), paracentral (111.10 ±2.85 µm) and peripheral (110.34 ±3.42 µm) zones weren’t statistically significantly different (p>0.05). Neither were they statistically significantly different for the Moria One-use Plus SBK flaps (central: 113.85 ±8.07 µm; paracentral: 111.89 ±5.17 µm and peripheral: 113.78 ±4.79 µm; p>0.05). In the Moria M2 Single-Use 90-µm head microkeratome group, the central flap thickness was statistically significantly thinner than the peripheral zone, with a mean flap thickness of 117.96 ±13.14 µm centrally, 117.01 ±13.43 µm paracentrally and 123.11 ±13.77 µm peripherally (p<0.05).
The researchers say that the IntraLase flap and Moria One-use Plus SBK flap thicknesses were statistically significantly more accurate than the Moria M2 Single-Use 90-um head flap thicknesses in the peripheral zone (p<0.05).5787
Surface Ablation
A group of researchers from the Capital University of Medical Science in Beijing found that flaps produced by the IntraLase laser and the Moria One-use Plus SBK microkeratome are very uniform, regular, accurate and reproducible when compared to the Moria M2 Single-use 90-µm head.
In the prospective study, surgeons enrolled 81 patients (161 eyes) and divided them into three groups: IntraLase flaps (59 eyes); Moria One-use Plus SBK flaps (44 eyes) and Moria M2 Single-use 90-µm head flaps (58 eyes).
The researchers say that the flaps created by the IntraLase and the Moria One-use Plus SBK device were more uniform and regular, showing an almost planar configuration, when compared to the “meniscus-shaped” flaps created with the Moria M2 Single-use 90-um head microkeratome. The mean flap thickness of the IntraLase group was 110.81 ±2.26 µm, while the Moria One-use plus SBK and Moria M2 automated groups’ thicknesses were 113.04 ±4.90 µm and 119.87 ±13.64 µm, respectively. For the IntraLase flaps, the average thickness values in the central (111.18 ±3.33 µm), paracentral (111.10 ±2.85 µm) and peripheral (110.34 ±3.42 µm) zones weren’t statistically significantly different (p>0.05). Neither were they statistically significantly different for the Moria One-use Plus SBK flaps (central: 113.85 ±8.07 µm; paracentral: 111.89 ±5.17 µm and peripheral: 113.78 ±4.79 µm; p>0.05). In the Moria M2 Single-Use 90-µm head microkeratome group, the central flap thickness was statistically significantly thinner than the peripheral zone, with a mean flap thickness of 117.96 ±13.14 µm centrally, 117.01 ±13.43 µm paracentrally and 123.11 ±13.77 µm peripherally (p<0.05).
The researchers say that the IntraLase flap and Moria One-use Plus SBK flap thicknesses were statistically significantly more accurate than the Moria M2 Single-Use 90-um head flap thicknesses in the peripheral zone (p<0.05).5787
Surface Ablation
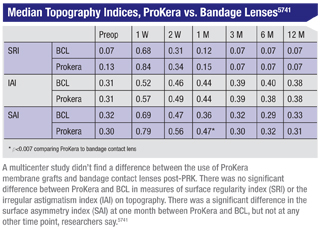
A prospective, non-randomized, controlled trial undertaken by surgeons from several U.S. centers didn’t find an advantage to using the cryopreserved amniotic membrane graft ProKera post-PRK when compared to a bandage contact lens.
The study was composed of 40 patients undergoing PRK at the Walter Reed Center for Refractive Surgery in Washington, D.C. Surgeons created standard 9-mm epithelial defects using a 20%-ethanol solution followed by photoablation using the Alcon/WaveLight Allegretto Wave Eye-Q 400-MHz laser. ProKera was applied on the non-dominant eye after surgery and a high-oxygen transmissible BCL was placed on the dominant eye. The researchers used the following Tomey TMS-4 corneal topography indices to assess optical quality: surface asymmetry index (SAI); surface regularity index (SRI) and irregular astigmatism index (IAI). Corneal haze was also assessed at a week and two weeks and then at one, three, six and 12 months postoperatively. A Wilcoxon signed ranks test was used to compare ProKera to BCL and p<0.007 was considered significant, adjusting for multiple comparisons across seven time points.
The median topography indices of ProKera vs. BCL are listed in the table above. There was no significant difference between ProKera and BCL in measures of SRI or IAI. There was a significant difference in SAI at one month between ProKera and BCL, but not at any other time point. At one month, nine more ProKera eyes had corneal haze than BCL eyes (p=0.002). However, the difference in corneal haze wasn’t significant at other visits.5741
Surgeons affiliated with a large corporate laser center, Optical Express, say that a patient’s past refractive change doesn’t appear to predict his future changes in refraction. They surmised this from an analysis of 252,899 patients (489,982 eyes) whose follow-up visits spanned 6.5 years.
To be included in the study, the patients’ manifest sphere and/or cylinder must have been captured for inclusion, with the initial and most recent visits separated by at least three years. The researchers also analyzed a subset of 15,864 patients (29,213 eyes) with four consecutive exams separated by 12 months (±one month). Using a predictive model, the investigators analyzed the value of past refractive stability in predicting future stability, using the standard of an annual change of no more than 0.5 D in either sphere or cylinder.
The patients’ mean initial myopia was -2.43 D, the mean hyperopia was +2.08 D and the mean cylinder was -0.87 D. Over an average of four years, 71 percent of spherical refractions and 91 percent of cylindrical refractions were stable. On an annualized basis, 95 percent of spherical refractions and 99.6 percent of cylinder refractions were stable, researchers say.
An age-related myopic shift was seen through patients’ late teens, with a smaller percentage shift as patients progressed through age 30.
There was a hyperopic shift in adulthood to age 65, then a myopic shift for those over 65. Most (94 percent) of the patients deemed unstable at a baseline exam subsequently would have been deemed stable at later exam points, while 10 percent of patients deemed stable would subsequently become unstable.
For the subset analysis of eyes with multiple examinations, the majority (94 percent) of eyes that changed by more than 0.50 D in either sphere or cylinder between the first and second exam had subsequent exams (either second to third or third to fourth) where both the sphere and cylinder changed by 0.50 D or less. Similarly, a minority (10 percent) of eyes that changed by 0.50 D or less in both sphere and cylinder between exam one and two had a change of either sphere or cylinder of greater than 0.50 D between either the second to third or third to fourth exams. Young (less than 17 years) and old (greater than 70 years) patients were the most likely to have a consistent and consecutive change in either sphere or cylinder of greater than 0.50 D between each of the four exams.5899
Dr. Probst is national medical director for TLC The Laser Center.




